paediatrics
Subtopic:
Fractures
What a Fracture Is
This means a break or a crack in a bone. It can range from a thin crack to a complete break where the bone is in two or more pieces.
Common Causes
Trauma: Most often due to injuries such as:
Falls (e.g., from a height, during play, off a bicycle).
Direct blows or impact (e.g., during sports, being hit by an object).
Twisting injuries (e.g., to an arm or leg).
Stress Fractures: Caused by repetitive stress or overuse, often seen in athletes.
Pathological Fractures: Occur in bones weakened by an underlying disease (e.g., bone cysts, tumors, certain metabolic bone diseases), causing a break with minimal or no trauma.
General Signs and Symptoms
The signs can vary depending on the location and severity of the fracture, but common indicators include:
Pain: Often severe, especially at the site of the injury; may worsen with movement or pressure.
Swelling: Occurs around the injured area.
Bruising (Ecchymosis): Discoloration of the skin due to bleeding under the skin.
Deformity: The injured limb or area may look misshapen, bent, or out of its normal position.
Loss of Function: Difficulty or inability to move the injured limb or bear weight on it.
Tenderness: Pain upon touching the injured area.
Crepitus: A grating or crackling sound or sensation felt when the broken bone ends rub together (should not be actively sought).
In open fractures, bone may be visible through a break in the skin.
Types of Fractures
Fractures are classified in several ways:
Based on Skin Integrity:
Closed (Simple) Fracture: The bone is broken, but the skin over the fracture site is intact.
Open (Compound) Fracture: The broken bone pierces the skin, or there is a wound that extends down to the fractured bone. This type has a higher risk of infection.
Based on the Fracture Line/Pattern:
Transverse Fracture: A straight break across the bone.
Oblique Fracture: An angled break across the bone.
Spiral Fracture: A break that spirals around the bone, often caused by a twisting force.
Comminuted Fracture: The bone is broken into three or more pieces.
Segmental Fracture: A bone is broken in two places, resulting in a “floating” segment of bone.
Based on Completeness:
Complete Fracture: The bone is broken into two or more separate pieces.
Incomplete Fracture: The bone is cracked but not broken all the way through. Common types of incomplete fractures include:
Greenstick Fracture: The bone bends and cracks on one side, but not completely through (like breaking a green, young tree branch). More common in individuals with softer, more pliable bones.
Buckle (Torus) Fracture: One side of the bone buckles or bulges upon itself without breaking the other side. Also common in softer bones due to compression forces.
Other Specific Types:
Growth Plate (Physeal) Fracture: A fracture that involves the physis (growth plate), an area of growing cartilage at the ends of long bones. These are unique to growing individuals and are classified using systems like the Salter-Harris classification. They require careful management as damage can affect future bone growth.
Stress Fracture: A small crack in a bone, often caused by repetitive force or overuse.
Avulsion Fracture: A small piece of bone attached to a tendon or ligament gets pulled away from the main part of the bone.
Diagnosis
History: Understanding how the injury occurred (mechanism of injury).
Physical Examination: Assessing for signs and symptoms, checking for deformity, swelling, tenderness, range of motion, and neurovascular status (circulation, sensation, and movement distal to the injury).
Imaging Studies:
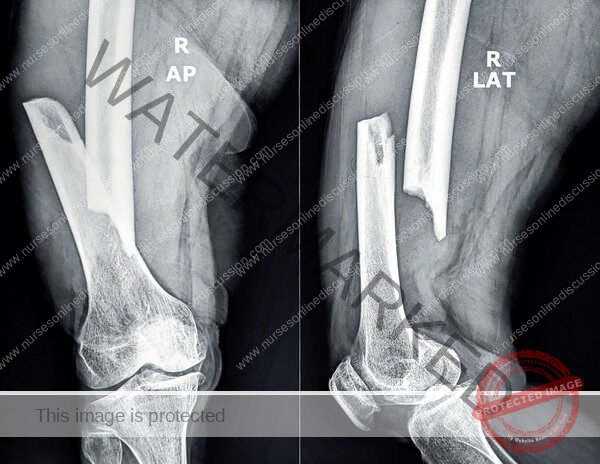
X-rays: The most common and usually the first imaging test to confirm a fracture, show its type, and location. At least two views (e.g., anteroposterior and lateral) are typically taken.
Computed Tomography (CT) Scan: May be used for more complex fractures, to get a better view of the fracture lines, or to assess joints.
Magnetic Resonance Imaging (MRI): Useful for detecting stress fractures, injuries to soft tissues (ligaments, tendons) around a fracture, or to evaluate growth plate injuries.
Principles of Management / Treatment
The goals of fracture treatment are to:
Relieve pain.
Achieve and maintain proper alignment (reduction) of the broken bone fragments.
Promote bone healing.
Restore normal function of the injured part.
Prevent complications.
First Aid / Initial Management:
Immobilize the injured limb to prevent further movement and damage.
Apply ice packs (wrapped in a cloth) to reduce swelling and pain.
Elevate the injured limb if possible.
Pain relief medication.
Reduction (Aligning the Bone):
Closed Reduction: The bone fragments are manually realigned without surgery. This is often done under sedation or anesthesia.
Open Reduction: Surgical realignment of the bone fragments. This is necessary for complex fractures, open fractures, or when closed reduction is unsuccessful.
Immobilization (Keeping the Bone Aligned While it Heals):
Casts: Made of plaster or fiberglass, encasing the injured limb to hold the bones in place.
Splints: Provide support and immobilization but are often used for initial stabilization or when some swelling is anticipated, as they are not circumferential like casts.
Traction: Uses weights, ropes, and pulleys to apply a gentle, continuous pulling force to align bone fragments and immobilize the area. Can be skin traction or skeletal traction (pins inserted into the bone).
Internal Fixation (Open Reduction Internal Fixation – ORIF): During surgery, bone fragments are held together with metal implants like pins, wires, screws, plates, or rods.
External Fixation: Metal pins or screws are inserted into the bone above and below the fracture site and are attached to a metal bar or frame outside the skin. This stabilizes the bones while they heal. Often used for severe open fractures or complex fractures.
Pain Management: Analgesics are prescribed to control pain.
Rehabilitation: Once the fracture has healed sufficiently, physical therapy is often needed to restore range of motion, strength, and function to the injured limb.
Healing Process
Bone healing is a natural process that occurs in stages:
Inflammation and Hematoma Formation: Blood clots form at the fracture site.
Soft Callus Formation: Fibrous tissue and cartilage begin to bridge the gap.
Hard Callus Formation: The soft callus is replaced by woven bone.
Bone Remodeling: The woven bone is gradually replaced by stronger, lamellar bone, and the bone reshapes to its original form.
Healing time varies depending on age, type and location of fracture, nutritional status, and overall health. Healing is generally faster in younger individuals.
Potential Complications
Early Complications:
Neurovascular Injury: Damage to nearby nerves or blood vessels from the bone fragments or swelling. Requires immediate attention.
Compartment Syndrome: A serious condition where increased pressure within a muscle compartment (due to swelling or bleeding) compromises circulation and nerve function. Symptoms include severe pain out of proportion to the injury, pain with passive stretch of muscles in the compartment, tenseness of the compartment, pallor, paresthesia (pins and needles), and eventually pulselessness. This is a surgical emergency requiring a fasciotomy (surgical incision to relieve pressure).
Infection (Osteomyelitis): Particularly a risk with open fractures or after surgical fixation.
Fat Embolism Syndrome: Rare but serious; fat globules from the bone marrow enter the bloodstream and can travel to the lungs or brain. More common with fractures of long bones (like the femur).
Late Complications:
Malunion: The fracture heals in an incorrect or deformed position.
Nonunion: The fracture fails to heal completely.
Delayed Union: The fracture takes longer than usual to heal.
Growth Disturbance: If a growth plate fracture is not managed properly or is severe, it can lead to premature closure of the growth plate, resulting in a shortened limb or angular deformity.
Joint Stiffness or Contracture: Prolonged immobilization can lead to stiffness.
Post-traumatic Arthritis: Arthritis can develop in a joint that has been fractured or injured.
Chronic Pain.
Considerations for Fractures in Growing Individuals
Bones are more porous and elastic, leading to unique fracture patterns like greenstick and buckle fractures.
The presence of physes (growth plates) makes them susceptible to physeal fractures, which require careful management to prevent growth disturbances.
Bone healing is generally faster.
The periosteum (the thick membrane covering bones) is thicker and stronger, contributing to faster healing and sometimes preventing complete displacement of fractures.
The mechanism of injury should always be consistent with the type of fracture and the individual’s developmental stage.
Related Topics
- Common health problems during childhood
- Nature and Causes of Childhood Diseases
- Respiratory System Diseases
- Gastrointestinal Tract Conditions
- Cardiovascular System Diseases and Conditions
- Central Nervous System Diseases
- Genitourinary Tract Diseases and Conditions
- Endemic and Epidemic Diseases
- Tumors in Children
- Eye and Ear Conditions
- HIV/AIDS in Children
- Integrated Management of Childhood Illnesses (IMCI)
- Surgical Conditions in Children
- Congenital Malformations in Children
- Fractures
- Burns
- Surgical Conditions of the Gastrointestinal Tract
- Provide first aid management of various accidents in children
- Admit children involved in accidents
- Educating Mothers on Accident Prevention in Children
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

