Manage of Women with Gynaecological Conditions
Subtopic:
Introduction to Gynaecology

Gynaecology is the specialized field of medical science dedicated to the health and diseases of the female reproductive system.
OVERVIEW OF ANATOMY AND PHYSIOLOGY OF THE FEMALE REPRODUCTIVE SYSTEM
The female reproductive system is intricately designed and encompasses several key components working in harmony. These are broadly classified into: the external genitalia, the internal genitalia, and the mammary glands.
EXTERNAL GENITALIA
The external female genitalia, commonly referred to as the vulva, is a multifaceted anatomical region. It is comprised of distinct structures, each contributing to specific functions and exhibiting unique characteristics.
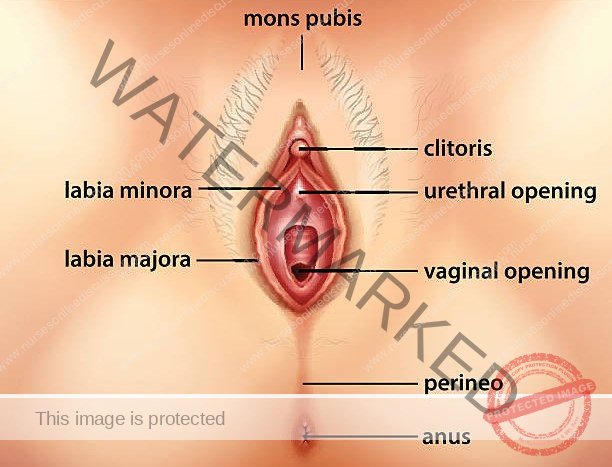
Mons Pubis: This is the rounded, fatty eminence situated anteriorly over the pubic symphysis. Post-pubertally, it becomes covered in pubic hair. Its primary function is to provide cushioning and protection to the pubic bone, particularly during sexual activity.
Labia Majora: These are two prominent, longitudinal folds of skin and adipose tissue extending inferiorly from the mons pubis to merge posteriorly at the perineum. Acting as the outer protective folds of the vulva, they shield the more delicate internal structures. Their volume may decrease with age or following childbirth.
Labia Minora: Located within the labia majora, these are two smaller, more delicate, and pigmented folds of skin. They encircle the vestibule, encompassing the urethral and vaginal openings. Rich in sebaceous and sweat glands, they contribute to lubrication and moisture. Composed of erectile tissue, the labia minora become engorged with blood during sexual stimulation, heightening sensitivity to touch.
Clitoris: This is a highly specialized, erectile and sensitive organ positioned at the anterior apex of the vulva, partially concealed by the anterior junction of the labia minora. Homologous to the penis in males, it is the primary centre for female sexual pleasure. During sexual arousal, it becomes engorged with blood and acutely sensitive to tactile stimulation.
Vestibule: This is the almond-shaped area or cleft enclosed by the labia minora. It serves as the entryway and contains the external openings of both the urethra (urinary meatus) and the vagina (vaginal introitus).
Vaginal Opening (Introitus): Situated within the vestibule, this is the external orifice leading into the vagina. In many individuals, the vaginal opening is partially occluded by the hymen, a membranous fold of tissue.
Functions of the Vulva:
Protection: The labia majora serve as an external barrier, safeguarding the internal reproductive organs from external trauma and potential pathogens.
Sexual Sensation: The clitoris and the abundant nerve endings within the labia minora are critical for sexual arousal, responsiveness and pleasure.
Reproductive Role: The vaginal opening facilitates penile-vaginal intercourse and acts as the passageway for the fetus during parturition.
Urinary Function: The urethral opening within the vestibule allows for the expulsion of urine from the urinary bladder.
Lubrication and Moisturization: Numerous glands in the vulvar region secrete fluids, maintaining local moisture and lubrication for comfort and function.
Parturition: During childbirth, the tissues of the vulva and vaginal opening are designed to distend significantly to allow for the passage of the neonate.
INTERNAL GENITALIA
The internal female reproductive organs, located within the pelvic cavity, consist of the vagina, cervix, uterus, fallopian tubes, and ovaries.
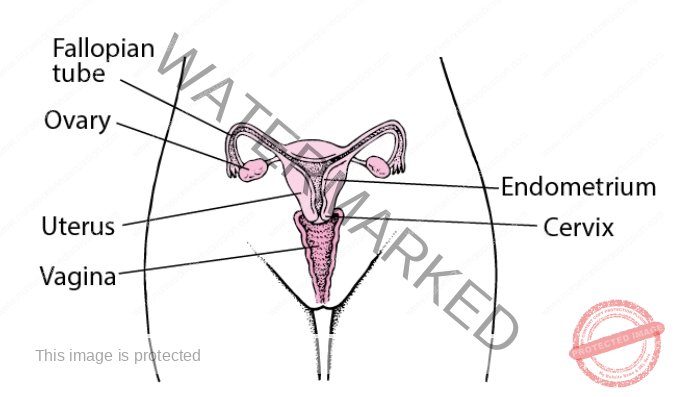
Vagina: The vagina is a muscular, tube-like canal that extends internally from the vulvar vestibule to the cervix. Approximately 10 centimetres in length in its resting state, it possesses remarkable elasticity, capable of significant expansion, particularly during childbirth. The vaginal mucosa secretes fluids that play a crucial role in maintaining cleanliness and a naturally acidic pH within the vaginal environment. The vaginal opening may be partially covered by the hymen, a membrane which typically ruptures during initial penetrative sexual activity.
Functions of the Vagina:
Serves as the exit pathway for menstrual blood and associated fluids during menstruation.
Acts as the conduit through which sperm ascend towards the fallopian tubes.
Functions as the receptive organ for the penis and semen deposition during sexual intercourse.
Forms the birth canal, facilitating the passage of the foetus during vaginal delivery.
Cervix: The cervix represents the lowermost segment of the uterus, projecting into the upper aspect of the vaginal canal. It establishes the connection between the uterus and the vagina, serving as a passage for menstrual flow, sperm, and the neonate during birth.
The cervix is anatomically divided into two primary regions:
The ectocervix: This is the outer portion of the cervix, readily visible during a standard gynaecological examination.
The endocervix: This refers to the cervical canal, a tunnel-like passageway that traverses the cervix, connecting the ectocervix to the uterine cavity.
Cervical Dynamics during Childbirth: The cervix undergoes significant transformations during labour and delivery. It softens considerably and progressively dilates (opens) to permit the passage of the foetus. Cervical dilation is a key indicator of the onset and progression of labour.
Uterus: The uterus is a pear-shaped, muscular organ situated within the female pelvis, positioned posterior-superior to the urinary bladder and anterior to the rectum. Anatomically, it is divided into three main parts: the fundus (the rounded upper portion), the body (the main central section), and the cervix (the lower constricted segment). The uterine wall itself is composed of three distinct layers: the endometrium (the inner mucosal lining), the myometrium (the thick middle layer consisting of smooth muscle), and the perimetrium (the outer serosal layer).
Functions of the Uterus:
Primary site of menstruation: The endometrium undergoes cyclical shedding and regeneration, resulting in monthly menstrual bleeding.
Gestational housing: The uterine cavity provides the space and environment for foetal development throughout pregnancy.
Labour and Delivery: The powerful uterine myometrium generates coordinated contractions during labour, which are essential for expelling the infant through the birth canal.
Fallopian Tubes: Also known as oviducts or uterine tubes (salpinges), the fallopian tubes are paired tubular structures, each approximately 10 cm in length. They extend laterally from the uterine fundus towards the pelvic sidewalls, positioned near the ovaries. Each fallopian tube is further subdivided into four sections: the infundibulum (the funnel-shaped distal end, featuring fimbriae – finger-like projections near the ovary), the ampulla (the widest and longest portion), the isthmus (the narrower segment closest to the uterus), and the interstitial (or intramural) part, which traverses the uterine wall and opens into the uterine cavity.
Functions of the Fallopian Tubes:
Sperm and Ovum Transport: The fallopian tubes facilitate the transport of sperm towards the ovary and, conversely, the ovum (egg) from the ovary towards the uterus. This transport is aided by the action of cilia (tiny hair-like projections) lining the tubal epithelium and muscular contractions of the tubal wall.
Fertilization Site: The ampulla of the fallopian tube is the usual site of fertilization, where sperm and ovum typically unite.
Zygote Nourishment and Transport: The fallopian tubes provide a nourishing environment for the fertilized ovum (zygote) and guide its movement towards the uterine cavity for implantation.
Ovaries: The ovaries are paired, almond-shaped glands situated on either side of the uterus within the pelvic cavity. They are connected to the uterus via the ovarian ligament and to the pelvic sidewall by the suspensory ligament of the ovary. The ovary is partially covered by the mesovarium, a fold of the broad ligament. The size of the ovary varies throughout a woman’s life, changing with age and stage of the menstrual cycle.
Ovarian Functions:
Ovum (Egg) Production: The ovaries are responsible for the production and release of ova (eggs) through the process of ovulation, essential for reproduction.
Female Sex Hormone Synthesis: The ovaries are the primary source of female sex hormones, principally oestrogen and progesterone.
Oestrogen: This hormone plays a pivotal role in the development and maintenance of female secondary sexual characteristics, promotes overall growth and development, and is crucial for the maturation of the reproductive organs.
Progesterone: Progesterone primarily prepares the endometrium for potential pregnancy by making it receptive to implantation. It also contributes to placental development, breast enlargement during pregnancy, and exerts a negative feedback effect to inhibit further ovum production during gestation.
Menstrual Cycle Regulation: Oestrogen and progesterone act synergistically to regulate the cyclical changes in the endometrium that characterize the menstrual cycle.
COMMON TERMS IN GYNAECOLOGY
Menarche: Menarche signifies the onset of menstruation, marking a girl’s first menstrual period. It is a significant developmental milestone, considered an initial indicator of puberty and the potential for future fertility. The average age of menarche typically occurs between 12 and 13 years.
Precocious Puberty: This term describes the abnormally early onset of puberty, defined as the commencement of menstruation before the age of 8 in girls, or the development of secondary sexual characteristics before age 9 in boys. Precocious puberty is an endocrine abnormality that necessitates medical investigation to determine the underlying cause.
Menorrhagia: Menorrhagia refers to abnormally heavy or prolonged menstrual bleeding. Clinically, it is often defined as menstrual blood loss exceeding 80 millilitres per cycle, or bleeding that lasts longer than 7 days. It is relatively common during adolescence and the perimenopausal transition. Potential causes of menorrhagia include abnormal blood clotting disorders, disruptions in the normal hormonal regulation of the menstrual cycle, or various endometrial pathologies.
Oligomenorrhoea: Oligomenorrhoea describes a condition characterized by infrequent or very light menstrual periods, typically occurring at intervals exceeding 35 days.
Post-Coital Bleeding: Post-coital bleeding is defined as any vaginal bleeding that occurs after sexual intercourse. It is always considered abnormal and requires medical evaluation to determine the cause.
COMMON CAUSES OF GYNAECOLOGICAL ISSUES
Congenital Anomalies:
Examples: Absence or malformation of the vagina, ovaries, uterus, or incomplete fusion of the uterus (uterine didelphys, bicornuate uterus).
Description: These are structural abnormalities of the reproductive organs that are present from birth, resulting from developmental errors during embryogenesis.
Environmental Factors:
Physical and Psychological Well-being: Chronic stress, anxiety, and mental health conditions can significantly impact the hypothalamic-pituitary-ovarian axis, leading to menstrual irregularities or even amenorrhoea (absence of menstruation).
Lifestyle Choices: Unhealthy lifestyle factors such as poor diet, excessive alcohol consumption, smoking, substance abuse, sedentary behaviour, and exposure to environmental toxins can negatively affect reproductive health and hormonal balance.
Pathogenic Agents (Infections):
Infections: Entry and proliferation of pathogenic microorganisms (bacteria, viruses, fungi, parasites) can cause various infections within the female reproductive tract.
Examples: Vaginitis (vaginal infection), vulvitis (vulvar infection), cervicitis (cervical infection), endometritis (uterine lining infection), salpingitis (fallopian tube infection), pelvic inflammatory disease (PID).
Inflammatory Conditions: Infections trigger inflammatory responses that can disrupt normal reproductive function and cause tissue damage.
Trauma:
Instrumental Trauma: Iatrogenic injuries caused by medical instruments during gynaecological procedures (e.g., surgery, childbirth interventions), which can potentially lead to complications such as fistula formation (abnormal connections between organs).
Accidental Trauma: Physical injuries to the genital organs resulting from accidents, falls, assaults, or other forms of trauma.
Hormonal Imbalances:
Endocrine Disorders: Various conditions affecting the endocrine system (hormone-producing glands) can disrupt hormonal balance and impact reproductive function. Examples include thyroid disorders, adrenal disorders, and pituitary gland abnormalities.
Polycystic Ovary Syndrome (PCOS): A common endocrine disorder characterized by hormonal imbalances, particularly elevated androgens, leading to ovarian dysfunction, menstrual irregularities, and other symptoms.
Reproductive System Disorders:
Endometriosis: A condition where tissue similar to the uterine lining (endometrium) grows outside the uterus, causing pelvic pain, dysmenorrhea (painful periods), and fertility problems.
Uterine Fibroids (Leiomyomas): Benign (non-cancerous) tumours of the uterine smooth muscle, which can cause heavy bleeding, pelvic pressure, and fertility issues.
Pelvic Inflammatory Disease (PID): An infection of the female pelvic organs, often caused by sexually transmitted infections, which can lead to chronic pelvic pain, infertility, and ectopic pregnancy.
Menstrual Disorders:
Dysmenorrhoea: Painful menstruation, often characterized by cramping pelvic pain before or during periods.
Menorrhagia: Heavy menstrual bleeding (as defined above).
Amenorrhoea: Absence of menstruation, which can be primary (never having started) or secondary (periods stopping after previously regular cycles).
Gynaecological Cancers:
Types: Cancers affecting the female reproductive organs, including cervical cancer, ovarian cancer, uterine (endometrial) cancer, vaginal cancer, and vulvar cancer.
Importance of Screening: Regular gynaecological screenings (e.g., Pap smears, pelvic exams) and early detection are crucial for improving outcomes in gynaecological cancers.
Pregnancy-Related Complications:
Ectopic Pregnancy: A pregnancy where the fertilized egg implants and develops outside the uterus, most commonly in a fallopian tube, which is a life-threatening condition.
Gestational Trophoblastic Disease (GTD): A group of conditions involving abnormal growth of cells that normally would develop into the placenta during pregnancy.
Pelvic Floor Disorders:
Pelvic Organ Prolapse: Descent or herniation of pelvic organs (bladder, uterus, rectum) into the vagina due to weakening of pelvic floor support structures.
Incontinence: Involuntary loss of bladder control (urinary incontinence) or bowel control (faecal incontinence) due to pelvic floor dysfunction.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

