Conditions of the eye
Subtopic:
Cataract
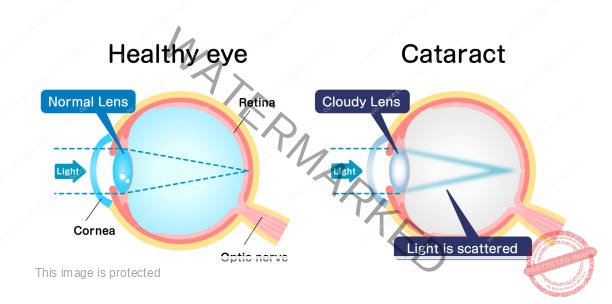
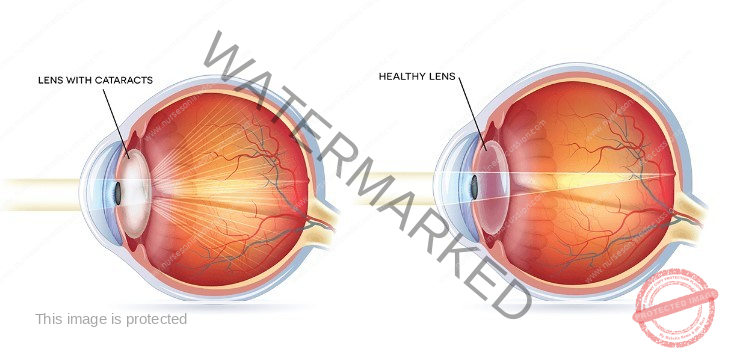
Cataract describes the lens of the eye becoming cloudy or less transparent, which hinders clear sight. This happens when proteins within the lens structure begin to stick together. This aggregation of proteins disrupts the normal passage of light through the lens. Instead of focusing clearly on the retina, the light is scattered. Consequently, the image formed on the retina lacks sharpness, leading to vision that appears hazy or less distinct. Cataracts can affect either one or both eyes independently and are not contagious. The medical term for this reduction in lens clarity or the development of cloudiness is Cataract.
How Healthy Eyes Work
In an eye functioning normally, light first enters through the clear front surface called the cornea, and then passes through the pupil (the black dot in the center of your eye). The lens, located behind the pupil, then focuses this incoming light precisely onto the retina, the light-sensitive layer at the back of the eye. This focused light creates a sharp, clear image, much like a camera lens focuses light onto the film.
The Impact of Cataracts
When a cataract develops, the lens loses its clarity and becomes cloudy. This cloudiness interferes with the way light passes through the lens. Instead of being focused neatly onto the retina, the light is scattered in different directions. Think of it like trying to see through a frosted window. Because the light is scattered, the image that reaches the retina is blurry and lacks sharpness. As the cataract gets worse over time, this blurring can significantly affect vision, making everyday activities like reading, driving, and recognizing faces increasingly challenging. A cataract can develop in one eye or both.
Risk Factors for Cataracts in Adults
While aging is the primary reason cataracts develop, several other things can increase your chances of getting them:
Age: Getting older is the most significant risk factor. Cataracts are very common in older adults.
Exposure to Sunlight (UV Light): Spending a lot of time in the sun without proper eye protection can damage the lens over time.
Smoking: The harmful chemicals in cigarette smoke can negatively affect the lens of the eye.
Diabetes: Having high blood sugar levels over time can cause changes in the lens that lead to cataracts.
Eye Injuries (Trauma): Any injury to the eye, whether a blunt force or something piercing the eye, can cause a cataract to form.
Family History: If you have family members who have had cataracts, you might be more likely to develop them.
Long-Term Use of Corticosteroid Medications: Taking these medications for a long time can sometimes contribute to cataract development.
Radiation Exposure: Being exposed to radiation, like from X-rays, can increase the risk.
Electrical Injury: Experiencing an electric shock can damage the lens and cause a cataract.
Myotonic Dystrophy: This is a genetic condition that can cause cataracts to develop at a younger age.
Inflammation Inside the Eye (Uveitis): Long-term inflammation in the middle layer of the eye can harm the lens.
Causes of Cataracts
Several factors can lead to the formation of cataracts:
Aging: This is the most frequent cause. As we age, the proteins in the lens of the eye can start to clump together, causing cloudiness.
Other Eye Diseases: Conditions like diabetes and uveitis can damage the lens and cause cataracts.
Previous Eye Surgery: Sometimes, surgery for other eye problems like glaucoma can increase the risk of developing cataracts later.
Certain Medications: Using steroid medications or phenothiazines for extended periods can contribute to cataract formation.
Eye Injuries: Damage to the eye, including if a foreign object gets inside, can lead to a cataract.
Exposure to Radiation: Being exposed to X-rays or ultraviolet (UV) rays can harm the lens.
Being Born with Cataracts (Congenital): Some babies are born with cataracts. This can be due to illnesses the mother had during pregnancy, like rubella, or because of genetic conditions.
Inherited Conditions: Certain genetic disorders like myotonic dystrophy and Marfan syndrome, as well as severe nearsightedness (high myopia), can make someone more likely to get cataracts.
Severe Dehydration: In rare cases, extreme dehydration, like that seen in people with cholera, has been linked to an increased risk of cataracts. This has been observed in some cases in India.
Types of Cataracts
Cataracts can be categorized in a few different ways:
Acquired Cataracts: These are cataracts that develop after birth.
Age-Related Cataract: This is the most common type and typically starts to appear after the age of 40.
Presenile Cataract: This refers to cataracts that occur in people younger than the typical age for age-related cataracts.
Traumatic Cataract: This type of cataract is a direct result of an injury to the eye.
Drug-Induced Cataract: These cataracts are caused by the long-term use of certain medications, with corticosteroids being a notable example.
Secondary Cataract: This type develops as a consequence of other medical conditions, such as diabetes, or inflammation inside the eye.
Congenital Cataracts: These are cataracts that are present at birth.
Inborn Cataract: These cataracts are present from birth and are often linked to genetic conditions or infections the mother had during pregnancy.
Classifications of Cataracts
Age-Related Cataract Classification
A. Morphological Classification
NUCLEAR CATARACT

CORTICAL CATARACT

Cortical Cataract: Develops in the outer layer or cortex of the eye’s lens. It initiates at the periphery of the lens, progressing inwards towards the center with distinctive white, wedge-like opacities. This specific type of cataract is frequently associated with causing significant glare issues, particularly in bright light conditions.
SUBCAPSULAR CATARACT
Develops immediately beneath the lens capsule, located at the back of the lens.
Begins as a small, opaque area, often initially subtle.
Typically forms near the rear surface of the lens, directly impacting the path of light as it travels to the retina.
Notably interferes with close-up vision needed for tasks like reading.
Vision may be notably reduced in bright light conditions.
Commonly induces glare or halos around light sources, particularly noticeable at night.
POSTERIOR SUBCAPSULAR CATARACTS

Posterior Subcapsular Cataracts: These cataracts originate at the back surface of the lens (near the posterior pole) and tend to spread outwards towards the periphery, or edges, of the lens.
Their development can be linked to conditions where the eye experiences chronic inflammation or with prolonged use of certain medications, notably corticosteroids (steroids).
They tend to affect vision more significantly than some other types of cataracts because their location causes light to scatter as it converges towards the back of the lens.
Dilating eye drops can sometimes be helpful in improving vision in this type of cataract, as dilation enlarges the pupil allowing more light to enter the eye around the opacity.
B. MATURITY CLASSIFICATION
IMMATURE CATARACT
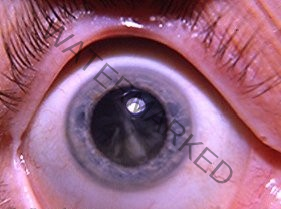
Immature Cataract: In this stage, the lens is partially opaque, meaning it is not entirely cloudy. Some areas of the lens remain clear, allowing some light transmission.
Vision is still possible, though it may be significantly impaired depending on the extent and location of the opacity within the lens.
MATURE CATARACT
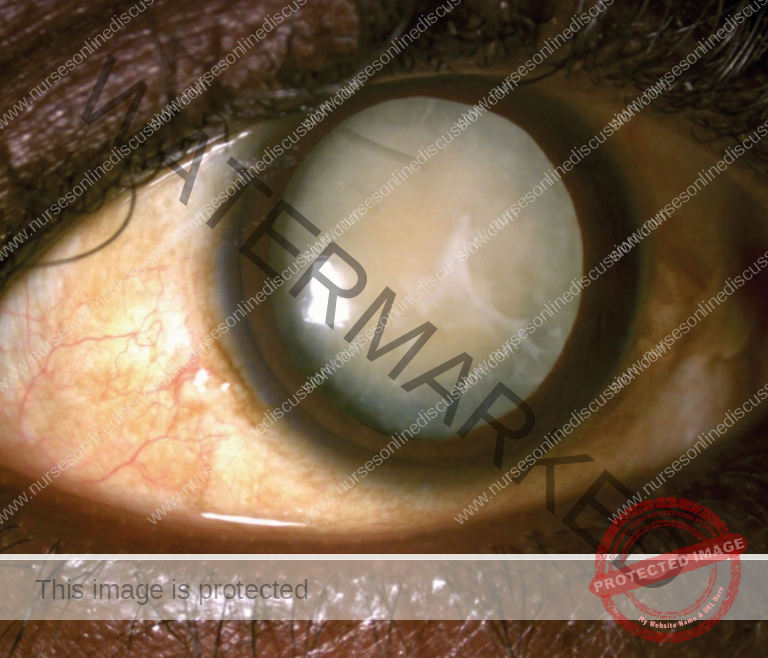
Mature Cataract: The lens becomes completely opaque, signifying a total clouding of the lens. This leads to a significant reduction in vision as light is unable to effectively pass through the lens to the retina.
The lens typically appears pearly white in color due to the complete opacification.
A mature cataract is characterized by an obvious white opacity visibly centered at the pupil.
HYPERMATURE CATARACT (Morgagnian)

Hypermature Cataract (Morgagnian): In this advanced stage, the lens cortex undergoes liquefaction, becoming fluid-like, and the lens nucleus, the dense central part, may sink downwards within the lens capsule due to gravity. This can potentially lead to a wrinkled anterior lens capsule and increased risk of severe complications.
Intumescent Type: The proteins within the lens break down and the lens absorbs water, causing it to become swollen and appear milky white.
Liquefactive/Morgagnian Type: The lens cortex undergoes auto-lytic liquefaction and turns uniformly milky white. The lens nucleus loses its supporting structure and settles to the bottom of the lens capsule.
CONGENITAL CATARACT

Congenital Cataract Classification
Congenital cataracts, those present at birth, occur in approximately 3 out of every 10,000 live births. Interestingly, in about two-thirds of these cases, the condition affects both eyes. While the exact cause can be identified in roughly half of the cases, the most frequent underlying reason is a genetic mutation. In infants, congenital cataracts can lead to the development of amblyopia, commonly known as “lazy eye,” where vision in one eye doesn’t develop properly. Congenital cataracts can be broadly categorized as follows:
Systemic Association: These cases are linked to other medical conditions affecting the entire body.
Metabolic Disorders: Certain metabolic disorders can interfere with the lens’s normal development. For example, galactosemia and galactokinase deficiency are conditions where the body has trouble processing specific sugars, which can lead to cataract formation in infants.
Prenatal Infections: If a mother experiences certain infections during pregnancy, it can affect the developing baby’s eyes. A classic example is congenital rubella syndrome, which can cause a range of problems, including cataracts in newborns.
Chromosomal Abnormalities: Certain genetic syndromes involving extra or missing chromosomes can increase the risk of congenital cataracts. Examples include Down syndrome (Trisomy 21), Patau syndrome (Trisomy 13), and Edward syndrome (Trisomy 18).
Non-Systemic Association: In these instances, the cataracts are not directly linked to a broader systemic illness.
Idiopathic Cases: Sometimes, despite thorough investigation, the exact cause of congenital cataracts remains unknown. These are referred to as idiopathic cases.
Clinical Presentation of Cataracts
The presence of a cataract can manifest in several noticeable ways:
Blurred Vision: This is a gradual decline in the sharpness of vision. Individuals may find it increasingly difficult to see fine details, making tasks like reading small print challenging.
Reduced Visual Acuity: This refers to a decrease in the overall clarity of vision, affecting both near and far objects. Things may appear less sharp, regardless of distance.
Night Vision Problems: Cataracts can make it harder to see in dimly lit environments or at night. This is because the cloudy lens scatters light, making it difficult for the eye to process images in low light conditions.
Glare Sensitivity: Bright light sources can become bothersome or even painful. Sunlight, car headlights, or even indoor lighting might cause discomfort or produce distracting halos around the light.
Halos Around Lights: Due to the scattering of light by the cataract, individuals may perceive rings or circles of light surrounding bright light sources.
Double Vision: In some cases, a cataract in one eye can cause diplopia, or double vision, where a single object appears as two distinct images.
Color Distortion: The lens can become discolored by a cataract, often with a yellowish or brownish tint. This can affect how colors are perceived, making them appear faded or with a yellow tinge.
Differential Diagnosis
It’s important to distinguish cataracts from other eye conditions that can cause similar symptoms:
Glaucoma: This condition involves increased pressure inside the eye, which can damage the optic nerve. While both can affect vision, glaucoma’s primary issue is nerve damage, unlike the lens clouding in cataracts.
Diabetic Retinopathy: This is damage to the blood vessels in the retina caused by diabetes. It can cause blurry vision but involves blood vessel abnormalities rather than lens opacity.
Hypertensive Retinopathy: High blood pressure can also damage the blood vessels in the retina, leading to visual disturbances that might be confused with cataract symptoms.
Age-Related Macular Degeneration (AMD): AMD affects the central part of the retina, leading to a loss of central vision. While both conditions affect vision in older adults, AMD primarily impacts central vision, while cataracts cause a more general blurring.
Retinitis Pigmentosa: This is a group of inherited diseases that cause progressive degeneration of the retina. It typically starts with night vision problems and peripheral vision loss, unlike the initial blurring associated with cataracts.
Trachoma: This is a bacterial infection that causes scarring of the inner eyelid, which can damage the cornea and lead to vision loss. It’s an infectious condition, unlike cataracts.
Onchocerciasis (River Blindness): This parasitic infection, transmitted by blackflies, can cause severe itching, skin changes, and eventually blindness, including cataract formation.
Vitamin A Deficiency: A lack of vitamin A can lead to various eye problems, starting with night blindness and potentially progressing to total blindness if untreated.
Clinical Findings / Investigations
A key objective finding when assessing for cataracts is a decreased visual acuity. This means the sharpness of vision is reduced.
This reduction in sharpness is typically measured using a standardized eye chart, either a wall chart for distance vision or a near-vision card for close-up vision.
VISUAL ACUITY
Acuity specifically refers to the clarity or sharpness of vision, indicating how well an individual can discern details.
During a visual acuity test, the eye doctor assesses how well the patient can read letters or symbols from a set distance.
The test is performed on each eye separately, with the eye not being tested covered.
The eye chart presents letters or symbols in progressively smaller sizes from top to bottom. The smallest line the patient can read accurately determines their level of visual acuity.
2. SLIT LAMP EXAM (SLE)
• SLE allows the ophthalmologist to see the structures of the eye under magnification.
• The microscope is called a slit lamp because it uses an intense slit of light to illuminate your cornea, iris, and lens.
• These structures are viewed in small sections to detect any small
abnormalities
3. DILATED EXAM
To get a clearer view of the back of your eye, the doctor will put special eye drops in your eyes to make your pupils widen (dilate). This is like opening a window wider to see inside. This allows the ophthalmologist to thoroughly examine the lens for any signs of a cataract and determine how cloudy it has become. The dilated view also enables the doctor to check the health of your retina and optic nerve. The effect of these dilating drops usually lasts for a few hours, gradually wearing off as your pupils return to their normal size.
4. REFRACTION
Your doctor will perform a refraction test to determine if your decreased vision is simply due to needing a new glasses prescription or if there’s another underlying issue, such as a cataract, causing the reduction in your visual sharpness.
Treatment/Management of Cataracts
1. Non-Surgical Management
Glasses: Cataracts change how light bends as it passes through your eye’s natural lens. New eyeglasses or contact lenses with the most accurate prescription can often help to maintain good vision in the early stages of cataract development.
Patient Advice:
Lighting: Enhance the lighting in your home by adding more lamps or using brighter bulbs to make tasks easier.
Sunglasses: When outdoors, consistently wear sunglasses to shield your eyes from glare and further potential damage from ultraviolet (UV) light.
Night Driving: Limit or avoid driving at night, as cataracts can significantly worsen vision in low-light conditions and cause distracting glare from headlights.
2. Surgical Management
Indications: Cataract surgery is considered when:
Changes in your eyeglasses prescription no longer provide satisfactory vision improvement.
The presence of the cataract significantly impacts your quality of life, making everyday activities difficult.
Removing the cataract is likely to improve your vision significantly (meaning the blurry vision isn’t due to other eye problems correctable with glasses).
Surgical Techniques:
Phacoemulsification:
Procedure: This is the most common modern technique. A very small incision is made in the eye. A tiny probe with a hollowed tip is inserted, which uses high-frequency ultrasonic vibrations to break the cloudy lens (cataract) into tiny pieces. The same probe then suctions these fragments out of the eye.
Advantages: This technique is minimally invasive, very precise, and typically leads to a quicker recovery time compared to older methods.
Extracapsular Cataract Extraction (ECCE):
Procedure: A larger incision is made in the eye. The central part of the lens (nucleus) and the outer layer (cortex) are removed from the lens capsule, but a part of the lens capsule is left behind.
Advantages: By preserving the back portion (posterior capsule), the surrounding edge (peripheral anterior capsule), and the supporting fibers (zonules) of the lens capsule, it can reduce the risk of certain complications like the vitreous gel from the back of the eye bulging forward (vitreous prolapse).
Intracapsular Cataract Extraction:
Procedure: This is a less common technique now. A larger incision is made, and the entire lens, including the nucleus, cortex, and capsule, is removed as one whole piece after the fibers holding the lens in place (zonules) are broken.
Advantages: Because the entire lens capsule is removed, there is no risk of developing posterior capsular opacification (often called an “after-cataract”), which is a clouding of the remaining lens capsule that can occur after other types of cataract surgery.
Disadvantages: This method carries a higher risk of complications during surgery, such as the vitreous gel prolapsing or the retina detaching from the back of the eye.
3. Pre-Operative Assessment:
General Health Evaluation:
Your blood pressure will be checked to ensure it’s within a safe range for surgery.
The medical team will assess your ability to comfortably lie flat for the duration of the surgical procedure and your capacity to cooperate with instructions.
Eye Drop Instillation Instruction: You will be taught the correct way to put in eye drops, as you will need to administer them before and after surgery.
Reassurance and Consenting: The medical team will address any concerns you may have, answer your questions, and obtain your informed consent before proceeding with the surgery.
Intraocular Pressure: Your eye pressure will be checked to ensure it is normal or that any pre-existing glaucoma is well-controlled before surgery.
4. Post-Operative Care:
Discharge: Most patients are able to go home on the same day as their cataract surgery.
Follow-Up: You will have scheduled follow-up appointments to monitor your healing progress. Typically, these appointments are the day after surgery, about a week later, and then again after approximately one month.
Patient Advice:
Discomfort: Experiencing mild discomfort or scratchiness in the eye is normal for the first few days following surgery.
Eye Patch/Shield: You will need to wear an eye patch or protective shield, especially while sleeping, on the day of surgery.
Exertion: It’s crucial to avoid any strenuous activities or heavy lifting to prevent increased pressure within the eye.
Trauma: Take precautions to protect your eye from any potential bumps or injuries.
Medications: Your doctor will likely prescribe eye drops to aid healing and prevent complications:
Steroid drops: These help to reduce inflammation within the eye.
Antibiotic drops: These are used to prevent infection after surgery.
Complications of Cataract Surgery
While cataract surgery is generally safe and effective, like any surgical procedure, there are potential complications:
Infective Endophthalmitis: This is a rare but very serious infection inside the eye that can develop after surgery and can lead to significant vision loss if not treated promptly.
Suprachoroidal Hemorrhage: This is a severe, though uncommon, bleeding complication that can occur during surgery, potentially causing permanent vision loss.
Uveitis: Inflammation of the middle layer of the eye (uvea) can occur after surgery, particularly in individuals with a history of uveitis or diabetes.
Ocular Perforation: This is a very rare instance where the eye structures are unintentionally pierced during the surgery.
Refractive Error: If the implanted artificial lens (intraocular lens or IOL) isn’t the precise power needed for your eye, you may still need glasses for optimal vision after surgery.
Posterior Capsular Rupture and Vitreous Loss: If the back part of the lens capsule breaks during surgery, it can lead to a loss of some of the vitreous gel and may slightly increase the risk of a future retinal detachment.
table
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2026 Nurses online discussion. All Rights Reserved

