Sexually Transmitted Infections (STIs)
Subtopic:
Chancroid (Soft Chancre)
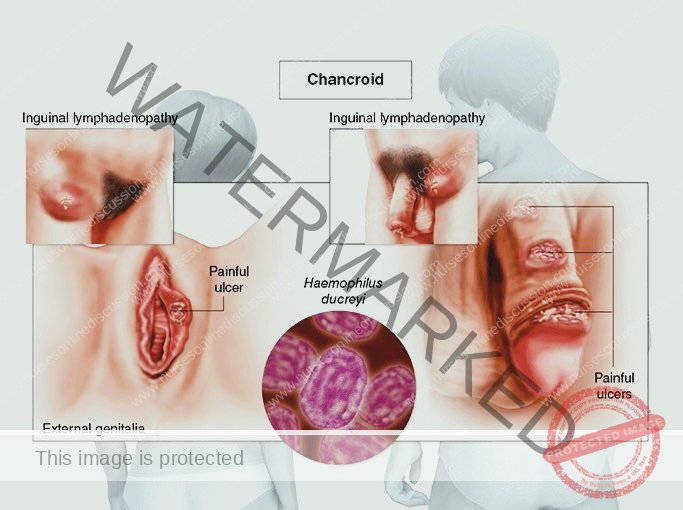
Chancroid is a sexually transmitted infection (STI) characterized by the development of painful, open sores, known as chancroids, typically located in the genital region. This infection frequently leads to swelling and pain in the lymph nodes of the groin.
Incubation period: 2-5 days.
Cause
This STI is caused by the bacterium Haemophilus ducreyi. Transmission primarily occurs through sexual contact.
Risk Factors:
Unprotected sexual encounters: Engaging in sexual activity without barrier methods significantly increases risk.
Multiple sexual partners: Having numerous sexual partners elevates the likelihood of exposure.
Commercial sex work: Sexual contact with sex workers is a recognized risk factor.
Substance misuse: Substance abuse can increase risky sexual behaviors.
Anal sex: Engaging in anal intercourse can facilitate transmission.
Living in endemic regions: Residence in certain developing countries where chancroid is more prevalent increases risk.
Rough sexual activity: Aggressive sexual practices may heighten the risk of transmission.
Signs and Symptoms:
Painful genital ulcer: A small sore, described as a soft chancre, appears on the genitals and is characteristically painful.
Inguinal lymphadenitis: The groin area may exhibit enlargement and inflammation of the lymph nodes, often with pus formation.
Systemic symptoms: Individuals may experience:
Headache
Fever
A general feeling of being unwell (malaise)
Treatment:
Prompt medical treatment is essential and typically involves antibiotics. Effective antibiotic regimens include:
Azithromycin: A single oral dose of 1 gram.
Ceftriaxone: A single intramuscular injection of 250 mg.
Ciprofloxacin: Oral administration of 500 mg twice daily for 3 days.
Erythromycin base: Oral administration of 500 mg three times daily for 7 days.
It is crucial to complete the entire prescribed course of antibiotics to ensure eradication of the infection and prevent complications. Follow-up appointments within 3 to 7 days are recommended to assess treatment response, medication adherence, check for other STIs, and evaluate for potential antibiotic resistance in H. ducreyi.
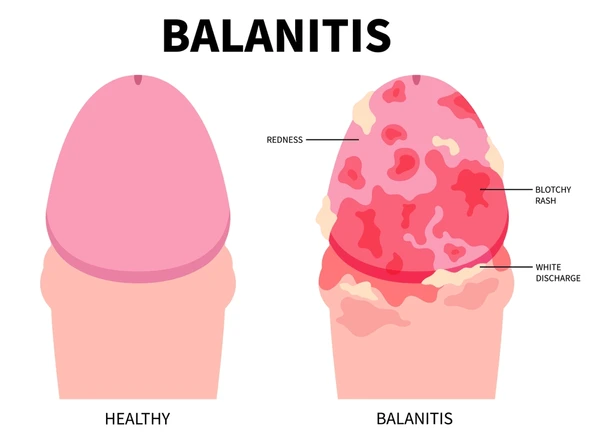
Balanitis
Balanitis is the term used to describe inflammation of the glans penis (the head of the penis). This condition can arise from various causes, with Candida (yeast) being a frequent culprit. Though less common, Trichomonas can also be implicated.
Aetiology (Causes):
The most common cause of balanitis is fungal infection, with Candida species being the most prevalent. In rarer instances, Trichomonas infection can also contribute to inflammation.
Clinical Features (Signs and Symptoms):
Discharge: A noticeable discharge from the penis is often present, indicating infection.
Erythema (Redness): Redness and inflammation of the glans penis are typical signs.
Erosions: Small breaks in the skin (erosions) may be visible on the glans.
Retractile Prepuce: The foreskin (prepuce) is able to be pulled back (retractile).
Management (Treatment):
Effective management of balanitis aims to treat the underlying infection and improve genital hygiene.
Fluconazole 200 mg Stat: A single, one-time dose of Fluconazole is recommended to effectively treat fungal infections like Candida.
Metronidazole 400 mg Every 12 Hours for 7 Days: Metronidazole, taken every 12 hours for a week, is added to provide broader coverage, particularly against certain bacteria that can thrive without oxygen (anaerobic microorganisms).
Hygiene Counselling: Patients should receive advice on proper genital hygiene practices to reduce the chance of future infections.
Circumcision Consideration: Circumcision may be suggested as part of long-term management, as it can potentially decrease the risk of future episodes of balanitis.
Follow-Up Measures (If Condition Persists):
If balanitis does not improve with initial treatment:
Partner Treatment: It’s important to ensure that the patient’s partner also receives appropriate treatment. This is crucial to prevent re-infection and ensure comprehensive care.
Syphilis:
Syphilis is a sexually transmitted infection (STI) caused by the bacterium Treponema pallidum, a spiral-shaped microorganism known as a spirochete. The time from initial infection to the appearance of the first symptom (incubation period) is quite variable, ranging from 2 to 90 days.
Modes of Transmission:
Syphilis is primarily spread through:
Mother-to-Child Transmission (Vertical Transmission): During pregnancy, an infected mother can transmit Treponema pallidum to her unborn child across the placenta. This is known as congenital syphilis and occurs during intrauterine life.
Direct Contact with Infectious Discharges: The bacteria can be transmitted through direct contact with infectious bodily fluids, particularly from syphilis sores.
Sexual Contact (Unprotected Sex): The most common route of transmission is through sexual activities, including vaginal, anal, and oral sex, without the use of barrier protection like condoms with an infected person.
Signs and Symptoms:
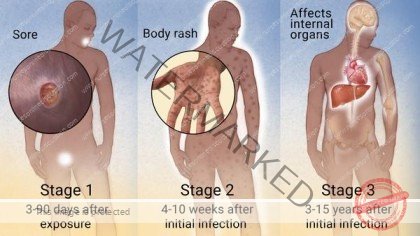
Syphilis progresses through distinct stages if left untreated, each with its own set of characteristic symptoms:
Primary Stage:
Chancre Development: The hallmark of primary syphilis is the appearance of a chancre, a sore or lesion at the site where the bacteria entered the body. This typically occurs 10 to 90 days following initial exposure.
Chancre Characteristics: The chancre is typically described as firm to the touch, painless, and superficial. It has an ulcerated surface and can persist for 4 to 6 weeks. Notably, it will heal spontaneously even without treatment, which can mislead individuals into thinking the infection has resolved.
Painless Lymph Node Swelling (Lymphadenopathy): Painless enlargement of regional lymph nodes may develop in the area near the chancre, usually 1 to 2 weeks after the chancre appears. Because the chancre is often painless and may be in a less noticeable location, this primary stage can easily be missed.
Secondary Stage:
Onset Timing: The secondary stage typically begins 1 to 6 months after the primary infection.
Flu-like Symptoms: Individuals often experience a general feeling of illness, similar to the flu, including mild fever (pyrexia), headache, loss of appetite (anorexia), and sometimes unintentional weight loss.
Generalized Rash: A distinctive reddish-pink rash appears, often described as systemic, meaning it can spread across the body. The rash commonly affects the trunk, limbs (extremities), palms of the hands, soles of the feet, and may also be present around the anus and vagina.
Condylomata Lata: Flat, broad, whitish lesions can develop from the rash areas. These are known as condylomata lata and are highly infectious.
Snail Track Lesions: Greyish-white patches may appear on the tongue, soft palate, and throat. These are sometimes referred to as snail tracks due to their appearance.
Hair Loss (Alopecia): Temporary hair loss (alopecia) can occur during this stage.
Positive Serological Tests: Blood tests for syphilis (serological tests) will be positive at this stage, confirming the infection.
Duration and Latency: The secondary stage can last for up to 9 months. It is followed by a latent period, where outward clinical signs disappear.
Latent Period:
Asymptomatic Phase: This is a period where the infection becomes inactive in terms of outward symptoms. Lesions disappear, and the individual generally feels healthy and well. However, the bacteria remain in the body.
Natural Cure Potential: In some individuals, the body’s immune system may clear the infection during this latent phase, resulting in a natural cure. However, without treatment, the infection can progress to the tertiary stage in many cases.
Tertiary Stage (Late Syphilis):
Late-Stage Manifestations: This stage can develop 1 to 10 years or even longer after the initial infection if left untreated. It affects major organ systems, particularly the cardiovascular system and the nervous system.
Gummatous Syphilis (Gumma Formation): Swelling or tumor-like masses called gummas can develop in various tissues, including the skin, mucous membranes, and bones.
Skin Ulceration: Ulceration of skin gummas can lead to chronic, non-healing ulcers.
Cardiovascular Syphilis: Involvement of the cardiovascular system can result in serious conditions such as:
Aortic aneurysm (bulging of the aorta)
Aortic insufficiency (leaking heart valve)
Coronary artery disease (arteriosclerosis)
Neurosyphilis: Spread to the nervous system can lead to a range of neurological complications, including:
Memory loss
Confusion
Mental disability (dementia)
General paresis of the insane (a historical term for neurosyphilis-induced psychosis)
Other Tertiary Complications: Other potential consequences include:
Joint degeneration
Vision impairment or blindness (failing sight)
Hearing loss or deafness
Diagnosis:
Syphilis is typically diagnosed through blood tests:
VDRL (Venereal Disease Research Laboratory) test: A non-treponemal test used for screening.
RPR (Rapid Plasma Reagin) test: Another non-treponemal test, commonly used to confirm syphilis.
Treponemal Tests: More specific tests like TP-PA ( T. pallidum particle agglutination assay) or FTA-ABS (fluorescent treponemal antibody absorption test) are used to confirm positive results from non-treponemal tests. Historically, Rahmtest and Wasserman tests were also used for syphilis detection.
Treatment:
Penicillin Remains First-Line: Treponema pallidum has not shown significant resistance to penicillin, making it the primary treatment.
Benzathine Penicillin G: The standard treatment is Benzathine benzylpenicillin administered intramuscularly. The dosage and duration depend on the stage of syphilis:
Primary, Secondary, and Early Latent Syphilis: A single dose of 2.4 million units (mu) is typically sufficient.
Late Latent and Tertiary Syphilis: 2.4 million units weekly for 3 weeks may be required.
Erythromycin for Penicillin Allergy: For individuals with a confirmed penicillin allergy, erythromycin is an alternative. A typical regimen is 500mg orally every 6 hours for 2 weeks. Note: Erythromycin is generally less effective than penicillin for neurosyphilis and congenital syphilis.
Partner Treatment: It is crucial to treat all sexual partners of an infected individual to prevent reinfection and further spread.
Follow-up Blood Tests: Treated patients require regular blood tests at 3-month intervals to monitor treatment effectiveness and ensure the infection is cleared.
Prenatal Syphilis Screening: To prevent congenital syphilis and adverse pregnancy outcomes, syphilis testing is recommended for all pregnant women during their first prenatal visit.
Treatment of Infants Born to Syphilitic Mothers: Babies born to mothers diagnosed with or showing signs of syphilis should be treated promptly. Benzathine penicillin is commonly administered at a dose of 50,000 IU as a single intramuscular injection into the thigh (lateral aspect).
Education of Clients:
Patient education is vital for syphilis management and control:
Medication Adherence: Emphasize the importance of drug compliance to ensure treatment success and prevent antibiotic resistance.
Vertical Transmission Risk: Explain the risk of mother-to-child transmission and the importance of prenatal screening and treatment.
Mandatory Treatment: Stress the necessity of completing treatment and attending follow-up appointments.
Partner Management: Promote partner counselling and testing, including HIV testing, as syphilis and HIV co-infection are common.
Prevention Strategies: Advise on abstinence during treatment and correct and consistent condom use to prevent future infections.
Effects of Untreated Syphilis in Pregnancy and Childbirth:
Untreated syphilis in pregnant women can lead to devastating consequences:
Mid-trimester abortion: Spontaneous abortion, typically after 20 weeks of gestation.
Premature labour: Increased risk of preterm birth.
Intrauterine foetal death (IUFD): Stillbirth occurring before delivery.
Intrauterine Growth Restriction (IUGR): Baby’s growth in the uterus is restricted.
Stillbirth (Macerated): Birth of a deceased infant, often showing signs of tissue breakdown (maceration).
Congenital Syphilis: Infant born with syphilis infection, leading to various health problems.
Maternal Complications (Tertiary Syphilis): Pregnant women with untreated syphilis are also at risk of developing the tertiary stage complications, including:
Aortic aneurysm and insufficiency
Memory loss, confusion, mental disability, and general paralysis (neurosyphilis)
Coronary artery stenosis
Joint degeneration, vision impairment, and hearing loss
Basic Facts About STIs:
Sexually transmitted infections (STIs), also known as sexually transmitted diseases (STDs), are infectious conditions caused by various microorganisms. The primary mode of transmission is through sexual contact, typically during unprotected sexual intercourse.
(The table summarizing common STDs, their etiological grouping, and clinical features, which was present in the original notes, is omitted here as per instruction to not include summaries.)
Sexually Transmitted Diseases (STDs) – Key Features and Information
| STD Category | Specific STD | Main Clinical Signs & Symptoms | Causative Pathogen | Incubation Timeline |
| Bacterial STIs | Gonorrhea | Purulent discharge from the urethra or cervix, painful urination (dysuria), increased urinary frequency | Neisseria gonorrhoeae bacterium | 2-6 days |
| Syphilis | Initial presentation: painless, well-defined ulcer (chancre); subsequent symptoms vary based on disease stage | Treponema pallidum spirochete bacterium | 2-4 weeks | |
| Non-gonococcal urethritis/cervicitis | Thin, non-irritating discharge from the cervix or urethra | Chlamydia trachomatis, Mycoplasma hominis, and other microorganisms | 7-14 days | |
| Lymphogranuloma venereum (LGV) | Swollen, painful inguinal lymph nodes (buboes), may present with an ulcer that can be bilateral | Chlamydia trachomatis (specific LGV serovars) | 3-30 days | |
| Granuloma inguinale | Raised, ulcerated lesions with a beefy appearance, typically painless, associated with inguinal lymph node involvement | Klebsiella granulomatis bacterium (formerly Calymmatobacterium granulomatis) | 1-10 weeks | |
| Bacterial vaginosis | Thin vaginal discharge with a distinct fishy odor | Gardnerella vaginalis and other anaerobic bacteria | May be endogenous | |
| Chancroid | Ulcer characterized as dirty and painful, often with underlying tissue involvement | Haemophilus ducreyi bacterium | 1-3 weeks | |
| Viral STIs | Genital Herpes | Recurring episodes of small, multiple, painful ulcers that start as vesicles | Herpes Simplex Virus (HSV) | 2-7 days (initial infection) |
| Hepatitis B virus infection (HBV) | Jaundice (yellowing of skin/eyes) accompanied by inflammation of the liver | Hepatitis B virus (HBV) | Varies | |
| HIV/AIDS | Clinical criteria defined by WHO for AIDS diagnosis; varies widely depending on disease progression | Human Immunodeficiency Virus (HIV) | Months – 10 years or more | |
| Venereal warts/HPV | Finger-like or flat growths on the genital areas | Human Papillomavirus (HPV) | Weeks-months | |
| Fungal STIs | Genital candidiasis | White, curd-like vaginal discharge coating vaginal walls, causing itching, soreness, and potential excoriation or small cuts | Candida albicans fungus | May be endogenous and recurrent |
| Ringworm (fungal) | Patches of reduced or increased pigmentation (hypo/hyperpigmentation) in the pubic region | Tinea species of fungi | Varies | |
| Protozoal STI | Trichomoniasis | Greenish, itchy vaginal discharge with a foul smell | Trichomonas vaginalis protozoan | Variable |
| Other STIs | Scabies | Vesicles containing mites in the pubic region, intense itching | Sarcoptes scabiei mite | Approximately 30 days |
| Pediculosis (Vermin) | Presence of nits (lice eggs) in pubic hair, itching in the pubic area | Pthirus pubis (pubic lice) | 7 – 10 Days |
Risk Factors for STI/STDs:
Several influential factors contribute to the prevalence of Sexually Transmitted Infections (STIs) in Uganda. These include:
Multiple Sexual Partners: An increased number of sexual partners directly raises the chances of both contracting and spreading STIs. Each new partner introduces potential exposure.
Inconsistent or Absent Condom Use: When condoms are not used regularly or correctly during sexual activity, the protective barrier against STI transmission is removed, significantly increasing susceptibility.
Lack of Male Circumcision: Studies suggest that the absence of circumcision in men can be associated with a higher risk of STI transmission in certain populations.
Alcohol and Drug Consumption: The use of alcohol and drugs can negatively impact sexual health decisions. Alcohol, in particular, can impair judgment, leading to less careful partner selection, reduced inhibitions concerning safe sex, and difficulties in negotiating or correctly using condoms.
Early Initiation of Sexual Activity: Starting sexual intercourse at a younger age is linked to a greater likelihood of acquiring STIs throughout life, as it increases the duration of potential exposure and may be associated with less health knowledge or access to care.
Socio-Cultural Norms, Including Early Marriage: Cultural practices and societal norms, such as the prevalence of early marriage, can contribute to STI spread by influencing sexual behaviours and access to information or services.
Economic Hardship, Especially Poverty: Poverty creates significant barriers to STI prevention and care. Limited financial resources can restrict access to condoms, testing, treatment, and essential health education.
Gender Imbalances and Limited Female Agency: In situations where women have less power in sexual relationships, including limited ability to negotiate safer sex practices, their risk of STI exposure is elevated.
Legal and Human Rights Constraints, Stigma, and Discrimination: Laws, policies, stigma, and discrimination against certain groups, such as sex workers, can undermine effective STI prevention and control efforts by hindering access to services and creating barriers to care.
Unequal Access to Social and Healthcare Services: Disparities in access to social support systems and quality healthcare services amplify the risk of STIs, creating a situation where vulnerable populations face disproportionate burdens and reduced opportunities for prevention and treatment.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

