Gynecological Nursing
Subtopic:
Ectopic pregnancy
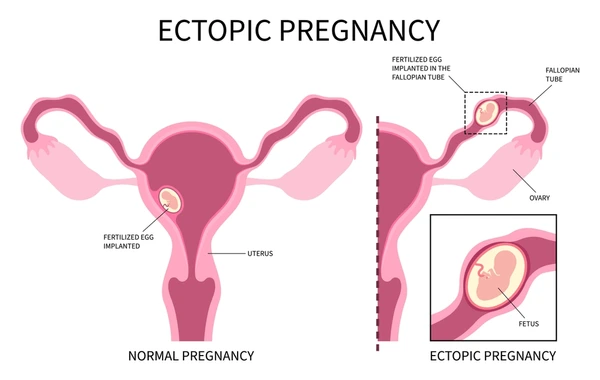
An ectopic pregnancy is a serious medical condition arising when a fertilized egg implants and begins to grow outside of the uterus. In a typical pregnancy, the fertilized egg travels into the uterus and implants within its lining. However, in an ectopic pregnancy, this process goes awry, and the implantation occurs in a location where the pregnancy cannot proceed normally to full term.
Ectopic pregnancy is defined by the implantation of the fertilized egg (ovum) at a site other than within the uterine cavity itself.
Causes of Ectopic Pregnancy:
Fallopian Tube Damage: Scars or blockages within the fallopian tubes significantly elevate the risk of ectopic pregnancy. These obstructions can result from prior infections, surgical procedures in the pelvic area, or conditions like endometriosis. Such damage impedes the normal passage of the fertilized egg, increasing the likelihood of implantation outside the uterus. Furthermore, congenital factors like unusually long fallopian tubes, which are prone to kinking, or naturally narrow fallopian tubes can also heighten this risk.
Hormonal Imbalances: Certain disruptions in hormonal levels or hormonal irregularities can disrupt the natural movement of the fertilized egg and the process of implantation. This can increase the possibility of ectopic pregnancy by interfering with the coordinated actions needed for successful uterine implantation.
History of Ectopic Pregnancy: Women who have previously experienced an ectopic pregnancy have a notably increased chance of having another ectopic pregnancy in subsequent pregnancies. This prior occurrence is a significant risk factor for recurrence.
Reproductive System Abnormalities: Structural irregularities or unusual formations within the female reproductive system can contribute to ectopic pregnancies. For instance, an abnormally shaped uterus or a fallopian tube that is not located in its typical position can create conditions that favor implantation outside the uterus.
Pelvic Inflammatory Disease (PID): Infections in the pelvic organs, such as salpingitis (inflammation of the fallopian tubes), are major contributors to ectopic pregnancy risk. PID can cause significant damage to the delicate lining of the fallopian tubes. This damage may involve the destruction or erosion of the cilia (tiny hair-like structures that aid egg transport) and the formation of adhesions (scar tissue) that impede the muscular contractions (peristalsis) necessary for proper egg movement through the tubes.
Tumors: Growths or masses located near the fallopian tubes can exert pressure on the tubes. This external pressure can cause a partial or complete blockage within the fallopian tube, hindering the egg’s passage and raising the risk of ectopic implantation.
Endometriosis: This condition involves the growth of tissue similar to the uterine lining (endometrium) outside the uterus. Endometriosis can affect the fallopian tubes and surrounding pelvic organs, creating an environment that increases the likelihood of ectopic pregnancy through inflammation and anatomical distortion.
Repeated Induced Abortions: Having multiple induced abortions may, in some cases, increase the risk of subsequent ectopic pregnancies. This is potentially linked to possible damage to the uterine lining or fallopian tubes during these procedures, although the exact mechanisms are complex and still under investigation.
Tubal Surgery: Surgical procedures performed on the fallopian tubes, whether for sterilization reversal or to address other tubal issues, can lead to the formation of adhesions either inside the tube (intraluminal) or outside the tube (extraluminal). These adhesions can disrupt normal tubal function and elevate the risk of ectopic pregnancy.
Intrauterine Devices (IUDs): While IUDs are highly effective at preventing intrauterine pregnancies, if pregnancy does occur with an IUD in place, there is a slightly increased relative risk that it will be ectopic. This is because IUDs primarily prevent implantation within the uterus, but do not prevent fertilization or implantation outside the uterus.
Sites of Ectopic pregnancy
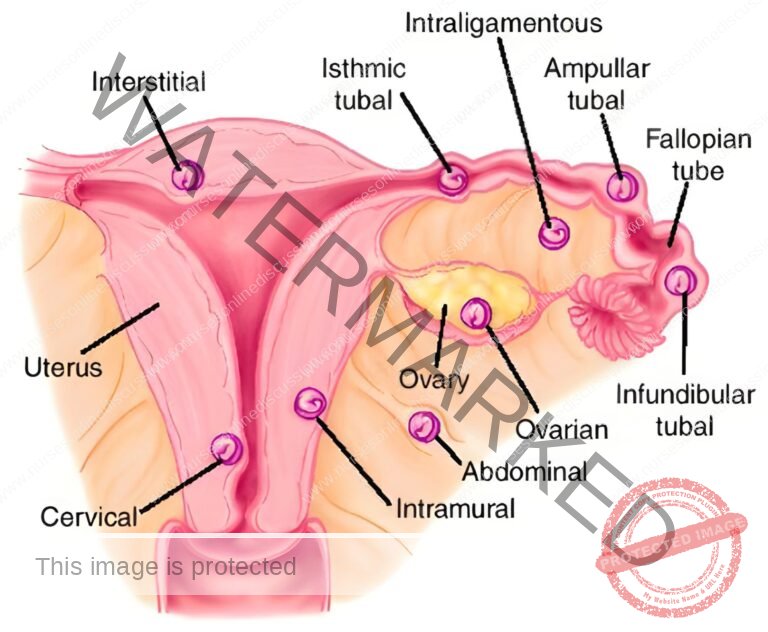
The most frequent location for an ectopic pregnancy is within the uterine tube, but it can also occur in other areas such as the broad ligament, the ovary, and the abdominal cavity.
Fallopian tubes (most common): This is the predominant site for ectopic pregnancies.
Ovary: Implantation can occur on the surface of the ovary itself, though less frequently than in the tubes.
Intraperitoneal abdominal cavity: In rare instances, the fertilized egg may implant within the abdominal cavity, outside of the reproductive organs.
Cervix: Implantation in the cervical canal is a very uncommon location for ectopic pregnancy.
Tubal Pregnancy
Tubal pregnancy specifically refers to the condition where a fertilized egg embeds itself and develops within one of the fallopian tubes.
Specific Locations within the Fallopian Tube for Tubal Pregnancy:
Ampulla (most common): The ampulla, the widest section of the fallopian tube, is the most typical site for tubal ectopic pregnancies.
Isthmus (most dangerous): Implantation in the isthmus, the narrowest part of the fallopian tube close to the uterus, is particularly risky. Due to the limited space, rupture can happen very early, sometimes even before a woman is aware of her pregnancy.
Fimbriated end (infundibulum) – rare: Ectopic pregnancy at the fimbriated end, or infundibulum (the funnel-shaped opening of the tube near the ovary), is an infrequent occurrence.
Interstitial part (rare): Implantation in the interstitial part of the fallopian tube, the section that passes through the uterine wall, is also rare.
Possible Outcomes of tubal Pregnancy
Tubal pregnancies can have different resolutions depending on the development and location of the implanted egg.
Tubal mole: In this outcome, the developing embryo (zygote) ceases to live but remains within the fallopian tube, often surrounded by a blood clot. This situation can lead to a slow, ongoing ectopic pregnancy that may leak blood gradually.
Tubal abortion: Here, the developing embryo detaches from the lining of the fallopian tube and is expelled through the fimbriated end. The embryo may not survive this process. However, in some cases, it can re-implant on abdominal organs and continue to grow, potentially developing into an abdominal pregnancy, which, in rare scenarios, can progress towards term.
Tubal rupture: As the embryo grows, the fallopian tube may become too stretched and unable to accommodate the increasing size. This can result in the tube tearing or rupturing. Tubal rupture is a critical obstetric emergency because it leads to significant internal bleeding into the abdominal cavity and can cause shock.
Tubal erosion: In this scenario, the developing embryo invades and erodes through the wall of the fallopian tube. This erosion causes bleeding into the abdominal cavity, as the embryo disrupts the tube’s tissue.
Signs and Symptoms of Ectopic Pregnancy (Tubal Rupture)
The signs and symptoms, particularly in the case of tubal rupture, are critical for prompt diagnosis and intervention.
Information Obtained from Patient History:
History of amenorrhea (missed period) of 6 – 10 weeks: Often, women experience a period of absent menstruation, similar to early intrauterine pregnancy, typically lasting six to ten weeks.
Patient complaints of feeling faint, dizziness, thirst, and vomiting: These symptoms can indicate early pregnancy, but in the context of ectopic pregnancy, they can also be signs of internal bleeding and early shock.
Patient reports acute abdominal pain: The pain is typically located in the iliac fossa (lower abdomen), often described as colicky (cramping and fluctuating) in nature. The pain may radiate to the shoulder, especially when lying down. This referred pain occurs because blood in the abdominal cavity irritates the diaphragmatic nerve and the peritoneum (lining of the abdominal cavity).
Findings on Physical Examination:
Signs of pregnancy may be present: Physiological changes associated with pregnancy, such as darkening of the areola (the area around the nipple), might be observed.
Signs of shock are evident: These include cold, clammy skin, a rapid and weak (thready) pulse, low blood pressure (hypotension), and potentially a low body temperature. These are indicators of significant blood loss and circulatory compromise.
Patient appears anxious and restless: These are common responses to pain and internal distress.
Pallor (paleness) of the mucous membranes: This is a sign of anemia and blood loss, visible in the lining of the mouth and eyelids.
Findings on Abdominal Palpation:
Abdominal tenderness: There is pain upon touching the abdomen, particularly on the side affected by the ectopic pregnancy.
Abdominal muscle rigidity: The abdominal muscles may become tense and stiff. This guarding is an involuntary response to protect the painful area.
Abdominal distension: Swelling or bloating of the abdomen can occur due to the accumulation of blood within the abdominal cavity.
Findings on Vaginal Examination:
Discrepancy between bleeding amount and patient’s condition: The amount of vaginal bleeding may seem relatively light and not fully explain the severity of the mother’s symptoms and signs of shock.
Tenderness on cervical motion: Pain is elicited when the cervix is moved during the examination.
Palpable mass in the lateral fornix of the vagina: A tender mass may be felt to the side of the uterus in the vaginal fornix (the recesses where the cervix meets the vaginal wall).
Painful mass in the Pouch of Douglas: A tender mass might be felt in the Pouch of Douglas (the space behind the uterus and in front of the rectum, accessible through the posterior vaginal fornix), indicating blood accumulation.
Dark brown blood on the examining finger: Dark blood may be noted upon removal of the examining finger after vaginal examination, suggesting old blood from internal bleeding.
Investigations:
Diagnostic tests are crucial to confirm ectopic pregnancy and rule out other conditions.
Ultrasound scan: An ultrasound is a primary diagnostic tool. It can reveal a ruptured ectopic pregnancy and the presence of blood collection in the affected area. Ultrasound is usually definitive in confirming the diagnosis.
Blood tests for Hemoglobin (Hb), grouping, and cross-match: Blood tests are essential to assess the level of blood loss (hemoglobin) and to prepare for potential blood transfusion (grouping and cross-match).
Complete Blood Count (CBC): A CBC will show a low hemoglobin level, reflecting blood loss.
Pregnancy test: A pregnancy test will be positive, confirming pregnancy but not its location.
Culdocentesis (Puncture of the Pouch of Douglas): In emergency situations where ultrasound is not immediately available, a needle puncture into the Pouch of Douglas (culdocentesis) can be performed. The aspiration of fresh blood strongly suggests hemoperitoneum (blood in the peritoneal cavity) due to a ruptured ectopic pregnancy.
Differential Diagnosis:
It’s important to differentiate ectopic pregnancy from other conditions with similar symptoms.
Salpingitis: Inflammation of the fallopian tubes (salpingitis) can mimic ectopic pregnancy, especially if associated with irregular menstrual bleeding.
Appendicitis: Inflammation of the appendix can cause lower abdominal pain, similar to ectopic pregnancy.
Abortion (miscarriage): A spontaneous abortion can present with pain and bleeding, but typically occurs within the uterus.
Twisted ovarian cyst: Torsion of an ovarian cyst can cause acute pelvic pain, resembling ectopic pregnancy.
Urinary tract infection (UTI): While UTI typically presents with urinary symptoms, lower abdominal pain can sometimes be a feature.
Management of Ectopic Pregnancy
Management strategies differ depending on the setting, initially at a health center and subsequently in a hospital.
Management in a Health Center (Initial Emergency Care):
At the health center level, the immediate priority is to stabilize the patient and arrange urgent transfer to a hospital. Ectopic pregnancy, especially if ruptured, is a life-threatening emergency, and rapid action is essential.
Aims at the Health Center:
To prevent shock: Addressing blood loss and circulatory collapse is paramount.
To relieve pain: Managing pain can improve patient comfort and reduce anxiety.
To reassure the patient: Providing calm and supportive communication can alleviate patient distress.
Steps at the Health Center:
Admission (Temporary): Admit the patient to a gynecology ward (if available, or any appropriate area). Briefly obtain essential history, conduct a general and focused physical examination, including abdominal and vaginal assessment. Formulate a preliminary diagnosis.
History Taking: Collect relevant histories, including personal, social, surgical, medical, and obstetric history. Obtain details of the current condition’s onset and progression.
Examination: Perform a focused physical examination from head to toe to assess for anemia, dehydration, and signs of shock.
Observation: Monitor and record vital signs: temperature, pulse, respiration, and blood pressure to assess organ function and stability.
Resuscitation (Initiation): Start intravenous fluid resuscitation with normal saline. Administer morphine 15mg intramuscularly for pain relief. Elevate the foot of the bed (Trendelenburg position) to promote blood flow to vital organs.
Transport Arrangement: Immediately arrange for safe and rapid transport to a hospital equipped for surgical management. Inform the patient and family about the diagnosis, the need for urgent hospital transfer, and the reasons for this decision.
Transfer Procedure: Clearly explain the transfer plan to the patient and family. Prepare a detailed referral note documenting the time of admission, treatment given at the health center, the patient’s condition upon arrival and at the time of transfer. Organize transportation. A midwife or healthcare provider should ideally escort the patient during transfer and provide a direct handover to the hospital staff.
Treatment Continuation during Transfer: Continue intravenous normal saline infusion during transport to manage or prevent shock. Administer pain relief (morphine or pethidine) as prescribed.
Nursing Care during Transfer: Cleanse the vulva with antiseptic solution and apply a sterile sanitary pad to manage vaginal bleeding. Send the patient to the hospital with the written referral note, detailing the patient’s presentation, condition at admission and transfer, and treatment provided.
Hospital Management
Hospital care for ectopic pregnancy is a gynecological emergency that requires prompt, coordinated action.
Aims in the Hospital:
To treat anemia: Correcting blood loss and restoring adequate hemoglobin levels is crucial.
To prevent or treat shock: Aggressively manage circulatory instability and shock due to internal bleeding.
To reassure the patient: Provide psychological support and alleviate anxiety.
To prevent complications: Minimize the risk of both immediate and long-term sequelae of ectopic pregnancy and its treatment.
Steps in Hospital Management:
Admission (Hospital Ward): Admit the patient to a well-ventilated, quiet room and prepare a warm admission bed. Establish a therapeutic nurse-patient relationship to provide emotional support.
History Taking (Comprehensive): Obtain detailed medical histories from the patient (if conscious and able) or from family members (collateral history if the patient is unable to provide information). Inquire about social, medical, surgical, obstetric, and gynecological history. Focus particularly on the history of the presenting complaint, including onset of symptoms, amount of vaginal bleeding, location and nature of pain, presence of vomiting, and any prior treatments. Estimate the weeks of amenorrhea.
Physician Notification: Immediately inform the attending physician about the patient’s arrival and clinical status.
General Examination (Thorough): Perform a complete physical examination from head to toe to comprehensively assess for anemia, shock, dehydration, and any other relevant findings.
Observation (Vital Signs): Continuously monitor and record vital signs: temperature, pulse, respiration rate, and blood pressure.
Investigations (Diagnostic Confirmation): Upon the doctor’s order, initiate the following investigations:
Hemoglobin estimation: To assess the severity of anemia and blood loss.
Blood group and cross-matching: To prepare for potential blood transfusion.
Pregnancy test (if not already done): To confirm pregnancy if uncertain, although clinical presentation is highly suggestive.
Ultrasound scan (Transvaginal or abdominal): To definitively confirm the diagnosis of ectopic pregnancy, locate its site, and assess for rupture and hemoperitoneum.
Urinalysis: To rule out urinary tract infection as a differential diagnosis.
Resuscitation (Aggressive): Continue intravenous fluid resuscitation with normal saline to prevent or treat shock. Administer morphine 15mg intramuscularly for pain relief as prescribed. Manage shock aggressively with intravenous fluids and monitoring of fluid balance. Maintain a fluid balance chart to track input and output.
Blood Transfusion: Administer blood transfusion as clinically indicated based on hemoglobin levels and the patient’s hemodynamic status.
Pain Relief (Analgesia): Provide analgesics, such as morphine, as prescribed by the physician to manage pain effectively.
Pre-operative Care:
Surgical intervention is usually required for ectopic pregnancy.
Preparation for Theater:
Nursing Care Pre-operatively:
Give the patient a bed bath.
Provide a clean theatre gown.
Monitor and record vital signs immediately pre-operatively. Collect all patient charts and records for transport to the operating room.
Arrange for patient transfer to the operating theatre.
Explain the nature of the planned surgery to the patient and obtain informed consent.
Reassure the patient to reduce anxiety and fear.
Inform the operating room staff about the pending patient and her condition.
Insert an intravenous line for continuous fluid infusion during surgery.
Perform vulval swabbing with antiseptic solution to minimize the risk of surgical site infection.
Insert a urinary catheter to drain the bladder and monitor urine output during surgery. Commence a fluid balance chart.
Insert a nasogastric tube for aspiration of stomach contents to prevent aspiration during anesthesia, or administer an antacid (e.g., magnesium trisilicate) to reduce stomach acidity.
Administer pre-medication as prescribed, such as atropine, to reduce respiratory secretions during anesthesia.
Re-check and record vital signs, comparing them with baseline observations.
Compile all clinical charts, notes, and investigations, and transport the patient carefully to the operating theatre, dressed in a theatre gown.
Upon arrival in the operating room, provide a comprehensive patient report to the theatre nurse.
Ensure that 1-2 units of blood are readily available, cross-matched and booked for potential transfusion.
Hand over patient care to the theatre staff. If possible, the ward nurse should stay with the patient until anesthesia induction.
Return to the ward and prepare a post-operative bed, ensuring all necessary equipment is ready.
In Theatre (Surgical Procedure):
Laparotomy (open abdominal surgery) or laparoscopy (minimally invasive surgery) is performed.
Salpingectomy (removal of the fallopian tube containing the ectopic pregnancy) is the standard surgical procedure to control bleeding and remove the ectopic gestation.
During surgery, the contralateral (opposite) fallopian tube is examined for patency and any blockages are addressed if possible, to optimize future fertility.
If the tubal rupture is recent and the intraperitoneal blood is fresh and not contaminated, autotransfusion may be considered. The blood is collected, filtered into an anticoagulant (sodium citrate), and re-infused into the patient. If autotransfusion is not suitable or sufficient, cross-matched banked blood is transfused as needed.
Post-operative Care:
Post-operative care is vital for recovery and preventing complications.
Post-operative Bed Preparation:
Prepare a post-operative bed with all necessary accessories readily available: drip stand, oxygen delivery system, vital signs monitoring tray, emergency medication tray, resuscitation equipment, etc. This ensures immediate availability of essential equipment upon the patient’s return from theatre.
Patient Reception Post-operatively:
When surgery is complete, inform ward staff. Two qualified nurses should go to the recovery room in the operating theatre to collect the patient.
In the recovery room, receive a detailed handover report from the anesthetist and the theatre nurse about the patient’s intra-operative course and current condition.
While still in the recovery room, independently verify the report by:
Checking airway patency, breathing effectiveness, and circulatory status (ABC).
Taking immediate post-operative vital signs.
Observing the surgical site for any signs of active bleeding.
Checking the urinary catheter for proper drainage, color, and amount of urine.
After confirmation of stable initial recovery, gently transfer the patient from the operating table trolley to the prepared ward bed in a recumbent position, with the head turned to one side, ensuring continuous airway monitoring during transport.
On the Ward (Post-operative Management):
Carefully lift the patient from the trolley to the prepared post-operative bed. Position the bed close to the nurses’ station for frequent and close observation.
Place the patient in a recumbent position with the head turned to the side to facilitate drainage of oral secretions and prevent tongue fallback, which could obstruct the airway.
Observations and Records (Post-operative Monitoring):
Monitor and record vital signs (temperature, pulse, respiration rate, blood pressure) frequently: every 15 minutes for the first hour, every 30 minutes for the next hour, then hourly for the next 2 hours, and then 2-hourly, or as per surgeon’s instructions. The frequency of monitoring is gradually reduced as the patient’s condition stabilizes. Continue these observations until discharge.
Regularly observe the surgical wound site for signs of bleeding or hematoma formation.
Monitor urinary catheter drainage, noting patency, urine color, and hourly urine output.
Maintain a meticulous fluid balance chart, recording all intravenous and oral intake and all output (urine, drains, etc.). Balance the chart every 24 hours to monitor hydration status and rule out acute kidney injury.
Comfort and Hygiene:
Upon regaining consciousness, welcome the patient back from theatre. Sponge the face with a cool, damp cloth. Change the theatre gown for a clean hospital gown. Provide mouth care to freshen the mouth and remove anesthetic taste. Offer a pillow for comfort.
Fluid/Hydration Management:
Continue intravenous fluid infusion (e.g., 0.9% saline) to replace peri-operative fluid losses and maintain hydration.
Closely observe the intravenous infusion site for signs of phlebitis (swelling, redness, pain) and monitor the drip rate. Correct any issues promptly.
Carefully monitor fluid intake and output to prevent fluid overload or dehydration.
Intravenous fluids are typically discontinued when bowel sounds are audible, indicating return of bowel function, and the patient is able to tolerate oral fluids and diet.
Remove the intravenous cannula when intravenous medications are completed and oral intake is adequate.
Drug Therapy (Post-operative Medications):
Administer prescribed antibiotics to prevent post-operative infections. Common regimens may include:
Ampicillin 500mg every 6 hours for 5 days.
Ceftriaxone 2g once daily for 5 days.
Metronidazole 500mg every 8 hours for 5 days.
Gentamicin 160mg once daily for 5 days.
Administer prescribed analgesics for post-operative pain relief. Common options may include:
Pethidine 100mg every 8 hours for 3 doses.
Diclofenac 75mg every 8 hours for 12 hours.
Paracetamol (Panadol) 1g every 8 hours for up to 5 days, initiated as soon as the patient can take oral medications.
Monitor the patient for any adverse side effects of all administered medications.
Administer supportive medications such as ferrous sulfate and folic acid supplements to prevent or treat post-operative anemia.
Wound Care:
Regularly inspect the surgical wound for signs of bleeding, hematoma, or infection (redness, swelling, discharge, increased pain). Reinforce dressings if soiled, and change dressings as needed, using aseptic technique.
Perform daily wound dressing changes as per hospital protocol and physician orders.
Sutures or surgical staples are typically removed on post-operative days 7 and 8, often removing alternate sutures/staples on day 7 and the remainder on day 8.
Physiotherapy:
Encourage the patient to perform deep breathing and coughing exercises regularly to prevent post-operative chest complications such as atelectasis and hypostatic pneumonia.
Encourage early mobilization. Start with passive limb movements while in bed, progressing to active exercises and ambulation as tolerated to prevent deep vein thrombosis (DVT) and promote circulation.
Psychotherapy and Emotional Support:
In addition to pre-operative psychological support, provide continuous reassurance and emotional support post-operatively to alleviate anxiety and address emotional distress related to pregnancy loss and surgery.
Dietary Management:
Perform a ‘digestion test’ (auscultate for bowel sounds) to assess return of bowel function. Once bowel sounds are present, start the patient on clear fluids, offering small sips of water initially.
Gradually introduce a soft diet, progressing to a regular diet as tolerated.
Ensure the diet is nutritionally balanced and rich in:
Protein: To promote tissue repair and wound healing.
Fiber (roughage): To prevent constipation.
Carbohydrates: For energy.
Vitamins and minerals: For overall recovery.
Note: Remove the nasogastric tube once the patient can tolerate oral intake without nausea or vomiting.
Hygiene:
Provide a bed bath on the first post-operative day while the patient is still weak. Progress to assisting the patient to shower or bathe in the bathroom as strength improves.
Ensure regular mouth care to prevent oral complications like stomatitis and halitosis.
Maintain a clean and comfortable environment, ensuring clean patient clothing and bed linens.
Bowel and Bladder Care:
Monitor urine output. If urine is clear and adequate (typically within 24-48 hours post-operatively), remove the urinary catheter. Encourage the patient to void spontaneously.
Encourage bowel movements. Provide privacy and offer a diet rich in fiber to prevent constipation.
If constipation occurs and conservative measures (diet, fluids, mobilization) are ineffective, administer mild laxatives such as bisacodyl (5-10mg orally at night or per rectum).
Rest and Sleep:
Ensure a quiet, well-ventilated room with controlled lighting and temperature.
Restricting visitors and minimizing disturbances can create a conducive environment for rest and sleep, which are crucial for recovery.
Discharge Advice:
When the patient is deemed fit for discharge, provide clear and comprehensive discharge advice:
Advise adequate rest at home to facilitate recovery.
Instruct the patient to avoid heavy lifting or strenuous activities to prevent strain on abdominal muscles and wound healing.
Schedule follow-up review appointments at the clinic or hospital and ensure the patient understands the importance of attending these appointments.
Advise attendance at antenatal care (ANC) clinics for future pregnancies, once medically cleared.
If pelvic inflammatory disease (PID) was suspected as a contributing factor to the ectopic pregnancy, advise the patient to bring her husband or partner for evaluation and treatment, as appropriate.
Ensure the patient understands and has a supply of all prescribed discharge medications and emphasize the importance of completing the full course of treatment.
Complications of Ectopic Pregnancy:
Ectopic pregnancy and its management can lead to both immediate and long-term complications.
Immediate Complications:
Shock (Hypovolemic Shock): Due to significant internal bleeding from tubal rupture, leading to circulatory collapse.
Peritonitis: Infection of the peritoneum (lining of the abdominal cavity) can occur secondary to rupture and blood in the abdominal cavity or post-operatively.
Dehydration: Fluid loss from bleeding and potentially vomiting can lead to dehydration.
Long-Term Complications:
Sepsis: Systemic infection arising from peritonitis or surgical site infection.
Anemia: Chronic anemia may persist after significant blood loss, requiring iron supplementation and monitoring.
Fibrosis and Adhesions: Scar tissue formation (fibrosis) and adhesions (abnormal tissue connections) can develop in the pelvis following surgery, potentially affecting future fertility or causing chronic pelvic pain.
Recurrence of Ectopic Pregnancy: Women who have had an ectopic pregnancy have a higher risk of experiencing another ectopic pregnancy in subsequent pregnancies.
Infertility: In some cases, ectopic pregnancy or its surgical management (especially salpingectomy) can contribute to infertility. Psychological distress and grief related to pregnancy loss and potential fertility concerns are also significant long-term considerations.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda

