Specialized Nursing Care Procedure
Subtopic:
Colostomy Care
Learning Objectives
Understand the anatomical differences between colostomy and ileostomy, including indications and stool characteristics.
Describe the goals of colostomy care, with emphasis on maintaining skin integrity and effective waste elimination.
Identify types of colostomies based on location, duration, and surgical technique.
Outline procedural steps for performing colostomy care in both adults and children.
Recognize common nursing diagnoses associated with colostomy patients and provide supportive care.
Apply appropriate dietary, psychosocial, and hygiene considerations in patient education and long-term management.
A colostomy
A colostomy is a surgically created opening (stoma) in the abdominal wall that connects to the colon, allowing for the elimination of waste. It involves diverting a portion of the colon from its usual path towards the anus to a new opening on the abdomen called a stoma.
An ileostomy is a similar procedure, but it involves bringing a part of the small intestine (ileum) to the abdominal surface, creating a stoma for waste elimination, bypassing the colon completely
Comparison of Ileostomy and Colostomy
Feature | Ileostomy | Colostomy |
|---|---|---|
| Intestinal Segment | Ileum (small intestine) | Colon (large intestine) |
| Stool Consistency | Liquid or semi-liquid | Can range from liquid to formed |
| Frequency | Frequent (multiple times a day) | Less frequent than ileostomy |
| Odor | Stronger odor | Generally less strong than ileostomy |
| Control | Limited control over bowel movements | More potential for control over bowel movements |
| Reasons | Ulcerative colitis, Crohn’s disease, colon cancer, etc. | Similar reasons to ileostomy, but also for conditions specific to the colon |
Purpose of Colostomy Care
The primary purpose of colostomy care is to facilitate the controlled elimination of colon contents to the outside of the body through the surgically created stoma.
Specific Goals of Colostomy Care:
Stoma and Skin Health: Maintaining the integrity of the stoma and surrounding skin, preventing irritation, trauma, and infection.
Prevent Skin Damage: Avoiding skin problems such as lesions, ulcerations, and excoriation from contact with fecal matter.
Infection Control: Preventing bacterial and fungal infections associated with fecal contamination.
Patient Comfort: Minimizing discomfort, irritation, and odor.
Positive Self-Image: Supporting the patient’s self-esteem and body image.
Effective Waste Elimination: Ensuring proper collection and containment of fecal matter using appropriate pouching systems.
Odor Management: Employing strategies to reduce unpleasant odors, including regular pouch changes and odor neutralizers.
Indications for a Colostomy
A colostomy may be indicated in the following situations:
Colon Tumors: Both cancerous and non-cancerous growths in the colon that require surgical removal.
Colon Trauma and Perforation: Injuries to the colon that necessitate diverting the fecal stream to allow healing.
Inflammatory Bowel Diseases: Conditions such as ulcerative colitis, Crohn’s disease, and diverticulitis, where a colostomy may be needed to manage inflammation or complications.
Congenital Anomalies of the Gastrointestinal Tract (GIT):
Hirschsprung’s Disease: A condition characterized by the absence of nerve cells in a portion of the colon, leading to bowel obstruction.
Necrotizing Enterocolitis: A serious intestinal condition primarily affecting premature infants.
Imperforate Anus: A birth defect where the anus is absent or blocked.
Other Congenital Colon Malformations: Various other birth defects affecting the colon.
Type of Colostomy

Colostomies can be classified based on their location, duration, and the surgical technique used.
By Location (Based on the portion of the colon used):
Ascending Colostomy: Created in the ascending colon (right side of the abdomen).
Stool Characteristics: Liquid to semi-liquid, frequent, and contains digestive enzymes that can irritate the skin.
Transverse Colostomy: Created in the transverse colon (across the upper abdomen).
Stool Characteristics: Semi-formed to soft stool, less frequent than ascending colostomy.
Descending Colostomy: Created in the descending colon (left side of the abdomen).
Stool Characteristics: Firmer, more formed stool.
Sigmoid Colostomy: Created in the sigmoid colon (lower-left abdomen).
Stool Characteristics: Formed stool, similar to normal bowel movements; may be possible to regulate bowel movements with this type.
By Duration:
Permanent Colostomy: Intended as a long-term or lifelong solution. Typically performed when a portion of the colon is removed or severely damaged.
Temporary Colostomy: Created to allow a part of the colon to heal or to divert stool while other surgical procedures are performed. It is designed to be reversed later.
By Surgical Technique:
Loop Colostomy: A loop of the colon is brought to the abdominal surface. The loop is partially divided, creating two openings: one for stool and one for mucus. Often preferred for temporary colostomies due to easier reversal.
End Colostomy: The end of the functioning part of the colon is brought to the abdominal surface, creating a single opening for stool. Often used for permanent colostomies. The end of the remaining inactive bowel is sealed after the bowel is cut.
Double-Barrel Colostomy: Both ends of the divided colon are brought to the surface, creating two separate stomas. One expels stool and the other expels mucus.
Characteristics of Feces According to Colostomy Location:
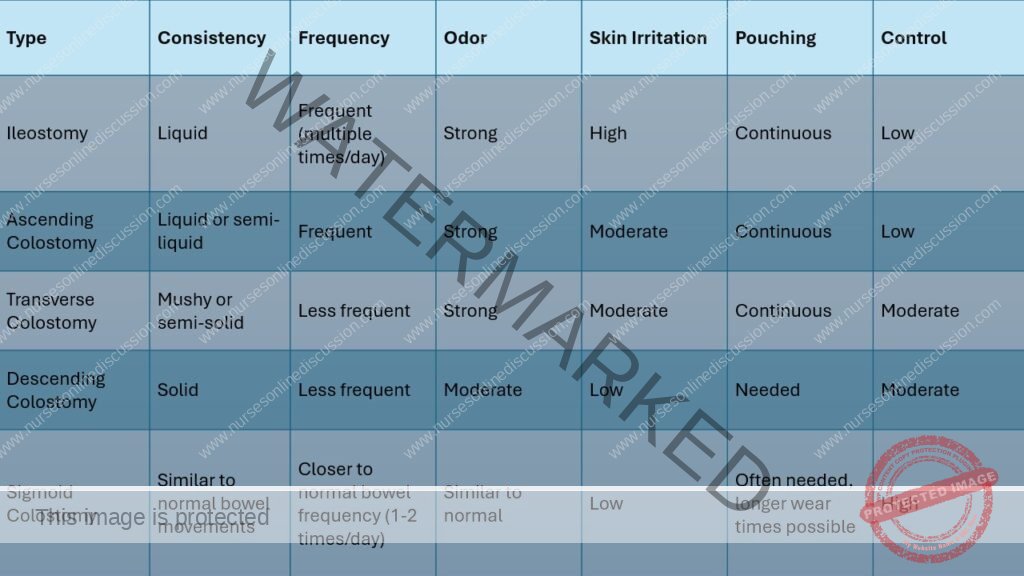
Note: Control: Refers to the ability to control bowel movements. Pouching: Continuous pouching means the pouch needs to be worn all the time.

Procedure Steps for Colostomy Care
Requirements
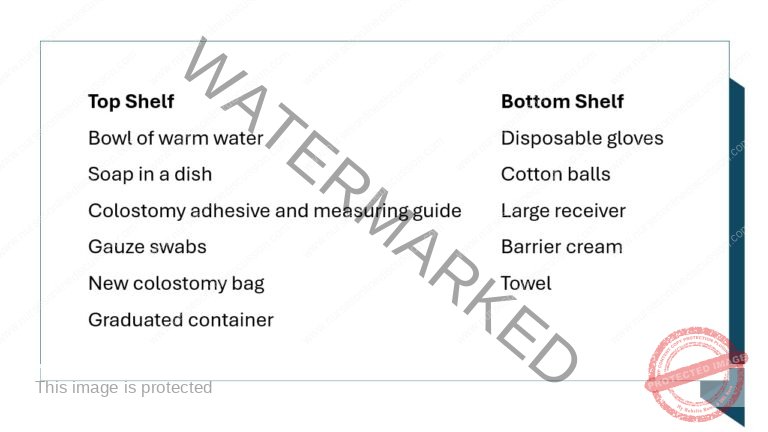
Procedure
Step | Action | Rationale |
1 | Follow the general rules. | Ensures adherence to standard protocols and enhances procedural consistency. |
2 | Turn down the bed clothes. | To expose the stoma and avoid soiling bed clothes. |
3 | Remove the soiled bag gently, taking care not to pull the skin. | Protects the underlying skin from damage. |
4 | Wash the area around the stoma with soapy water and dry well. Apply a little barrier cream if necessary. | Removes excretions and old adhesive, promoting skin integrity. |
5 | Re-measure the stoma and make the correct measurement. | Ensures that the bag fits correctly, preventing leakage and skin irritation. |
6 | Cut the correct size of circle in the stoma adhesive, using the measuring guide, and apply it on the stoma. | Prevents trauma to the stoma if the opening is too small and skin irritation if too large. |
7 | Apply a clean bag on the stoma. | Prevents infection by providing a sterile environment. |
8 | Remove the soiled articles, assess patient’s response to the procedure, and leave the patient comfortable. | Promotes patient understanding about the colostomy and ensures comfort. |
9 | Wash and dry hands. | Reduces the risk of cross-infection. |
Procedure for Colostomy Care in Children
Gather Supplies: Assemble all necessary equipment for the procedure.
Explain and Involve: Explain the procedure to the child in an age-appropriate manner, encouraging their participation to reduce anxiety.
Hand Hygiene: Wash hands thoroughly with soap and water to prevent contamination and reduce the risk of infection.
Gloving: Put on clean gloves to maintain hygiene and prevent infection transmission.
Protective Barrier: Place a waterproof barrier (e.g., towel or disposable pad) under the child to protect the skin and bedding from fecal matter.
Auscultate Bowel Sounds: Listen for bowel sounds to assess intestinal activity.
Linen Saver Placement: Position a linen saver on the abdomen around and below the stoma opening.
Pouch Removal: Carefully remove the existing pouch and skin barrier (wafer) and place them in a disposable waste bag.
Wafer Removal: Gently lift a corner of the wafer with one hand while pressing down on the skin with the other hand. Remove the wafer in small sections.
Gauze Placement: Place a gauze pad over the stoma opening.
Save Tail Closure: If reusable, save the tail closure from the pouch.
Stoma and Skin Assessment: Inspect the stoma and surrounding skin. Note the color, swelling, any signs of trauma or healing, and the condition of the existing skin barrier. The stoma should appear moist and reddish-pink.
Pouch Emptying: Empty the pouch contents into a measuring container, record the amount and characteristics of the fecal output, and discard appropriately.
Hand Hygiene and New Gloves: Remove and discard the used gloves. Wash hands thoroughly and put on a new pair of clean gloves.
Gentle Pouch and Barrier Removal: Gently remove any remaining adhesive or skin barrier, carefully pushing the skin away from the barrier to minimize skin trauma.
Peristomal Skin Cleaning: Clean the skin around the stoma gently with warm water and gauze pads. Avoid harsh rubbing.
Stoma Measurement: Measure the stoma using the manufacturer’s measuring guide to determine the correct size for the new pouching system.
Pouch Preparation: Select the appropriate pouch based on the child’s needs. If using a custom cut-to-fit pouch, use an ostomy guide to cut the opening to the correct size. Prepare the pouch by removing the backing from the barrier and adhesive, leaving the adhesive covering of the skin barrier wafer intact.
Stoma Paste Application: Remove the gauze and apply stoma paste around the stoma or to the edges of the opening in the wafer, if needed, to create a seal.
Wafer Application: Remove the adhesive covering from the wafer. Center the wafer over the stoma and press it firmly in place for about 30 seconds to ensure a good seal.
Pouch Attachment: Center the new pouch over the stoma and attach it to the wafer.
Positive Reinforcement: Praise the child for their cooperation during the procedure.
Equipment Disposal/Storage: Dispose of or store all equipment appropriately.
Hand Hygiene: Remove and discard gloves. Wash hands thoroughly.
Odor Control: Use a room deodorizer if needed to eliminate any unpleasant odors.
Documentation: Record the type of pouch and skin barrier used, the amount and appearance of the fecal output, and the condition of the stoma and surrounding skin.
Nursing Diagnoses Related to Colostomy Care
Several nursing diagnoses may be relevant for patients with a colostomy, including:
Impaired Comfort: Related to the surgical incision, as evidenced by:
Verbal reports of pain at the incision site.
Facial grimacing or guarding behaviors.
Elevated pain scores.
Difficulty moving or walking.
Restlessness or anxiety due to pain.
Risk for Impaired Skin Integrity: Related to the presence of the stoma and contact with effluent, as evidenced by:
Redness, swelling, or irritation around the stoma.
Skin breakdown, such as abrasions or ulcers.
Complaints of discomfort or itching.
Leakage or drainage from the stoma.
Disturbed Body Image: Related to the altered body appearance and function, as evidenced by:
Expressing negative feelings or self-consciousness about the stoma.
Avoiding social situations.
Difficulty looking at or touching the stoma.
Statements indicating feelings of being unattractive or different.
Deficient Knowledge: Related to stoma care and lack of prior experience, as evidenced by:
Frequent questions about stoma care.
Incorrect demonstration of care techniques.
Expressing anxiety or fear about managing the stoma.
Lack of confidence in self-care.
Nursing Considerations in Colostomy Care
Stoma Assessment:
Color: The stoma should be a healthy pink or red color. A dusky blue color suggests ischemia (inadequate blood supply), while a brown-black color indicates necrosis (tissue death). Assess stoma color at least every 8 hours.
Edema: Mild to moderate swelling is expected in the first 2-3 weeks post-surgery. Severe swelling could indicate an obstruction, allergic reaction, or gastroenteritis.
Bleeding: A small amount of oozing when the stoma is touched is normal due to its high vascularity. Moderate to large amounts of bleeding could indicate a bleeding disorder, gastrointestinal bleeding, or other issues.
Skin Protection:
Hygiene: Cleanse the peristomal skin with mild soap and warm water, then dry it thoroughly before applying a new skin barrier.
Skin Barriers: Use skin barriers such as petroleum jelly gauze or protective ointments around the stoma to prevent irritation. Ensure the skin under the barrier is regularly assessed for integrity.
Pouch Management:
Changing Supplies: Provide the patient with necessary supplies for changing the pouch.
Waterproofing: Pouching systems are waterproof, allowing patients to bathe or swim with them in place. However, patients with colostomies can shower without a pouch, but those with ileostomies should avoid doing so because of their frequent, unpredictable output.
Selection: Choose a transparent, odor-proof plastic pouch with an appropriate-sized opening that fits snugly around the stoma without touching it. Ensure the pouch has a drainage valve or can be easily changed.
Emptying and Changing: Empty the pouch when it is 1/3 full to prevent leakage. Record the volume, color, and consistency of the drainage each time the pouch is changed. Observe the skin for irritation.
Dietary Considerations:
Initial Diet: For the first month, a low-fiber diet is recommended.
Long-Term Diet: After one month, a regular diet is usually tolerated.
Ileostomy Diet: Patients with ileostomies need to be cautious of foods that can cause blockage (e.g., popcorn, nuts, certain vegetables, tough meats).
Hydration: Encourage fluid intake of at least 3 liters per day (unless contraindicated) to prevent dehydration, especially in hot weather or with diarrhea.
Activity:
Heavy Lifting: Avoid heavy lifting for 6-8 weeks after surgery to prevent hernias.
Clothing: Loose-fitting clothing is often preferred initially. Avoid tight belts over the stoma.
Patient and Family Education:
Pouch Management: Teach the patient how to apply, change, and empty the pouch.
Skin and Stoma Care: Educate on proper skin care, odor control, and stoma assessment.
Dietary Guidance: Provide information on appropriate foods and the importance of hydration.
Obtaining Supplies: Provide information on where to obtain ostomy supplies.
Follow-Up Care: Emphasize the importance of regular follow-up appointments and when to report complications (e.g., changes in stoma appearance or function, fever, diarrhea, skin irritation).
Colostomy Irrigation:
May be used to regulate bowel movements or treat constipation. It involves instilling lukewarm water (500-1000 ml) into the stoma using a soft catheter. Do not force the catheter if resistance is felt.
Managing Odor and Gas:
Dietary Modifications: Identify and limit foods that cause excessive odor (e.g., eggs, onions, fish, cabbage, alcohol) or gas (e.g., beans, onions, cabbage, beer, carbonated beverages).
Diarrhea: Avoid foods that may worsen diarrhea (e.g., alcohol, spinach, green beans, coffee, spicy foods, raw fruits).
Psychosocial Adaptation:
Emotional Support: Provide emotional support and encourage the patient to express their feelings about the colostomy.
Gradual Acceptance: Encourage the patient to gradually participate in their stoma care, but do not force them before they are ready.
Cleanliness and Odor Control: Maintain a clean and odor-free environment to minimize the patient’s distress.
Social and Sexual Concerns: Address concerns about social interactions, clothing, sexual activity, sleep, and body image. Encourage open communication with partners and provide resources for support.
Pregnancy: Reassure patients that pregnancy is possible with a colostomy, but the number of pregnancies may need to be limited.
Nursing Care Guidelines
Gentle and Professional Approach: Treat the patient with empathy and maintain a professional demeanor.
Regular Stoma Assessment: Monitor the stoma for any changes in color, size, or appearance.
Maintain Cleanliness: Change soiled appliances, dressings, or linens promptly.
Monitor for Undissolved Medications: Check for undissolved medications in the ileostomy pouch, as this may indicate absorption problems.
Skin Protection: Apply skin barriers and provide appropriate skin care around the stoma.
Careful Cleaning: Cleanse the healed stoma with mild soap and water. Avoid alcohol, and discontinue soap if irritation occurs. Consult a healthcare provider if redness or yeast-like growth appears.
Patient Education: Teach the patient how to manage their ostomy independently, including appliance changes and what to monitor and report.
Emotional Support: Allow the patient to express their feelings, answer questions, and address misconceptions.
Abnormal and Danger Signs in a Stoma
Unusual Noises: Report any abnormal sounds emanating from the stoma.
Excessive Bleeding: Report any significant bleeding from the stoma.
Color Changes: Report darkening (indicating stenosis or compromised blood supply) or bleaching/extreme lightening (indicating poor circulation).
Stoma Drying: The stoma should remain moist; report any signs of drying.
Signs of Infection: Report any redness, swelling, or discharge around the stoma.
Stoma Edema: Report any swelling, which could indicate an obstruction or other complication.
Routine Observations
Appliance Fit: Ensure the appliance fits correctly to prevent leakage and maintain circulation.
Daily Weight: Monitor the patient’s weight for fluctuations that may indicate fluid or nutritional imbalances.
Electrolyte Balance: Regularly review blood test results to monitor electrolyte levels.
Stool Assessment: Record the amount and characteristics of stool to identify any changes or problems.
Vital Signs: Monitor vital signs regularly to detect early signs of complications
Complications of Colostomy
Complications associated with a colostomy can be broadly categorized as follows:
1. Surgical Complications:
Wound Infection: Bacterial contamination of the surgical wound, potentially causing pain, inflammation, and delayed healing.
Hemorrhage: Bleeding from the surgical site, requiring medical intervention.
Parastomal Hernia: Protrusion of abdominal contents through a weakness in the abdominal wall near the stoma.
2. Stoma-Related Complications:
Stenosis: Narrowing of the stoma opening, potentially obstructing stool passage.
Prolapse: Protrusion of the stoma beyond the desired level, which can cause discomfort and pouching difficulties.
Retraction: Sinking or receding of the stoma below the skin surface, making pouch application challenging.
Necrosis: Tissue death of the stoma, often due to inadequate blood supply, requiring urgent surgical intervention.
3. Skin Issues:
Irritation and Breakdown: Skin irritation, inflammation, and potential ulceration around the stoma (peristomal skin) due to prolonged contact with fecal matter.
Infection: Bacterial or fungal infections of the peristomal skin.
4. Other Complications
Bleeding: While some minor bleeding from the stoma is normal, excessive bleeding may indicate a problem like trauma or infection.
Obstruction: Blockage of the colostomy, hindering the passage of stool.
5. Fluid and Electrolyte Imbalance:
Dehydration: Increased risk of fluid loss through the stoma, particularly with high-output stomas.
Electrolyte Imbalance: Potential loss of electrolytes, especially with significant fluid loss.
6. Psychosocial and Nutritional Issues:
Psychosocial Impact: Potential for body image issues, anxiety, and depression related to living with a stoma.
Nutritional Deficiencies: Possible impaired nutrient absorption, leading to deficiencies.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowRelated Topics
Foundations of Nursing (III)
- Apply Nursing process to the management of patients
- Administer prescribed medicine appropriately
- Instilling medication (general)
- Blood transfusion
Specialized Nursing Care Procedures
- Perform Shortening and removal of drains
- Perform Colostomy Care
- Prepare Abdominis Paracentesis (Abdominal Tapping)
- Prepare Lumbar Puncture
- Perform Gastrostomy Feeding
- Carry out gastric Lavage
- Perform Tracheostomy Care
- Ophthalmological Care
- Care of the patient`s ears
- Pre-Operative Eye Care
- Ear Care
- Peri-Operative Care:
- Orthopedic Nursing Care
- Prepare for Neurological Assessment
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2026 Nurses online discussion. All Rights Reserved

