Reproductive Health
Artificial Methods of Family Planning
Table of Contents
Artificial methods of family planning refer to the use of various techniques and devices to prevent pregnancy. These methods rely on the use of
physical barriers, chemicals, or surgical interventions to either prevent sperm from reaching the egg or to interfere with the fertilization process.
FAMILYPLANNINGCARD
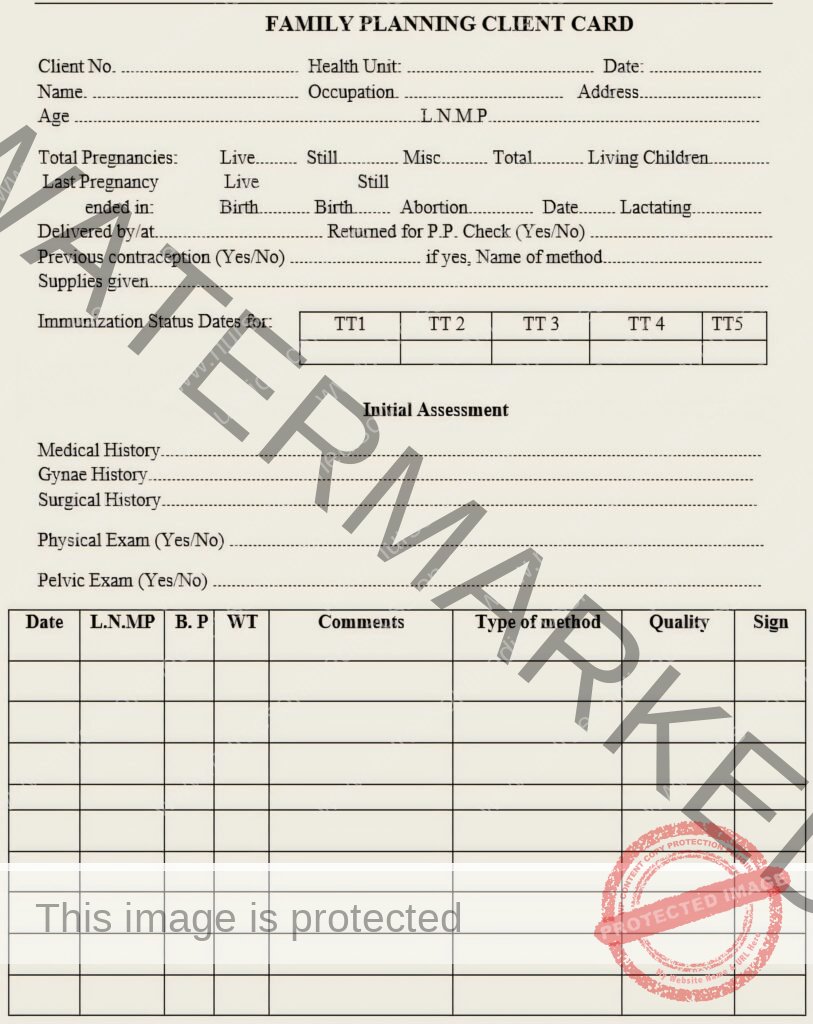
Criteria for Family Planning Method Initiation
Before recommending a specific family planning method, a thorough assessment is crucial. This involves gathering information through history taking and a physical examination to ensure the method is safe and appropriate for the client.
I. History Taking:
Personal Information: Age, sex, address, next of kin.
Social History: Marital status, education level, and habits (e.g., smoking) that might influence method choice.
Medical History: Identification of pre-existing medical conditions, problems, sickle cell disease, and current medications.
Obstetric History:
Menstrual history (age of menarche).
Number of pregnancies and live births.
Gynecological History: Presence of any conditions affecting the reproductive organs (e.g., abnormal bleeding, cervical cancer, pelvic inflammatory disease (PID), breast cancer).
Family Planning History: Previous use of family planning methods and experiences.
II. General Examination:
A head-to-toe examination should be performed to assess overall health:
General Appearance: Look for signs of anemia, edema, jaundice, and lymphadenopathy.
Breast Examination: Observe for any color changes or masses.
Abdominal Examination: Palpate for any abnormal masses.
Pelvic Examination: Assess for abnormal vaginal discharge.
Important Note: Baseline weight and blood pressure should be recorded, especially before initiating hormonal contraceptive methods.
Artificial Methods of Family Planning
These methods are interventions designed to prevent pregnancy.
Barrier Methods:
Spermicides
Condoms (male and female)
Intrauterine Devices (IUCDs)
Diaphragms
Intra-vaginal contraceptive sponges
Cervical caps
Condoms (Male and Female)
Condoms are a popular and long-established barrier method. They are thin sheaths made of rubber (usually latex, sometimes polyurethane) worn on the penis or inside the vagina during sexual intercourse.
Key Benefits of Condoms:
Pregnancy Prevention: When used consistently and correctly, condoms are effective in preventing pregnancy.
STI/HIV Prevention: Condoms are the only family planning method that offers significant protection against sexually transmitted infections, including HIV/AIDS, when used consistently and correctly.
Indications for Condom Use:
Condoms are suitable for a wide range of individuals and situations:
Men seeking active participation in family planning.
Sexually active adolescents.
Couples with infrequent sexual intercourse.
Individuals in casual sexual relationships where pregnancy is not desired.
Couples needing a temporary backup method while waiting for other contraceptive methods to become effective.
Couples needing a short-term method before transitioning to a different contraceptive.
Individuals at increased risk of STIs (e.g., having multiple partners or a partner with other partners).
Couples where one or both partners are HIV positive (to reduce transmission risk).
Male Condoms:
Male condoms are sheaths that fit over an erect penis. The majority are made from thin latex rubber, with some being made from polyurethane (plastic) for individuals with latex allergies.

Condoms: Mechanism, Effectiveness, and Usage
Condoms, available for both males and females, are barrier methods of contraception that also offer significant protection against sexually transmitted infections (STIs).
Primary Mechanism of Action:
Condoms function by creating a physical barrier that prevents the mixing of bodily fluids during sexual intercourse. This prevents:
Pregnancy: By blocking sperm from entering the vagina and reaching the egg.
STI Transmission: By containing infectious agents present in semen, on the penis, or in vaginal fluids, preventing them from infecting the partner.
Effectiveness:
The effectiveness of condoms depends significantly on consistent and correct use.
Male Condoms:
Pregnancy Prevention:
Typical Use: Approximately 18 pregnancies per 100 women whose partners use male condoms over one year. This reflects real-world use, including occasional incorrect or inconsistent use.
Perfect Use: Approximately 2 pregnancies per 100 women whose partners use male condoms correctly with every act of intercourse over one year.
Protection Against HIV and Other STIs:
Significant Risk Reduction: Male condoms significantly reduce the risk of HIV infection when used correctly with every act of sex.
HIV Transmission Prevention: Consistent and correct use can prevent 80% to 95% of HIV transmission that would occur without condoms.
Protection Against Discharge-Spread STIs: Highly effective against STIs spread through bodily fluids, such as HIV, gonorrhea, and Chlamydia.
Protection Against Skin-to-Skin STIs: Offer some protection against STIs spread through skin-to-skin contact, such as herpes and human papillomavirus (HPV), if the condom covers the infected lesions.
Addressing Client Concerns and Questions:
It’s important to address common concerns and myths surrounding condom use:
Reinforce Correct Use: Emphasize the importance of proper application and disposal, and remind clients that condoms are for single use only.
Latex Allergy: Discuss alternative options for individuals with latex allergies.
Dispelling Myths (Male Condoms):
Condoms do not cause sterility, impotence, or weakness.
Condoms do not decrease sex drive.
Condoms do not promote promiscuity.
Condoms cannot get lost inside a woman’s body.
Condoms do not have holes large enough for HIV to pass through.
Condoms are not laced with HIV.
Condoms do not cause illness in women by preventing semen entry.
Condoms do not cause illness in men due to sperm moving back up.
Condoms are used by married couples and are not exclusively for use outside of marriage.
Who Should Not Use Condoms?
Individuals with a confirmed latex allergy should explore non-latex options. However, for those at risk of STIs/HIV, even with an allergy, using a non-latex condom is still recommended as it’s the only method offering significant protection against these infections.
How to Use Male Condoms Correctly:
Use a new condom for every act of sex. Check the package for damage and the expiration date. Open the package carefully by tearing it along the designated edge, avoiding sharp objects.
Before any genital contact, place the condom on the tip of the erect penis with the rolled side facing outwards.
If uncircumcised, retract the foreskin. Pinch the tip of the condom to squeeze out any air.
Unroll the condom completely down to the base of the erect penis.
Immediately after ejaculation, hold the rim of the condom firmly at the base of the penis and withdraw while the penis is still erect. This prevents spillage of semen.
Slide the condom off the penis, being careful not to spill semen.
Dispose of the used condom safely in a trash can. Do not flush it down the toilet.
Practices to Avoid When Using Male Condoms:
Unrolling the condom before placing it on the penis.
Using oil-based lubricants with latex condoms. These can weaken the latex and cause breakage. Use water-based or silicone-based lubricants instead.
Using condoms that are old or damaged. Check for dryness, brittleness, or stickiness.
Reusing condoms. Condoms are designed for single use only.
Practicing dry sex. Increased friction can lead to condom breakage. Use adequate lubrication.
Female Condoms:
Female condoms are sheaths that are inserted into the vagina. The most common type is the Female Condom 2 (FC2), which is made of thin, soft, synthetic rubber (nitrile) film and has flexible rings at both ends. Latex female condoms are available in some countries.
Primary Mechanism of Action (Female Condoms):
Similar to male condoms, female condoms create a barrier that:
Prevents Pregnancy: By blocking sperm from entering the uterus.
Prevents STI Transmission: By preventing the exchange of bodily fluids between partners.

- Female Condoms: Effectiveness, Characteristics, and Usage
Female condoms are a woman-controlled barrier method of contraception that also provides protection against sexually transmitted infections (STIs).
Effectiveness:
The effectiveness of female condoms, like male condoms, depends significantly on consistent and correct use.
Pregnancy Prevention:
Perfect Use: Approximately 5 pregnancies per 100 women using female condoms correctly with every act of intercourse over one year.
Typical Use: Approximately 21 pregnancies per 100 women using female condoms over one year. This reflects real-world use, including potential for incorrect or inconsistent use.
Protection Against HIV and Other STIs:
Risk Reduction: Female condoms reduce the risk of infection with STIs, including HIV, when used correctly with every act of intercourse.
Characteristics of Female Condoms:
Female condoms offer several advantages:
Safe: Generally considered a safe method with minimal risks.
Woman-Initiated: Allows women to take control of their contraceptive and STI protection.
Body Heat Conduction: The soft texture quickly warms to body temperature during sex.
Dual Protection: Provides protection against both pregnancy and STIs, including HIV.
Potential for Added Stimulation: The outer ring can provide additional sexual stimulation for some women.
No Provider Requirement: Does not require a prescription or professional fitting.
Can Be Inserted in Advance: Can be inserted up to eight hours before intercourse, allowing for spontaneity.
Comfortable Fit: Not typically tight or constricting like male condoms.
Minimal Sensation Interference: Generally does not dull sexual sensation like male condoms can for some.
No Immediate Removal Needed: Does not need to be removed immediately after ejaculation.
No Systemic Side Effects: Does not introduce hormones or other substances into the body.
Temporary Backup: Can be used as a temporary alternative or backup to other methods.
Protection Against STI-Related Conditions: Helps protect women from pelvic inflammatory disease (PID), cervical cancer, and infertility caused by STIs.
Important Considerations:
Lower Typical Effectiveness: As typically used, female condoms are less effective than many other family planning methods.
Partner Communication: Requires communication and cooperation with the partner for proper use.
Insertion Can Be Difficult Initially: Some women may find insertion challenging at first.
Potential for Noise: May produce some rustling or squeaking sounds during intercourse.
Side Effects of Female Condoms:
None: Generally free of physical side effects.
Rare Allergic Reactions: Allergic reactions to latex (in latex versions) are possible, though uncommon.
Who Can Use Female Condoms?
Synthetic Rubber (Nitrile) Female Condoms: Safe for all men and women to use.
Natural Latex Female Condoms: Safe for all men and women, except those with a severe latex allergy (which is extremely rare).
How to Use Female Condoms Correctly:
Use a new condom for each act of sex.
Check the Condom: Do not use if torn, damaged, or past the expiration date.
Open the Package: Carefully open the package.
Insertion (Before Any Physical Contact): Can be inserted up to eight hours before sex.
Find a Comfortable Position: Squatting, raising one leg, sitting, or lying down.
Prepare the Condom: Grasp the inner ring at the closed end and squeeze it to make it long and narrow.
Insert the Inner Ring: With your other hand, separate the labia and locate the vaginal opening. Gently push the inner ring into the vagina as far as it will go.
Final Positioning: Use a finger to push the inner ring further until it’s just past the pubic bone. The larger outer ring will remain outside the vagina.
Ensure Proper Penis Entry: Guide the penis into the opening of the condom and ensure it stays inside during intercourse.
Removal: To remove the condom, hold and twist the outer ring to seal in fluids. Gently pull the condom out of the vagina. It doesn’t need to be removed immediately after sex but should be removed before standing up to avoid semen spillage.
Disposal: Dispose of the used condom safely in a trash can. Do not flush it.
Tips for New Users:
Practice: Encourage new users to practice insertion and removal before having sex. Reassure them that it becomes easier with practice.
Experiment with Positions: Suggest trying different positions to find what makes insertion easiest.
Take it Slow: Advise slow and gentle insertion, especially in the beginning.
Continue with Previous Method: If switching from another method, suggest continuing with the old method until comfortable and confident using the female condom.
Follow-Up and Counseling:
Provide ongoing support and counseling to address:
Client Concerns and Questions.
Reinforce Correct Condom Use.
Dispelling Myths (Female Condoms):
Female condoms cannot get lost inside the body.
Female condoms are not difficult to use; correct use just needs to be learned.
Female condoms do not have holes large enough for HIV to pass through.
Female condoms are used by married couples and are not only for use outside of marriage.
Female condoms do not cause illness by preventing semen entry.
General Advantages of Condoms (Male and Female):
Effective when used correctly.
No medical supervision required for purchase or use.
Convenient to carry.
Prevent both pregnancy and STIs, including HIV/AIDS.
Generally easy to use (with practice).
Reduce the risk of systemic side effects and reactions.
Fairly inexpensive and widely available.
General Disadvantages of Condoms (Male and Female):
Potential for loss of spontaneity.
May rupture or lose position during intercourse.
Condom use can be associated with extramarital sex and STIs, leading to stigma in some communities.
Not suitable for individuals who are poorly motivated to use them consistently.
Lack of privacy when purchasing condoms may be a concern for some.
Male condoms cannot be used by a man who cannot maintain an erection.
Requires male responsibility (for male condoms).
Some individuals may consider them “unclean.”
Spermicides
This involves application of chemicals into the vagina to prevent pregnancy.

Mode of Action:
Spermicides are contraceptive substances designed to kill or inactivate sperm, thereby preventing fertilization.
Forms of Spermicides:
Spermicides are available in various formulations, including:
Jellies
Creams
Foams
Suppositories or Tablets (vaginal inserts)
Lubricants in some condoms
As an active ingredient in the vaginal contraceptive sponge
Advantages of Spermicides:
Availability: Generally available without a prescription, making them easily accessible.
Effectiveness (with correct use): Can be fairly effective when used consistently and correctly.
Backup Method: Can be used as a backup method with other forms of contraception for increased effectiveness.
On-Demand Use: Used only when needed, offering flexibility.
Woman-Controlled: The woman can independently use this method.
Additional Lubrication: Provide extra vaginal lubrication, which can enhance sexual intercourse.
Limited STI/PID Protection: May offer some limited protection against certain sexually transmitted infections (STIs) and pelvic inflammatory disease (PID). Note: This protection is not as robust as barrier methods like condoms.
Disadvantages of Spermicides:
Low Effectiveness Alone: Not highly effective when used as the sole method of contraception.
Messiness: Some couples find the method messy due to its fluid consistency.
Potential for Allergic Reactions: Can cause allergic reactions or irritation in some individuals.
Interruption of Intercourse: Requires application shortly before intercourse, which can interrupt spontaneity.
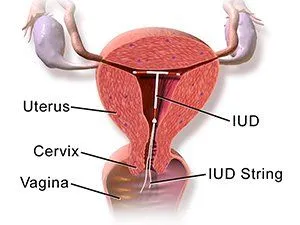
Intra-Uterine Contraceptive Devices (IUCDs)
IUCDs are highly effective, long-acting reversible contraceptives inserted into the uterus to prevent pregnancy.
Mode of Action:
Intra-uterine contraceptive devices (IUCDs) are devices inserted into the woman’s uterus. Their primary mechanism of action is to prevent implantation of a fertilized egg by causing a local inflammatory reaction within the uterine environment.
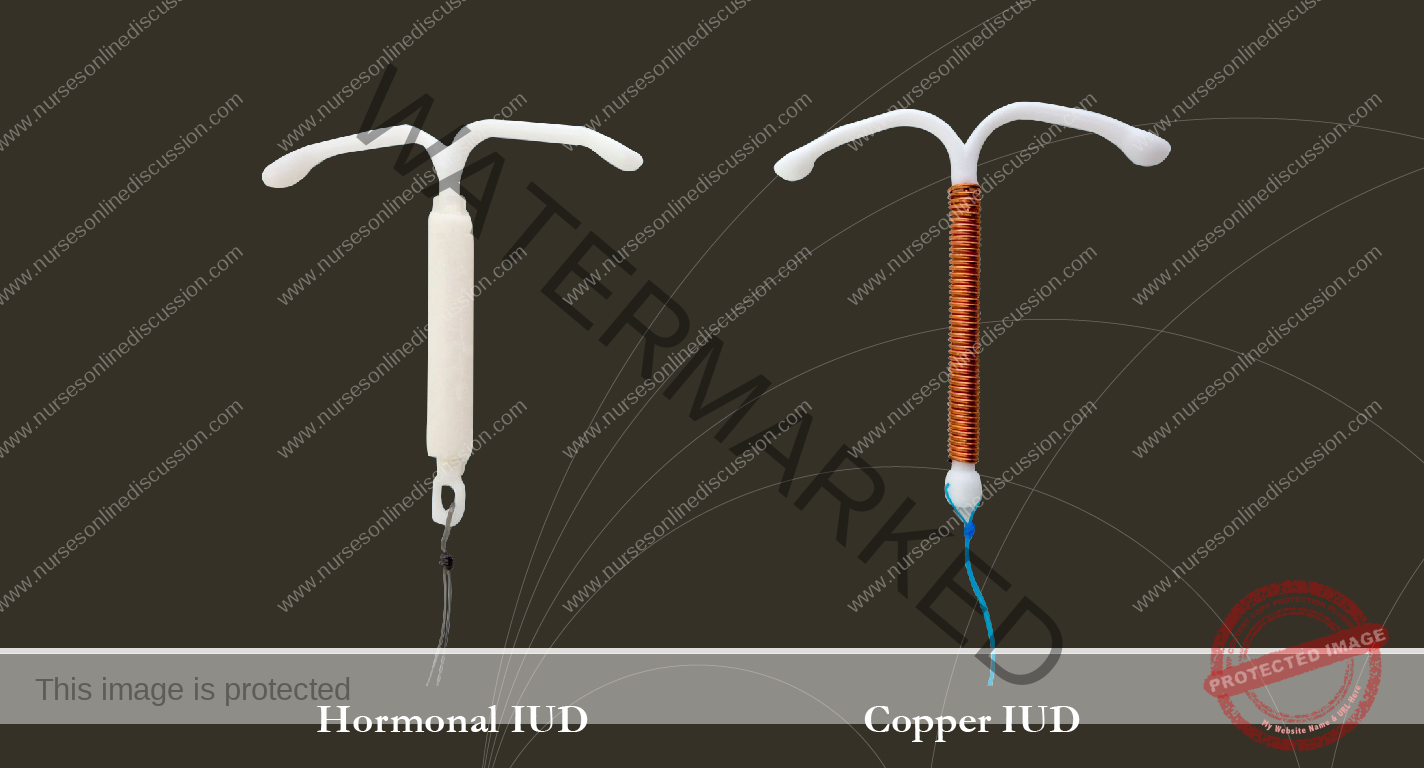
Types of IUCDs
Copper T 380A effective for 10-12 years
Multi-load 375 for 5 years
Mirena R hormonal IUCD
Advantages of IUCDs:
Highly Effective: Begins working immediately upon insertion.
Long-Lasting: Eliminates the need for frequent refills or repeated actions.
Extended Protection: Offers contraceptive protection for several years (up to 10 years or more, depending on the type).
Rapid Return to Fertility: Fertility returns immediately upon removal.
Limited Systemic Side Effects: Generally associated with fewer systemic side effects compared to hormonal methods.
No Interruption to Intercourse: Does not require any action at the time of sexual activity.
Safe for Breastfeeding Mothers: Does not affect breastfeeding.
Infrequent Follow-Up: Typically requires only one follow-up visit unless problems arise.
Side Effects of IUCDs:
Increased Menstrual Bleeding: Some women experience heavier menstrual flow.
Spotting: Bleeding between periods may occur, especially in the initial months.
Abnormal Vaginal Discharge.
Menstrual Cramps: Increased cramping during menstruation is possible.
Pelvic Inflammatory Disease (PID): A risk, particularly shortly after insertion.
Indications for IUCD Use:
Breastfeeding Women.
Women of Any Age (including adolescents and older women).
Similar Indications to Progestogen-Only Pills (POPs).
Contraindications for IUCD Use:
Irregular Vaginal Bleeding of Unknown Origin (potential sign of cervical cancer).
Known or Suspected Pregnancy.
Heavy and Painful Menstruation (may be exacerbated by IUCD).
Cancer of the Uterus.
Current Pelvic Inflammatory Disease (PID).
Multiple Sexual Partners (increased risk of STI and subsequent PID).
Uterine Abnormalities that distort the uterine cavity.
Managing PID in IUCD Users:
IUCD users who develop PID should be treated with antibiotics. The IUCD can remain in place if the woman desires and there is improvement within 72 hours. If there is no improvement, the IUCD should be removed.
Insertion of IUCD:
Timing of Insertion:
Any time during the menstrual cycle, provided pregnancy is ruled out.
Within the first seven days of the menstrual cycle.
Immediately following delivery or within 48 hours after childbirth.
Any time beyond four to six weeks postpartum.
Immediately or within seven days after an uncomplicated abortion.
During Cesarean section.
Procedure:
Aseptic Technique: Employ strict aseptic technique, including handwashing and sterile gloves.
Device Preparation: Load the IUCD into the introducer and plunger. The IUCD straightens within the introducer.
Cervical Visualization: Insert a Cusco’s vaginal speculum to clearly visualize the cervix.
Cervical Cleaning: Clean the cervix and vaginal vault with sterile swabs.
Uterine Sounding: Measure the length of the uterus using a uterine sound.
Introducer Insertion: Insert the introducer through the cervical opening into the uterus.
IUCD Deployment: Gently push the plunger to release the IUCD from the introducer into the uterus.
IUCD Positioning: Once released, the IUCD will resume its original shape and lodge against the uterine walls.
String Management: The two small strings attached to the IUCD will hang down through the cervical opening.
String Trimming: Cut the strings with sterile scissors, leaving approximately 3 cm protruding from the cervix.
Post-Insertion Monitoring: Allow the client to remain on the procedure table until she feels ready to get dressed.
String Check Education: Instruct the woman on how to feel for the strings in the vagina to confirm the IUCD’s position.
Post-Insertion Instructions:
Backup Contraception: Use a backup method of contraception for a minimum of 7 days.
Expected Discomfort: Some mild pain is normal and usually does not require medication.
String Checks and Follow-Up: Instruct the woman to check the strings during menstruation to ensure the IUCD is in place and to return if the strings are missing or feel different.
When to Seek Immediate Care: Advise the woman to return to the facility immediately if she experiences any significant discomfort, heavy bleeding, fever, or signs of infection.
Removing the IUCD:
Counseling and Discussion: If a client experiences intolerable side effects, discuss her concerns and weigh her preference for managing the problem versus removal.
Timing of Removal: IUCD removal can usually be done at any time during the menstrual cycle.
Easier Removal During Menstruation: Removal may be easier during menstruation when the cervix is naturally slightly dilated.
Referral for Difficult Removals: In cases of suspected uterine perforation or difficult removal, refer the client to an experienced provider for appropriate removal techniques.
Steps for IUCD Removal:
Explain the Procedure: Clearly explain the removal process to the client.
Ensure Privacy and Confidentiality.
Position the Client: Ask the client to lie on her back on the examination table.
Speculum Insertion: The provider inserts a vaginal speculum to visualize the cervix and IUCD strings.
Cervical Cleaning and Inspection: Carefully clean the cervix and vagina with an antiseptic solution and perform a visual inspection.
Comfort Measures: Instruct the client to take slow, deep breaths and inform the provider of any pain or discomfort during the procedure.
String Retrieval: Using narrow forceps, the provider gently grasps the IUCD strings.
Gentle Removal: The provider slowly and steadily pulls the strings until the IUCD is completely removed from the cervix.
Show the IUCD: Show the removed IUCD to the client and allow her to handle it if she wishes. This can help reassure her that nothing remains inside.
Thank the Client for her cooperation.
Clean Up.
Reasons for Missed Threads in IUCD Users:
Thread Retraction: The threads may have coiled up inside the uterus or cervical canal.
Thread Breakage: The threads may have torn.
Spontaneous Expulsion: The IUCD may have been expelled unnoticed by the client.
Uterine Perforation: The IUCD may have migrated through the uterine wall into the peritoneal cavity.
Uterine Growth (Pregnancy): The growing uterus in early pregnancy can pull the IUCD upwards, making the threads difficult to locate.
Methods of Identifying a “Missing” IUCD:
History Taking: Rule out pregnancy as a first step.
Ultrasonography: To visualize the IUCD’s location within or outside the uterus.
Hysteroscopy: A procedure using a thin, lighted tube with a camera to view the inside of the uterus.
Straight X-ray: To locate the IUCD if perforation is suspected.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowGet in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

