Eye Conditions
Subtopic:
Trachoma
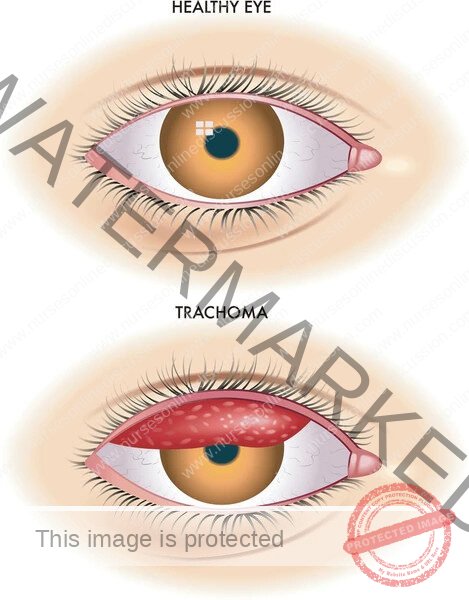
Trachoma
This refers to a chronic infectious disease of the eye and is the leading infectious cause of preventable blindness worldwide. It is a keratoconjunctivitis, meaning it affects both the conjunctiva (the mucous membrane lining the eyelids and covering the white part of the eye) and the cornea (the clear front surface of the eye).
Causative Agent:
Chlamydia trachomatis (serovars A, B, Ba, and C). These are obligate intracellular bacteria.
Epidemiology and Risk Factors:
Predominantly found in poor, rural communities in developing countries with inadequate access to water and sanitation.
Endemic in many parts of Africa, Asia, Central and South America, Australia, and the Middle East.
Children, especially preschoolers (ages 1-9), are the main reservoir of infection due to higher rates of active disease and nasal/ocular discharge.
Women are affected more frequently than men, likely due to closer contact with infected children.
Risk factors (the “5 Fs” are often cited, though simplification is common):
Faces (unclean faces)
Fingers (unclean hands)
Flies (eye-seeking flies like Musca sorbens that breed in human feces)
Fomites (contaminated towels, bedding, clothing)
Feces (poor sanitation leading to fly breeding)
Crowded living conditions.
Limited access to clean water for hygiene.
Poor sanitation and waste disposal.
Transmission:
Direct contact with ocular or nasal discharge from an infected individual.
Indirect contact through contaminated hands, clothing, towels, or other fomites.
Eye-seeking flies that have been in contact with discharge from infected eyes.
Repeated episodes of infection over many years lead to the blinding complications.
Pathophysiology and Clinical Stages (WHO Grading System):
The disease progresses through stages of inflammation and scarring. Repeated infections are key to developing severe, sight-threatening disease. The WHO has a simplified grading system for trachoma:
Trachomatous Inflammation – Follicular (TF):
This is the earliest sign of active trachoma.
Characterized by the presence of five or more follicles in the upper tarsal conjunctiva (the conjunctiva lining the inner surface of the upper eyelid).
Follicles are small, round, yellowish-white swellings (lymphoid germinal centers) that are at least 0.5 mm in diameter. They are most easily seen on the everted upper eyelid.
(Image description: Close-up of an everted upper eyelid showing multiple small, pale, raised bumps – the follicles – on the pink conjunctival surface.)
Trachomatous Inflammation – Intense (TI):
This represents a more severe active inflammatory response.
The upper tarsal conjunctiva is markedly thickened, red, and swollen, obscuring more than half of the normal deep tarsal blood vessels.
Follicles are often present, but the intense inflammation is the dominant feature.
(Image description: Close-up of an everted upper eyelid showing a diffusely red, thickened, and somewhat velvety conjunctival surface, where the underlying blood vessels are difficult to see clearly due to the swelling.)
Trachomatous Scarring (TS):
Evidence of past or chronic inflammation, leading to scar tissue formation on the tarsal conjunctiva.
Appears as white lines, bands, or sheets of fibrous tissue. Severe scarring can distort the eyelid.
Arlt’s line is a specific type of scar – a horizontal line of scarring across the upper tarsal conjunctiva.
(Image description: Close-up of an everted upper eyelid showing distinct white, linear, or sheet-like scars on the conjunctival surface. Arlt’s line, if present, would be a prominent horizontal scar.)
Trachomatous Trichiasis (TT):
This is a potentially blinding complication resulting from conjunctival scarring.
The scarred eyelid (usually the upper lid) turns inward (entropion), causing at least one eyelash to rub against the eyeball (cornea).
Evidence of recent eyelash removal also qualifies as TT.
This constant abrasion of the cornea is painful and leads to corneal damage.
(Image description: Profile or frontal view of an eye showing the upper eyelid margin turned inwards, with eyelashes visibly touching and rubbing against the cornea.)
Corneal Opacity (CO):
The cornea becomes cloudy or opaque due to chronic inflammation and abrasion from trichiasis.
This opacity, if it covers the pupil, causes irreversible vision loss and blindness.
(Image description: Frontal view of an eye where the normally clear cornea has a whitish, cloudy, or opaque area, potentially obscuring the pupil and iris.)
Symptoms:
Active Trachoma (TF and TI):
Often asymptomatic in children, or mild symptoms.
Eye irritation, redness.
Photophobia (sensitivity to light).
Mucoid or mucopurulent discharge.
Eyelid swelling.
Cicatricial Disease (TS, TT, CO):
Foreign body sensation (due to trichiasis).
Eye pain.
Excessive tearing (epiphora).
Decreased vision.
Blindness (in advanced CO).
Diagnosis:
Primarily clinical, based on identifying the characteristic signs of the WHO grading system using a binocular loupe (2.5x magnification) and adequate lighting.
Laboratory tests (e.g., nucleic acid amplification tests – NAATs like PCR for C. trachomatis DNA from conjunctival swabs) are used mainly for research or epidemiological surveys, not typically for routine clinical diagnosis in endemic areas.
Management and Treatment (WHO SAFE Strategy):
The WHO endorses the SAFE strategy to control and eliminate trachoma as a public health problem:
S – Surgery:
For trachomatous trichiasis (TT) to correct the inwardly turned eyelid and prevent eyelashes from rubbing on the cornea. Procedures like bilamellar tarsal rotation are commonly used.
A – Antibiotics:
To treat active infection (TF and/or TI) and reduce the community reservoir of C. trachomatis.
Oral azithromycin (single dose) is the preferred antibiotic for mass drug administration (MDA) and individual treatment.
Topical tetracycline eye ointment (twice daily for 6 weeks) is an alternative, especially for young children or pregnant women where azithromycin might be contraindicated or less feasible.
F – Facial Cleanliness:
Promoting regular face washing, especially in children, to remove infectious ocular and nasal secretions.
E – Environmental Improvement:
Increasing access to clean water for personal hygiene.
Improving sanitation (e.g., latrine construction and use) to reduce fly populations and fecal contamination.
Controlling fly populations.
Complications and Prognosis:
Untreated or recurrent trachoma leads to chronic inflammation, conjunctival scarring, entropion, trichiasis, and ultimately corneal opacification and blindness.
Dry eye syndrome can also result from damage to goblet cells and accessory lacrimal glands.
Secondary bacterial infections can exacerbate corneal damage.
With timely implementation of the full SAFE strategy, the prognosis for preventing blindness is good. Once significant corneal opacity has developed, vision loss is usually permanent unless corneal transplantation is available and successful (which is rare in trachoma-endemic settings).
Prevention:
Largely encapsulated within the “F” and “E” components of the SAFE strategy:
Promoting personal hygiene, particularly regular face washing with soap and water.
Improving access to clean water sources.
Improving sanitation to reduce fly breeding sites and fecal contamination.
Health education to raise awareness about trachoma transmission and prevention.
Related Topics
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

