Communicable Diseases
Subtopic:
Disease Transmission Cycle
Communicable or infectious diseases are caused by infectious agents, also known as pathogens, or the toxins they produce. Pathogens are organisms capable of causing infection. They possess the ability to survive and thrive within the bodies of humans or animals.
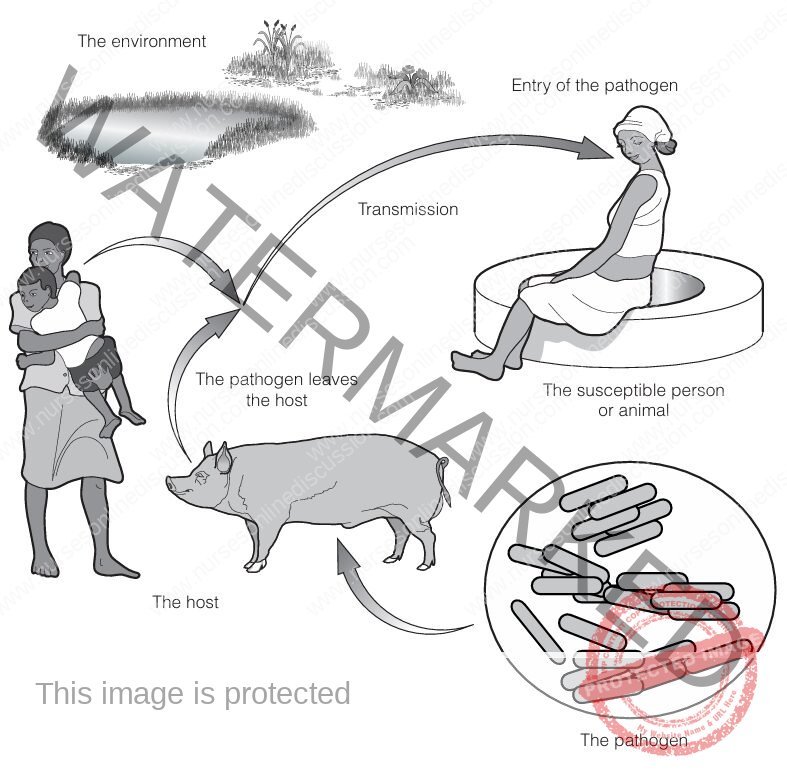
For pathogens to endure and spread, they must successfully exit an infected host, survive their journey through the environment during transmission, enter a person or animal who is susceptible, and then grow or multiply within the newly infected host. This repeating sequence is termed the transmission cycle of disease, or simply the transmission cycle. This cycle can be straightforward, involving direct transfer, or more intricate, incorporating intermediate hosts or vectors. Understanding these sequences is vital for preventing the spread of infections.
The transmission cycle comprises several essential components:
The pathogen: The microbial agent responsible for initiating the infection.
The host: The person or animal carrying the infectious pathogen.
The exit: The route or method by which the pathogen leaves the infected host’s body.
Transmission: The process by which the pathogen moves from the host to a susceptible individual or animal. This stage can involve phases in the external environment, or require intermediate hosts or vectors.
The environment: The external setting where the transfer of the pathogen takes place.
The entry: The pathway or method by which the pathogen gains access into the susceptible person or animal.
The susceptible person or animal: The potential recipient who is vulnerable to becoming infected by the pathogen.
Let’s examine some of these components in greater detail:
The Pathogen
The pathogen is the specific biological agent that initiates the infection. Different pathogens cause distinct infections; for example, Vibrio cholerae specifically causes cholera.
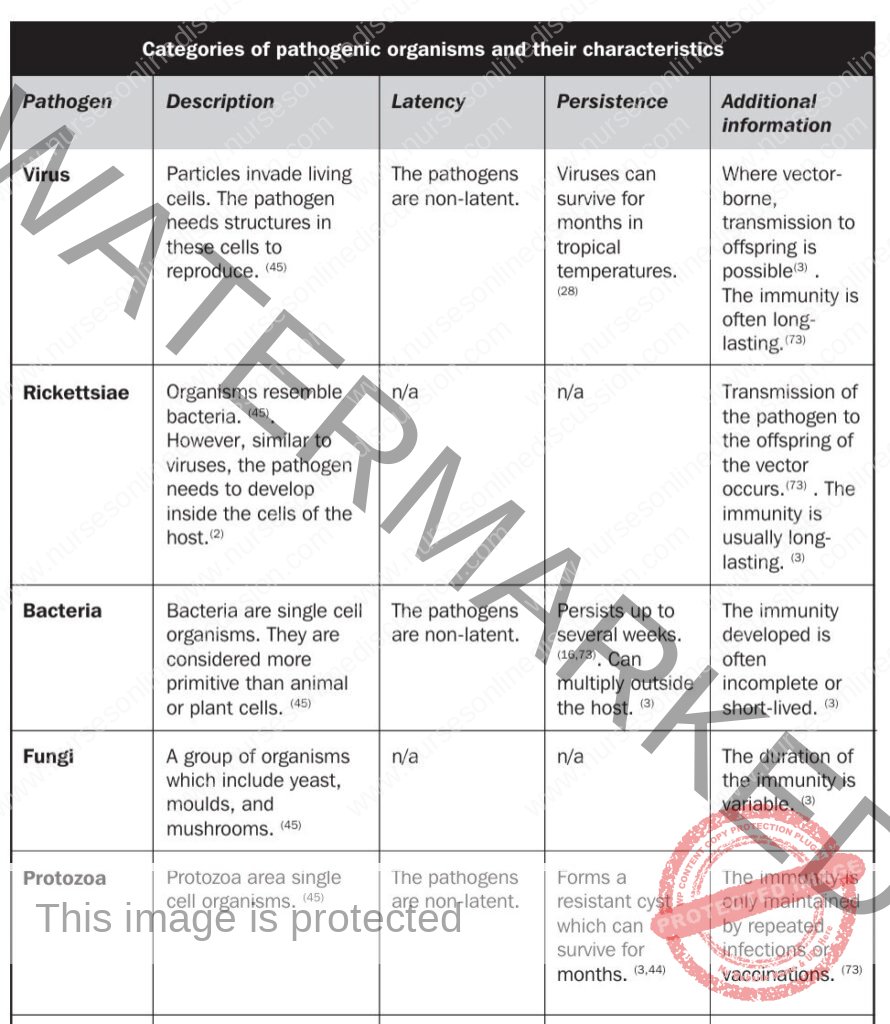
Pathogens causing diseases covered in relevant materials include viruses, bacteria, rickettsiae, fungi, protozoa, and helminths (parasitic worms).
All pathogens follow a life course involving stages of development, maturation, structural changes, multiplication or reproduction, dispersal, and subsequent infection of a new host. This progression is referred to as the development of the pathogen.
Two terms describe pathogens exiting the host via faeces or urine:
Latency: After being shed, a latent pathogen needs to undergo development in the external environment or within an intermediate host before it becomes capable of infecting a susceptible host. The pathogen is not infectious during this required development period. Non-latent pathogens do not need this maturation step and can cause infection immediately upon being excreted.
Persistence: This indicates how long a pathogen can remain viable in the environment outside a host. A persistent pathogen can survive for an extended period (potentially months), while a non-persistent pathogen remains viable for only a limited time (days or weeks). Some protozoa can form resilient cysts that survive for months. Helminths are typically persistent and can survive for years in the environment.
The Host
The host refers to the individual (person) or animal carrying the infection caused by the pathogen.
The host plays a significant role in the transmission cycle, serving as both a place where pathogens reside (a reservoir) and a source from which they can spread.
Hosts can be classified into two types:
Definitive host: This host harbors the adult or sexually reproductive stage of the pathogen. Humans are typically the definitive hosts for the infections discussed.
Intermediate host: This host is infected with the larval or asexual developmental stage of the pathogen. Humans can act as intermediate hosts for some infections, such as Cysticercosis and hydatid disease. Among the pathogens mentioned, only helminths commonly involve both definitive and intermediate hosts. Vectors, in a functional sense, act as intermediate hosts for certain protozoa during transmission.
Zoonoses: These are infections that can naturally spread from animals to people. Over half of the infections noted in public health contexts are zoonoses. They often originate within animal populations, with human infection occurring incidentally. A primary challenge with zoonoses is that the animal population acts as a continuous reservoir, posing an ongoing risk to humans even if human cases are controlled. Managing zoonoses frequently requires control measures directed at animal hosts, such as reducing populations of rodents or immunizing domestic animals.
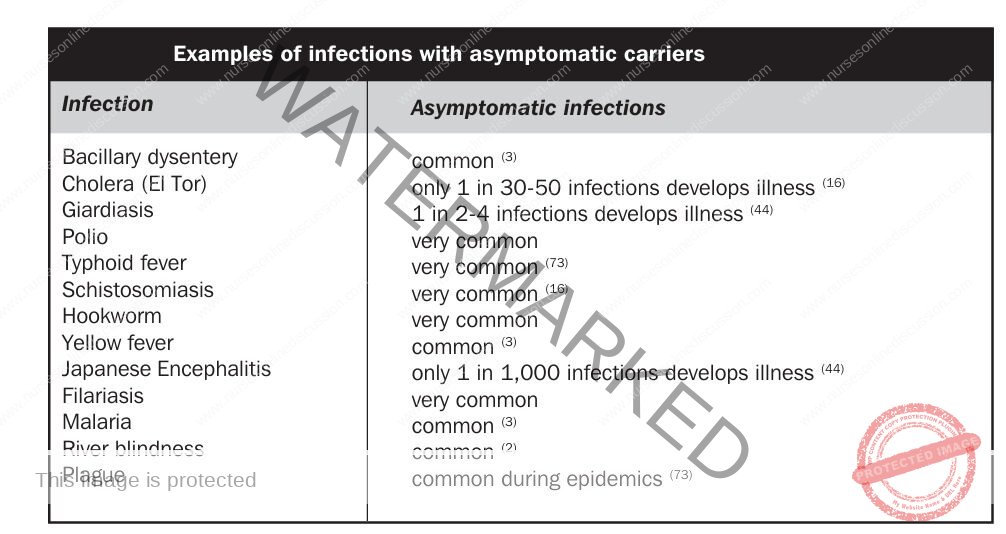
- Carriers: Individuals or animals who are infected and can transmit the pathogen but do not exhibit obvious signs of illness are called carriers, or sometimes asymptomatic carriers. Their symptoms may be mild or entirely absent. Carriers are very common in many infections and play a significant role in pathogen transmission, often being difficult to identify. Carriers can shed pathogens for a brief duration (transient carriers) or for a prolonged period (chronic carriers). Incubating carriers are infected and can spread the pathogen before their own symptoms appear. Convalescent carriers continue to shed pathogens after they have recovered from the illness. Infections frequently associated with asymptomatic carriers include cholera, typhoid fever, and schistosomiasis.
Other Reservoirs of Pathogens
Apart from infected hosts, other places can serve as reservoirs. Some hardy pathogens can survive in the environment for substantial lengths of time; for instance, eggs of roundworms can remain viable in soil for years.
Intermediate hosts can also be important storage points for pathogens, and some helminths can even multiply within them.
Vectors are often infectious for their entire lifespan, and for some pathogens, the infection can be passed down through generations of vectors to their offspring (transovarial transmission).
Certain pathogens can complete their entire life cycle independent of a host organism, such as threadworms and some types of bacteria spread via faeces and mouth.
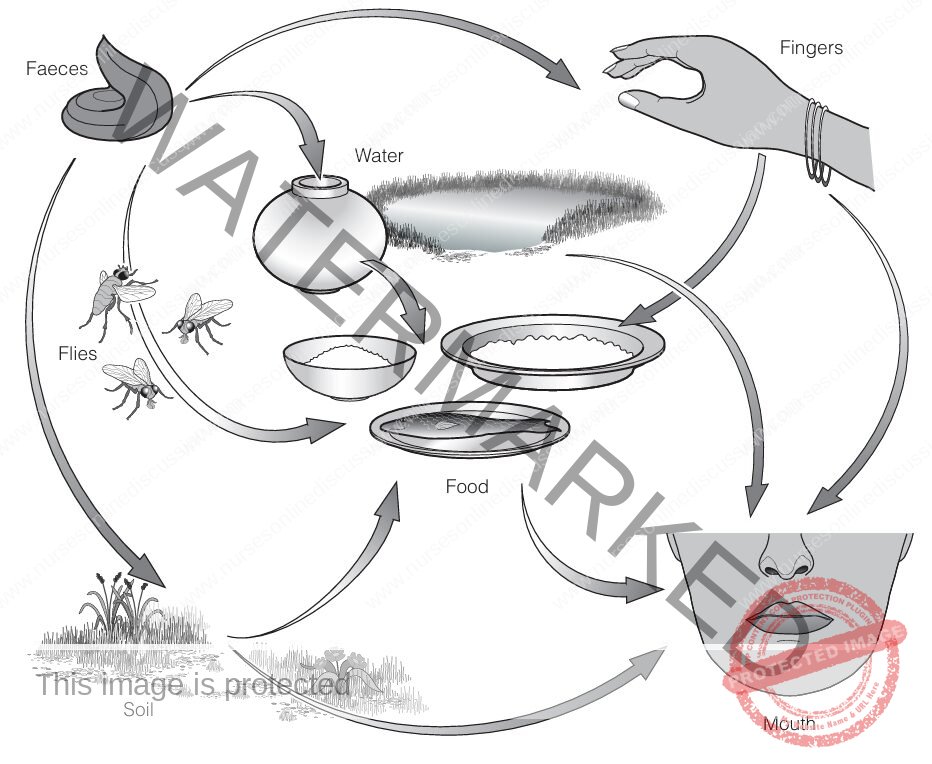
Transmission of Disease
Pathogens must successfully leave their current host, navigate a pathway to a new vulnerable host, and enter their body. Water and environmental sanitation (WES) strategies aim to lessen the risk during this transmission stage. Understanding the routes of transmission is fundamental for WES professionals to determine the most effective control measures.
Infections can be grouped based on how they are transmitted, as diseases with similar cycles can often be addressed by similar preventive methods.
Important terms related to transmission or classification include:
Food-borne infections: Diseases transmitted by consuming food contaminated with the pathogen.
Vector-borne infections: Transmitted through biological vectors, which are typically arthropods like mosquitoes, ticks, or mites. The pathogen undergoes development or multiplication within the vector before transmission occurs. Mechanical vectors, such as flies or cockroaches, are not classified as biological vectors because they merely transport the pathogen without it developing within them.
Water-borne infections: Diseases spread by drinking water that contains the pathogen.
Water-washed infections: Transmission is reduced or prevented by improving personal hygiene and increasing the availability and use of water for washing.
Infections follow either direct or indirect transmission pathways.
Direct transmission: The pathogen can infect a susceptible host immediately after leaving the current host, without needing a developmental stage in the environment, an intermediate host, or a vector. For pathogens shed in faeces, these are the non-latent agents. Disease categories with direct transmission include:
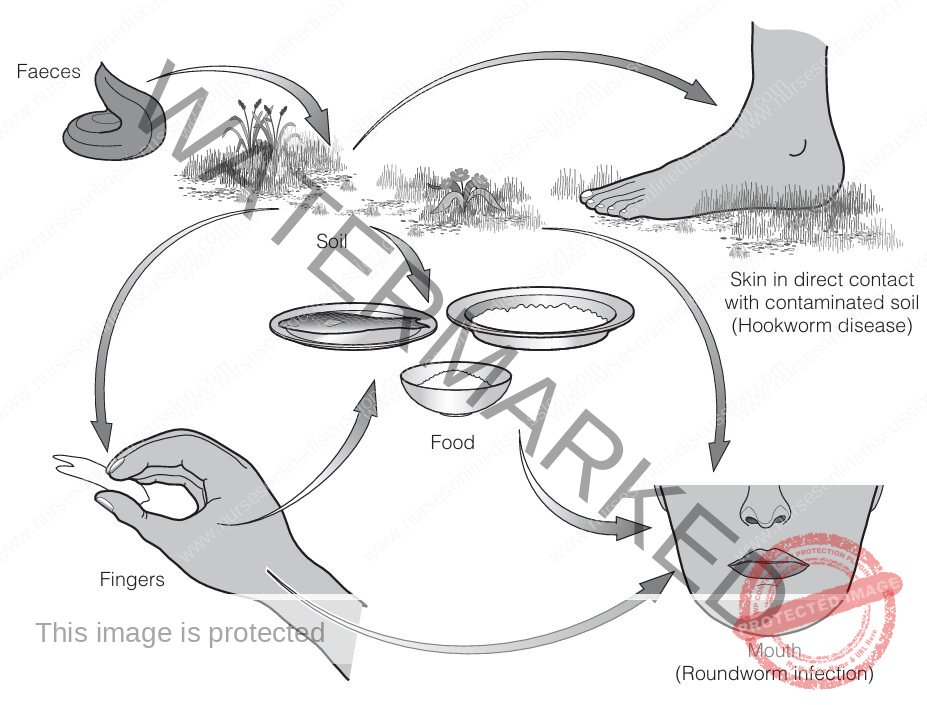
Faecal-oral infections: Pathogens exit the host via faeces and are then ingested orally. Transmission occurs through contact with contaminated hands, food, water, soil, or via mechanical vectors like flies. These diseases can be food-borne, water-borne, and water-washed. Examples include cholera and typhoid fever.
Leptospirosis: The pathogen is shed in the urine of animal hosts (commonly rats). Humans are typically infected through contact of skin, especially damaged skin, with contaminated water, soil, or vegetation.
Infections of direct contact: Affecting the skin or eyes, these pathogens are transmitted directly via contaminated hands, clothing, flies, or other fomites. Entry occurs through the skin or mucous membranes. These infections are water-washed and strongly linked to inadequate personal hygiene. Examples include conjunctivitis and scabies.
Indirect transmission: The pathogen requires a phase of development or maturation outside the immediate host before it can infect a new host. This necessary development takes place in a specific intermediate host, vector, or type of environment. For pathogens found in faeces, these are the latent agents. This reliance on a specific organism or environment provides distinct targets for prevention efforts, such as vector control programs. Disease categories with indirect transmission include:
Soil-transmitted helminths: These parasitic worms exit the body as eggs or larvae and must develop in the soil to become infectious. Entry into humans can be via skin penetration (e.g., hookworms) or by ingesting contaminated soil or food (e.g., roundworms). Ingestion methods are considered food-borne and water-washed.
- Water-based helminths: Pathogens are shed via excreta and require development within intermediate hosts that live in freshwater. Transmission necessitates excreta reaching freshwater containing suitable hosts. This category includes schistosomiasis, which develops in freshwater snails and enters humans through skin contact in contaminated water. It also includes infections involving two water-based intermediate hosts (e.g., snails or copepods, followed by fish, crabs, or aquatic plants), with human infection resulting from eating the undercooked second intermediate host.
Beef/pig tapeworm infection: Eggs are passed in human faeces and must be consumed by cattle or pigs, where they develop within their tissues. Human infection occurs by eating undercooked beef or pork containing the infective stage. A complication, cysticercosis, can occur if humans directly ingest pig tapeworm eggs, leading to transmission similar to faecal-oral routes.
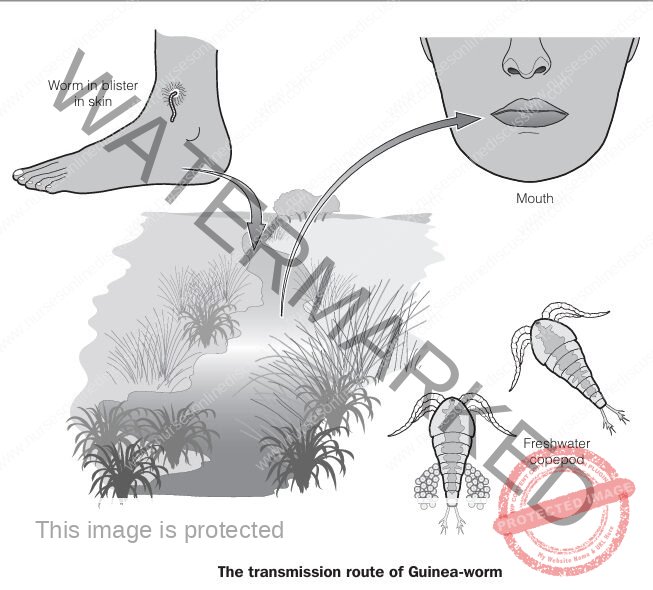
Guinea-worm infection: Larvae are released into water from a blister on the infected person’s skin and then infect tiny crustaceans called copepods (Cyclops), where they mature. People become infected by drinking water containing infected Cyclops. This disease is considered water-borne.
- Vector-borne diseases: Transmitted by arthropod vectors (insects, ticks, mites). The pathogen circulates in the host’s blood or skin and is picked up by the vector when feeding. It then develops and often multiplies inside the vector, which becomes infectious. Humans are typically infected by the vector’s bite. Animal hosts often serve as important reservoirs for these diseases. Examples include malaria and yellow fever.
The Environment
The environment encompasses everything surrounding the pathogen during its transmission journey. WES interventions frequently involve altering the environment to lessen the likelihood of transmission.
Key environmental factors include:
Climate: Plays a crucial role, influencing the presence and activity of vectors and intermediate hosts, which depend on rainfall and temperature. Conditions like direct sunlight, dryness, and high temperatures generally decrease the survival time of pathogens. Many infections show seasonal patterns linked to climate. Climate also affects human behaviour, such as increased crowding in cold weather, which can favor infections spread by close contact like body lice.
Landscape: Physical features, both natural and constructed, such as mountains, rivers, or reservoirs. Landscape influences local climate (micro-climate), the availability of water, and vegetation types. Human modifications to the landscape, such as building artificial reservoirs or irrigation systems, can increase disease risk by creating suitable habitats for vectors or intermediate hosts.
Human surroundings: Closely related to the landscape but on a smaller, more manageable scale (e.g., within a neighbourhood, village, or household). These are environments shaped by people altering natural elements. Poorly managed human surroundings, specifically relating to water supply, the handling of human waste (excreta), wastewater, solid waste, and control of vectors and intermediate hosts, can promote disease transmission.
Human behaviour: This is complex and shaped by cultural norms, social status, available resources, and political factors. Simply having access to safe water or sanitation facilities does not guarantee they will be used effectively; the facilities must be acceptable and perceived as beneficial improvements. Changes in behaviour leading to improved hygiene practices are considered the most significant factor in reducing the transmission of WES-related diseases, often having a greater impact than structural improvements alone. Identifying and encouraging changes in behaviour that currently facilitate disease transmission should be a priority for WES specialists.
The Susceptible Person or Animal (Future Host)
A pathogen’s ability to successfully infect a new host depends on the number of pathogens encountered (the infectious dose) and the host’s natural ability to resist or overcome these invaders (their barriers).
Infectious dose: The minimum number of pathogens required to establish an infection in a susceptible host. This indicates how easily an infection can spread. The term is most commonly used in the context of faecal-oral infections. Infections with a low infectious dose (e.g., Bacillary dysentery, Giardiasis, requiring only 10-100 pathogens) are more likely to spread through direct person-to-person contact than those with a high infectious dose (e.g., Cholera, Typhoid, requiring millions). Control measures like improving drinking water quality or treating sewage are particularly effective against infections requiring a high infectious dose. Helminths are often considered to have a very low effective infectious dose, as even a single larva can develop into an adult worm.

Barriers of the body: These are the defense mechanisms that prevent pathogens from entering the body and causing infection.
The initial barriers include the skin, mucous membranes lining body cavities (which contain antimicrobial substances), and the acidity of the stomach. Conditions like low stomach acidity or open wounds can weaken these first lines of defense.
Beyond the initial barriers are non-specific mechanisms providing general resistance, which do not require prior exposure to the pathogen. This general resistance can be lowered by factors such as other ongoing infections, malnutrition, stress, or fatigue. Pregnancy also increases susceptibility in women.
The immune system can develop specific protection (immunity) through previous encounters with the pathogen or through vaccination. This is known as active immunity. The immune system identifies the pathogen and produces specific antibodies or cellular responses. The effectiveness and duration of this immunity vary depending on the specific pathogen and the time elapsed since exposure. Active immunity is specific to the particular pathogen that triggered it. Immunity against many bacteria and viruses often lasts for years. However, immunity acquired against different types (serotypes or strains) of the same pathogen may only protect against the specific type encountered. Immunity developed against fungi is highly variable. Immunity against protozoa is often maintained only through repeated exposure or vaccinations. Generally, significant protective immunity is not built up against helminthic infections.
Passive immunity is provided by receiving antibodies produced elsewhere, such as antibodies transferred from a mother to her baby via the placenta or through the administration of antibodies (e.g., via antiserum). This type of immunity is temporary, typically lasting for days to a few months.
An individual or animal lacking sufficient protective barriers (due to poor general resistance or low specific immunity) is considered susceptible to a particular pathogen. Populations weakened by poor nutrition or high rates of existing diseases are at increased risk. If a pathogen is widespread or vaccination rates are high, a large portion of the population may have some degree of immunity, and new infections may primarily affect children. Conversely, introducing a pathogen into a population with little to no prior immunity can lead to widespread outbreaks (epidemics) affecting people of all ages.
Infection Over Time
If a sufficient number of pathogens overcome the host’s defense mechanisms, the process of infection begins.
Incubation period: This is the time interval from when the pathogen first enters the body until the first noticeable signs or symptoms of the disease appear.
It is important to note that not all infections result in obvious illness; asymptomatic carriers are frequently observed.
Period of communicability: This is the duration during which an infected host is capable of shedding pathogens and transmitting the infection to others.
Latent period: This term refers to the time from when a pathogen enters the host until the host becomes infectious (capable of transmitting the pathogen). This is a distinct concept from the latency of the pathogen itself requiring environmental development mentioned earlier.
An individual can become infectious and spread the pathogen before experiencing any symptoms themselves (incubating carriers). If they continue to spread the pathogen after their illness has resolved, they are referred to as convalescent carriers.
Related Topics
Disease Causation and Prevention
Disease Transmission Cycle
Levels of Disease Prevention
Introduction to Environmental Hygiene/Sanitation
Housing
Ventilation Heating and Lighting
Safe Water Supply
Food Hygiene
Sanitation
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

