Respiratory System Conditions
Subtopic:
Otitis Media
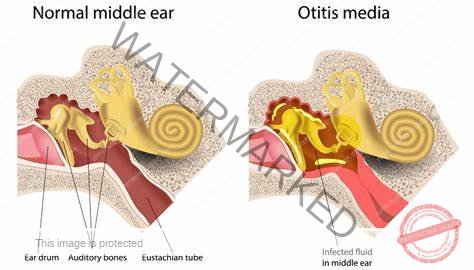
Otitis media refers to inflammation, which can be either short-term (acute) or long-lasting (chronic), affecting the middle ear. This condition is frequently encountered in children.
Acute Otitis media:
Acute otitis media is characterized by a sudden and quick development of the illness, accompanied by one or more of the following signs:
Otalgia: Ear pain.
Fever: Elevated body temperature.
Otorrhea: Discharge or fluid draining from the ear.
Recent onset of anorexia: A recent loss of appetite.
Irritability: Increased fussiness or agitation.
Vomiting: Throwing up.
Diarrhea: Loose or frequent bowel movements.
These symptoms occur alongside abnormal findings observed during an otoscopic examination (examination of the ear with an otoscope). These findings related to the eardrum (tympanic membrane) may include: loss of its normal transparency (opacity), outward swelling or protrusion (bulging), redness (erythema), and the presence of fluid in the middle ear (middle ear effusion).
Chronic otitis media:
Chronic otitis media indicates a persistent, long-term inflammation of the middle ear. It is generally defined as inflammation lasting for a minimum of six weeks and is typically linked to continuous ear discharge (otorrhea) through a hole in the eardrum (perforated tympanic membrane) or the presence of a tympanostomy tube (a small tube surgically inserted into the eardrum).
Cause
The most common bacterial culprits include:
Streptococcus pneumoniae
Haemophilus influenzae
Moraxella catarrhalis
Group A beta-hemolytic Streptococcus
Viral infections of the respiratory system can also lead to otitis media.
Additionally, enlarged tonsils or adenoids, which are lymphoid tissues located in the throat, can sometimes obstruct the Eustachian tube, a passage connecting the middle ear to the back of the nose and throat.
It’s worth noting that with appropriate antibiotic treatment, ear pain typically starts to lessen within about 8 hours.
Predisposing factors
Several factors make children more susceptible to otitis media:
Eustachian tube characteristics in children: The Eustachian tube in young children is anatomically different from that in adults. It is shorter, wider, and more horizontally oriented, making it easier for germs to travel from the throat to the middle ear.
Immature immune system: A developing immune system in children is less effective at fighting off infections.
Frequent upper respiratory infections: Common colds and other upper respiratory tract infections can often precede otitis media.
Furthermore, the tendency for infants to spend a lot of time lying down can encourage the pooling of fluids like formula in the back of the throat, potentially increasing the risk of infection reaching the middle ear via the Eustachian tube.
Signs
Common signs and symptoms of otitis media include:
Earache: Pain within the ear.
Fever: Elevated body temperature.
Abnormal eardrum appearance: The tympanic membrane may appear red and bulging. There might also be visible fluid behind the eardrum, and in some cases, pus or fluid may drain from the ear. Some individuals might experience an itchy sensation in the ear.
Irritability and restlessness: Younger children who cannot verbalize their discomfort may show increased fussiness, agitation, cry more than usual, and sometimes pull or tug at their affected ear.
Tenderness behind the ear: The area over the mastoid bone (located behind the ear) may be sensitive to the touch.
Pus discharge: If there is ear drainage, it typically lasts for less than 14 days in acute cases.
Tinnitus: Ringing, buzzing, or other noises in the ear.
Bulging of the eardrum: The tympanic membrane may be visibly pushed outward due to pressure from fluid buildup.
Hearing loss: A temporary decrease in the ability to hear.
Activities like lying down, chewing, and sucking can exacerbate pain by causing pressure changes within the middle ear. As a result, a child with otitis media might eat less than usual or have difficulty sleeping.
During a physical examination, the eardrum often appears inflamed and red, and the mastoid process might be tender upon palpation.
Other general signs of illness, such as a high temperature (fever) of 38°C (100.4°F) or higher and a lack of energy, may also be present.
Babies with ear infections may exhibit a combination of being hot to the touch and generally irritable. Because infants cannot clearly communicate the source of their discomfort, diagnosing the problem can sometimes be challenging.
Pathophysiology
The ear, responsible for both hearing and maintaining balance, is anatomically divided into three sections: the outer ear, the middle ear, and the inner ear.
The process of hearing begins when sound waves traveling through the air reach the outer ear, specifically the pinna, which is the visible part of the ear. These sound waves then travel from the pinna, through the ear canal, and arrive at the middle ear. The middle ear contains the eardrum (a thin, tightly stretched membrane) and three very small bones known as ossicles (malleus, incus, and stapes). When sound waves strike the eardrum, it vibrates. These vibrations are then amplified by the ossicles and transmitted to the inner ear.2
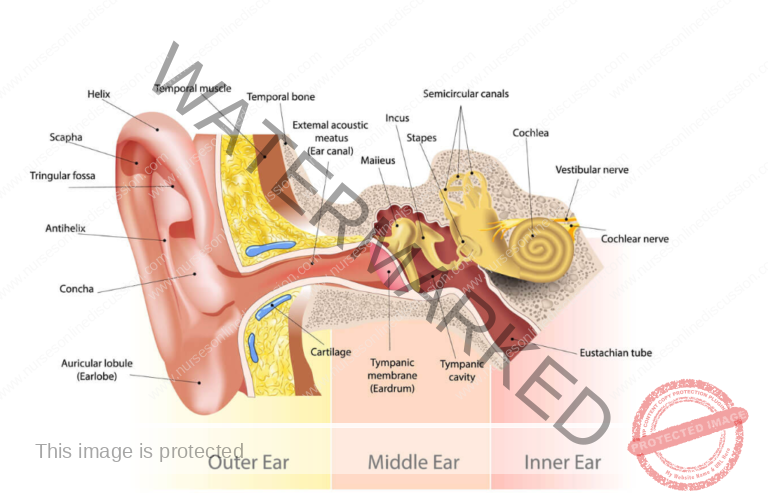
The inner ear is responsible for transforming these mechanical vibrations into electrical signals. These signals are then sent to the auditory nerve, which connects directly to the brain. When these nerve impulses reach the brain, they are interpreted as sound.
The Eustachian Tube
- For the middle ear to function optimally, the pressure within it needs to be the same as the air pressure in the external environment. This pressure regulation is the role of the Eustachian tube, a small passage connecting the middle ear to the nasopharynx, the upper part of the throat behind the nose.
- By allowing air to enter the middle ear, the Eustachian tube ensures that the air pressure inside matches the air pressure outside. You might experience this equalization as a “popping” sensation in your ears when you yawn or swallow; this indicates that the Eustachian tubes are actively adjusting the air pressure in your middle ears. The Eustachian tube also serves as a drainage pathway, allowing mucus and other debris to move from the middle ear into the throat.
- Sometimes, the Eustachian tube can become blocked or fail to work properly. This can happen during a cold or an allergy, where inflammation and swelling can thicken the lining of the Eustachian tube or lead to a buildup of mucus within it. This blockage traps fluid within the normally air-filled middle ear.
- Otitis media often develops as a consequence of Eustachian tube dysfunction.
- The Eustachian tube, connecting the middle ear to the nasopharynx, is typically closed, narrow, and angled downwards. This configuration usually prevents microorganisms from the pharyngeal cavity from entering the middle ear space.
- It opens intermittently to allow for the drainage of normal secretions produced by the middle ear lining and to equalize the air pressure between the middle ear and the external environment.
- When drainage is impaired due to a blocked Eustachian tube, a pathological condition arises because secretions become trapped within the middle ear.
Diagnosis/Investigations
History taking: Gathering information about the patient’s symptoms and medical history.
Pus swab for microscopy, culture and sensitivity: If there is ear discharge, a sample can be taken to identify the specific bacteria causing the infection and determine the most effective antibiotics.
Physical examination of the ear using Otoscope: A visual inspection of the ear canal and eardrum is crucial for diagnosis.
To perform the ear examination, an otoscope is utilized. This handheld device, similar in appearance to a small flashlight, is equipped with a magnifying lens and a light source at its tip. It allows healthcare professionals to visualize the internal structures of the ear.
Other tests or investigations that may be performed include:
Tympanometry: This test assesses the movement and flexibility of the eardrum in response to changes in air pressure within the ear canal. A healthy eardrum should move freely when the air pressure changes. During the test, a probe is gently inserted into the ear canal, and it changes the air pressure at regular intervals while also emitting a sound into the ear. The probe measures how much sound is reflected back from the eardrum and how changes in air pressure affect these sound reflections. If less sound is reflected back when the air pressure is high, it often suggests the presence of fluid or infection in the middle ear.
A computer tomography (CT) scan: This imaging technique might be employed if there’s a concern that the infection has spread beyond the middle ear. A CT scan utilizes X-rays taken from multiple angles and a computer to create detailed cross-sectional images of the skull.
Tympanocentesis: This procedure involves using a small needle to withdraw fluid from the middle ear. The collected fluid can then be sent to a laboratory to identify the specific bacteria or viruses responsible for the infection.
Management
Amoxicillin is typically the first-line antibiotic prescribed for otitis media.
For patients with a confirmed penicillin allergy, trimethoprim-sulfamethoxazole is often used as an alternative.
Second-line antibiotics that may be considered if the initial treatment is ineffective or if there are specific circumstances include:
Amoxicillin/clavulanate
Ampicillin/sulbactam
A cephalosporin antibiotic
Children under the age of 2 years are considered to be at a higher risk for experiencing repeated episodes of otitis media, developing chronic otitis media, and having serious complications from the infection.
Antibiotics may be prescribed as follows: For adults, capsules of Amoxicillin 500mg four times a day (QID) for 5 days. For children, the dosage is typically 15mg per kilogram of body weight.
Erythromycin tablets 500mg four times a day (QID) for 5 days can be used in adults who have an allergy to penicillin antibiotics.
Analgesics (pain relievers) are often recommended to manage pain associated with otitis media. Examples include: Paracetamol 1 gram three times a day (tds) for 3 days, OR Ibuprofen tablets 400mg three times a day (tds) for 3 days.
Topical antibiotic ear drops, such as Gentamicin, can be applied directly into the ear canal. The usual application is 2 drops three times a day (tds) for 5 days, typically after gently cleaning any discharge from the ear (ear wicking).
A follow-up review is usually scheduled after 5 days of treatment. If the eardrum is still inflamed (red), the treatment regimen may be repeated.
Surgical Management
Grommets: For children who experience frequent and severe middle ear infections, small tubes, known as grommets or tympanostomy tubes, can be surgically inserted into the eardrum. These tubes help to drain fluid from the middle ear and ventilate the space.
Myringotomy: This is a surgical procedure where the surgeon makes a tiny incision in the eardrum. This can help to relieve pressure within the middle ear and allows for the drainage of excess fluid. In some instances, a myringotomy is followed by the insertion of a grommet.
Tympanotomy: This surgical procedure involves creating a surgical opening in the eardrum, also known as the tympanic membrane. The purpose is to facilitate the drainage of infected fluid from the middle ear. Surgical tubes may be implanted into the eardrum to provide ongoing drainage. This procedure might be considered when there is scarring or minimal damage to the eardrum, or in cases of deafness or hearing impairment.
Myringoplasty: This surgical procedure aims to repair a hole or perforation in the eardrum. The repair is achieved by placing a graft over the perforation. The graft material can be a small piece of tissue taken from another part of the patient’s body or a specially designed gel-like material.
Tympanoplasty: This more extensive surgical procedure involves the repair of damaged ossicles, the tiny bones in the middle ear. This may involve replacing the damaged ossicles with a small piece of bone or a prosthetic device.
Nursing care
Applying a warm compress, like a hot water bag, to the affected ear while the child lies on that side can help to ease the discomfort, particularly during episodes of acute pain. The warmth can provide soothing relief.
Using a cold compress, such as an ice bag, applied to the affected ear may be helpful in reducing swelling (edema) and inflammation in between episodes of acute pain. The coolness can help constrict blood vessels and minimize swelling.
If there is discharge from the ear, the external ear canal should be cleaned regularly using sterile cotton swabs. These swabs can be used dry or moistened with hydrogen peroxide to help remove any drainage.
To prevent skin irritation (excoriation) around the outer ear due to discharge, frequent gentle cleaning is important. Applying a protective barrier cream like zinc oxide to the skin around the ear opening can help shield it from the irritating effects of the drainage.
If the child has a tympanostomy tube (grommet) in place, special care is needed. It’s crucial to prevent water from entering the middle ear as this could introduce bacteria and lead to infection. Specific instructions on bathing and swimming precautions should be followed.
Educate the family on how to care for the child with otitis media. It’s important to inform them about potential complications of acute otitis media, such as conductive hearing loss, so they understand the importance of treatment and follow-up.
Provide emotional support to both the child, who may be experiencing pain and discomfort, and their family, who may be worried. Reassurance and clear explanations can help alleviate anxiety.
Ensure the patient gets adequate rest by encouraging or enforcing complete bed rest, especially during the acute phase of the infection. This allows the body to focus on healing.
Encourage the patient to drink plenty of fluids. Adequate hydration is important for overall health and can help thin mucus secretions.
If there is any discharge from the ear, it’s important to keep the ear dry. This can be done by a technique called ear wicking, where a small roll of sterile cotton is used to gently absorb the pus from the ear canal.
Complications
Meningitis: The infection can spread to the membranes surrounding the brain and spinal cord, causing a serious and potentially life-threatening condition.
Mastoid abscess: A collection of pus can form in the mastoid bone, which is located behind the ear.
Acute mastoiditis: This is an infection of the mastoid bone itself, often developing as a complication of untreated or poorly treated otitis media.
Facial nerve damage leading to facial palsy: The facial nerve passes through the middle ear, and inflammation or infection can damage it, causing weakness or paralysis of the facial muscles.
Infection in adjacent areas: The infection can spread to nearby tissues and organs, such as the tonsils or the nasal passages.
Brain abscess: In rare but serious cases, the infection can spread to the brain itself, forming a collection of pus.
Labyrinthitis: The infection can extend to the inner ear, affecting balance and hearing.
Sinus thrombosis: A blood clot can form in the venous sinuses of the brain, which can be a serious complication.
Septicemia: The infection can enter the bloodstream, leading to a systemic and life-threatening condition (blood poisoning).
Prevention
Provide health education to patients and families, including informing them about how to recognize the signs and symptoms of otitis media, such as ear discharge.
Ensure early diagnosis and prompt treatment of acute otitis media and upper respiratory tract infections, as these can often lead to middle ear infections.
Treat infections in adjacent areas promptly. For example, if a patient has tonsillitis, addressing this infection can help prevent the spread of bacteria to the middle ear.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

