Manage of Women with Gynaecological Conditions
Subtopic:
Menstrual disorders
Menstrual disorders are irregularities or problems related to a woman’s monthly menstruation during her reproductive years.
Common menstruation-related disorders include:
Amenorrhea: Absence of menstruation.
Dysmenorrhea: Painful menstruation or menstrual cramps.
Menorrhagia: Abnormally heavy or prolonged menstrual bleeding.
Metrorrhagia: Bleeding between menstrual periods.
Polymenorrhagia (Epimenorrhea): Menstrual cycles that occur too frequently.
Dysfunctional Uterine Bleeding (DUB): Abnormal uterine bleeding due to hormonal imbalances, not linked to structural issues.
Endometriosis: A condition where tissue similar to the uterine lining grows outside the uterus.
MENSTRUATION
Menstruation, commonly known as a period, is the regular, natural process where blood and tissue are discharged from the uterus through the vagina.
A typical menstrual period generally lasts between 2 to 7 days, with a normal total blood loss ranging from approximately 10 to 80 milliliters.
A healthy menstrual cycle usually spans from 21 to 35 days in length, counted from the first day of one period to the first day of the next.
THE MENSTRUAL CYCLE
The menstrual cycle is a recurring series of biological changes that happen in a woman’s body, typically about every 28 days, from puberty until menopause.
These cyclical events are controlled by hormones. Key hormones involved are produced by the pituitary gland in the brain (Follicle-Stimulating Hormone – FSH and Luteinizing Hormone – LH) and the ovaries (Progesterone and Estrogen). These hormones work together to regulate the cycle.
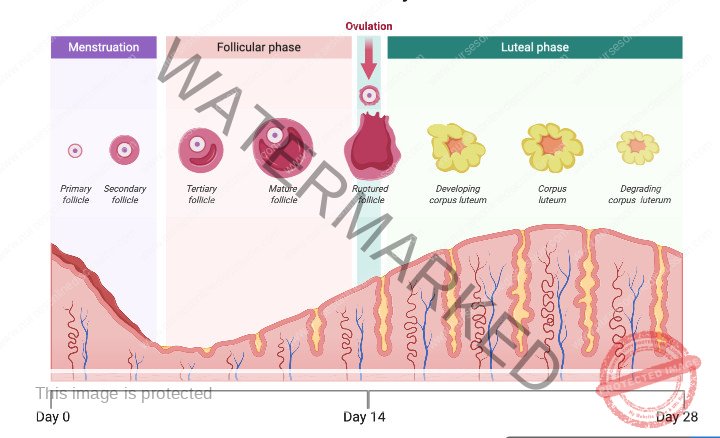
The Menstrual Cycle Phases
The menstrual cycle is typically divided into three main phases:
Follicular Phase (Proliferative Phase)
This phase starts with menstruation.
Menstrual bleeding occurs because estrogen and progesterone levels drop from the previous luteal phase.
This hormonal decrease triggers the shedding of the uterine lining (endometrium), resulting in menstrual flow.
During this phase, the follicle-stimulating hormone (FSH), released from the pituitary gland, increases.
FSH stimulates the development of multiple follicles in the ovaries, each containing an egg (ovum).
As the follicular phase progresses, FSH levels naturally decline, usually leading to one follicle becoming dominant.
This dominant follicle matures and starts producing estrogen.
Ovulatory Phase
This phase is initiated by a significant surge in luteinizing hormone (LH), accompanied by a smaller rise in FSH.
The LH surge is the primary trigger for ovulation, typically occurring around the 14th day of a 28-day cycle, but can vary depending on individual cycle length (generally between day 7 and 21).
Estrogen levels reach their peak just before ovulation.
Progesterone levels start to increase after the egg is released from the dominant follicle.
The remaining part of the dominant follicle after ovulation transforms into the corpus luteum, which becomes the main producer of progesterone.
Luteal Phase (Secretory Phase)
The luteal phase begins right after ovulation.
In this phase, the endometrium thickens further, preparing to nourish a fertilized egg if pregnancy occurs.
If fertilization does not happen, the rising levels of estrogen and progesterone exert negative feedback, reducing the production of both LH and FSH from the pituitary gland.
Since the corpus luteum needs LH to survive and function, the decrease in LH causes the corpus luteum to break down (atrophy).
This breakdown leads to a drop in estrogen and progesterone production.
The thickened uterine lining, no longer supported by high hormone levels, begins to shed, marking the start of menstruation.
The cycle then begins again with the follicular phase, completing the menstrual cycle.

Factors that May Interfere with the Menstrual Cycle, Leading to Menstrual Disorders
Physical Health Issues: Conditions like injuries, growths (tumors), and illnesses affecting glands, ovaries, or the uterus can disrupt the normal operation of the reproductive system, potentially causing menstrual irregularities.
Chronic Illnesses: Weakening diseases such as tuberculosis (TB) and HIV/AIDS can compromise overall health, which may in turn disturb the regular menstrual cycle.
Poor Nutrition: Inadequate nutrition or malnutrition can create imbalances in hormones, impacting the consistency and regularity of menstrual periods.
Dysfunctional Uterine Bleeding (DUB): Abnormal bleeding from the uterus, characterized by irregular patterns, can itself be a factor contributing to various menstrual disorders.
Age at Menarche: Menstrual cycles can be unpredictable in younger individuals shortly after menarche (the start of menstruation) as their hormonal systems are still maturing.
Pregnancy and Related Complications: Pregnancy naturally halts menstruation, and issues arising during pregnancy can lead to disruptions or irregularities in the menstrual cycle after delivery.
Medications and Radiation Exposure: Certain pharmaceutical drugs and exposure to radiation, especially X-rays like radiography, can have an effect on hormone levels, thus potentially disrupting the menstrual cycle.
Menopause Transition: The gradual phase of menopause marks the end of reproductive capability and is often accompanied by significant alterations and irregularities in menstrual patterns.
Intrauterine Contraceptive Devices (IUCDs): The use of intrauterine devices for contraception can be a factor in altered menstrual patterns and regularity for some individuals.
Severe Stress: Extreme stress and worry, such as that experienced during war or conflict situations, can throw off hormonal balance and negatively impact the menstrual cycle’s regularity.
Anxiety and Mental Health: Conditions like anxiety and other mental health issues can influence hormone levels and potentially contribute to menstrual irregularities.
Environmental and Routine Changes: Shifts in environment, like starting at a new school, or significant changes in daily routines can increase stress levels, indirectly affecting and disrupting the menstrual cycle.
Adolescent Hormonal Fluctuations: The teenage years are marked by substantial hormonal shifts as the body develops. This transitional phase can lead to menstrual irregularities as the hormonal system adjusts and stabilizes.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

