Manage of Women with Gynaecological Conditions
Subtopic:
Dysfunctional uterine bleeding
Dysfunctional uterine bleeding (DUB) is characterized by irregular uterine bleeding when no identifiable structural or systemic medical issues are present. It manifests as menstrual bleeding that is inconsistent, prolonged, or excessively heavy. Essentially, DUB describes abnormal bleeding stemming from hormonal imbalances rather than from specific physical causes like injury, infection, pregnancy complications, or growths.
Related Factors in Dysfunctional Uterine Bleeding
While no distinct physical or organic cause is evident in DUB, the term “dysfunctional” indicates that the bleeding originates from disruptions in the usual hormonal control of the menstrual cycle, rather than a clear anatomical problem. The following factors are not direct causes but can influence or worsen DUB:
Hormonal Imbalance: Disruptions in hormone levels, specifically oestrogen and progesterone, are key factors. These imbalances can disturb the normal rhythm of the menstrual cycle. These disruptions can arise from various sources, including:
Stressful conditions
Underlying health problems
Natural shifts in hormone production
Non-Cancerous and Cancerous Growths: The presence of both benign (non-cancerous) growths, such as uterine fibroids, and malignant (cancerous) growths, like uterine or cervical cancer, can trigger abnormal bleeding patterns. Growths can alter the structure of the uterus, disrupting the regularity of menstruation.
Contraceptive Use: Certain types of birth control, particularly hormone-containing contraceptives, can affect menstrual patterns. Changes in the type or dosage of contraceptives may contribute to dysfunctional bleeding in some individuals.
Blood Clotting Issues: Disorders that affect the body’s ability to clot blood, such as thrombocytopenia or leukaemia, can lead to DUB. When blood clotting is impaired, it can result in menstrual flow that is both irregular and excessively heavy.
Systemic Illnesses – Ovarian Insufficiency: Ovarian failure or insufficiency, marked by the loss of normal ovarian function, can upset hormonal balance and menstrual regularity. Systemic diseases impacting how the ovaries function can contribute to dysfunctional bleeding.
Varied Influences on Hormonal Equilibrium: Numerous elements can impact hormonal balance and subsequently contribute to DUB:
Immature Hypothalamus: In adolescents, the hypothalamus (brain region regulating hormones) may not be fully mature, leading to hormonal fluctuations.
Changes in Exercise Routine: Significant alterations in exercise habits can affect hormonal balance.
Impaired Follicular Stimulation: Issues with the stimulation of ovarian follicles (where eggs mature) can disrupt normal hormone production.
Nutritional Deficiencies: Poor nutrition or malnutrition can impact hormone regulation.
Emotional Stress/Crises: Emotional factors and crises can significantly influence hormonal balance.
Temporary Oestrogen Drop at Ovulation: A natural, temporary decrease in oestrogen levels around ovulation can sometimes trigger bleeding irregularities.
Radiation and Chemotherapy Treatments: These cancer treatments can affect hormone production and menstrual cycles.
Lifestyle Modifications: Major lifestyle changes can sometimes impact hormonal balance and menstrual patterns.
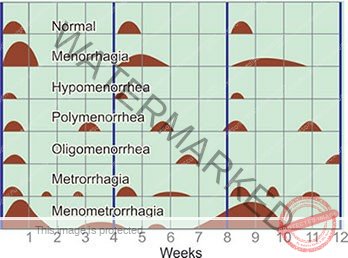
Forms of Dysfunctional Uterine Bleeding (DUB):
DUB can manifest in several distinct patterns of abnormal uterine bleeding:
Menorrhagia (Heavy or Prolonged Menstrual Bleeding): This type involves menstrual periods characterized by unusually heavy flow or extended duration, occurring during regular menstrual cycles. Essentially, it’s excessively heavy or long periods at the expected times.
Metrorrhagia (Bleeding Between Periods): This refers to vaginal bleeding that occurs at any point in between regular, expected menstrual periods. It’s characterized by bleeding that is not associated with menstruation.
Oligomenorrhea (Infrequent Menstruation): This is marked by significantly reduced menstrual flow, often accompanied by cycles that are much longer than normal or irregular in their timing. It indicates sparse and often irregular periods.
Polymenorrhea (Frequent Menstruation): This form is characterized by menstruation that occurs too frequently, specifically at intervals of less than three weeks. It’s defined by periods that are too close together.
Menometrorrhagia (Irregular and Excessive Bleeding): This involves a combination of prolonged and heavy bleeding that occurs both during expected menstrual times and also at unpredictable intervals between periods. It’s a mix of heavy, prolonged, and irregular bleeding.
Signs and Symptoms of Dysfunctional Uterine Bleeding:
Irregular Menstrual Cycles: Periods may become unpredictable, occurring more often or less often than what is typical for the individual. This reflects the hormonal imbalance affecting cycle regularity.
Prolonged Bleeding Episodes: Menstrual bleeding may last for an extended number of days, exceeding the typical duration for that person. This is due to the uterine lining shedding for longer than normal.
Heavy Menstrual Flow: Bleeding during menstruation may be excessively heavy, requiring frequent changes of sanitary protection and potentially impacting daily activities. This is a result of increased shedding of the uterine lining.
Bleeding Between Periods (Intermenstrual Bleeding): Spotting or bleeding can occur at times outside of the expected menstrual period. This is often due to hormonal fluctuations affecting the uterine lining’s stability.
Fatigue and Weakness: Excessive blood loss can lead to feelings of tiredness, fatigue, and reduced energy levels. This is a direct consequence of reduced red blood cells and iron deficiency.
Symptoms of Anaemia: Individuals may experience signs of anaemia such as general weakness, dizziness or lightheadedness, shortness of breath upon exertion, or unusually pale skin. These are all indicators of reduced oxygen-carrying capacity in the blood due to blood loss.
IMPORTANT NOTE: Dysfunctional uterine bleeding is diagnosed only after ruling out all other potential medical conditions or structural abnormalities that could be causing the abnormal bleeding. It is a diagnosis of exclusion.
Diagnostic Investigations:
Diagnosis of dysfunctional uterine bleeding relies on a combination of clinical assessment and laboratory tests:
Complete Blood Count (CBC): This blood test is crucial to check for anaemia by measuring red blood cell levels and haemoglobin. Anaemia can be a consequence of prolonged or heavy bleeding.
Human Chorionic Gonadotropin Test (hCG Test): A pregnancy test is essential to eliminate pregnancy as a cause of uterine bleeding, as bleeding in early pregnancy can be mistaken for menstrual irregularities.
Thyroid Stimulating Hormone (TSH) Measurement: This blood test is performed to assess thyroid function. Elevated TSH levels might indicate hypothyroidism, which can sometimes contribute to menstrual irregularities.
Prolactin Level Measurement: Measuring prolactin levels helps to exclude a pituitary adenoma (a benign tumour of the pituitary gland) as a possible cause, as these tumours can affect hormone balance and menstrual cycles.
Pelvic Ultrasound: This imaging technique is used to visualize the uterus and ovaries, helping to rule out structural issues such as fibroids, polyps, or ovarian cysts that could be causing abnormal bleeding.
MANAGEMENT OF D.U.B.
Treatment strategies for dysfunctional uterine bleeding are tailored to the individual, taking into account factors such as age, the condition of the uterine lining, and future pregnancy plans.
When the uterine lining is found to be thickened but composed of normal cells (without hyperplasia or malignancy), management of heavy bleeding may involve:
High-Dose Hormonal Therapy: Initially, a high dose of combined oral contraceptives (COCs) containing both oestrogen and progestin, or in some cases, oestrogen alone (often intravenously in severe cases), may be administered to rapidly control heavy bleeding. This is usually followed by oral progestin. This approach aims to quickly stabilize the uterine lining and stop excessive bleeding.
Maintenance with Low-Dose Oral Contraceptives: Once the bleeding is controlled (typically within 12 to 24 hours), a regimen of low-dose oral contraceptives is often prescribed for at least three months. This helps to regulate the menstrual cycle and prevent recurrence of abnormal bleeding. For women with less severe bleeding initially, lower doses of oral contraceptives may be started from the outset.
Progestin-Only Therapy (for Oestrogen Contraindications): If a woman has medical reasons that prevent the use of oestrogen-containing medications, progestin-only pills may be prescribed. These are typically taken orally for 10 to 14 days each month to help regulate the cycle and manage bleeding.
Other medication options may include: (further details on specific medications would typically follow in comprehensive notes).
| Class of Drug | Example | Remarks |
| NSAIDs | Mefenamic acid 500mg, Ibuprofen 400-800mg | Reduces menstrual blood loss by lowering prostaglandin concentration; Should be taken before and during menstruation. |
| Antifibrinolytics | Tranexamic acid 1g twice daily | Helps prevent blood loss during menstruation. |
| Hormonal Contraceptives | Combined Oral Contraceptives or IUDs | Controls chronic bleeding by suppressing the endometrium. |
| Progesterone Therapy | Norethisterone 5mg twice daily from day 5-26 of menstrual cycle | Helps stop acute bleeding. |
- Total hysterectomy is indicated if the woman is over 35 years, uterine lining thickened and contains abnormal cells and she does not want to become pregnant.
- D&C may be used if response or hormonal therapy proves ineffective.
- If a woman wants to become pregnant, clomiphene drugs may be given orally to induce ovulation.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

