Conditions of the eye
Subtopic:
Conjunctivitis
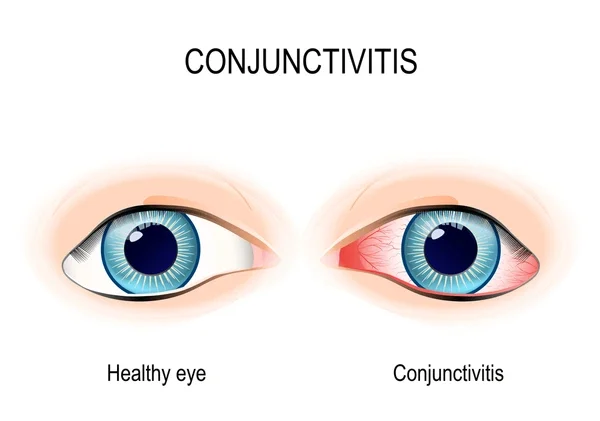
Conjunctivitis refers to the inflammation of the conjunctiva, which is the thin, clear membrane that lines the inner surface of the eyelids and the white part of the eyeball. This inflammation can arise from various causes, including infections (bacterial, viral, or fungal), allergic reactions, chemical irritants, or even parasites.
A hallmark of conjunctivitis is the dilation, or widening, of the blood vessels within the conjunctiva. This dilation leads to the characteristic redness (hyperemia) and swelling (edema) of the conjunctiva. Often, this is accompanied by discharge from the eye.
Conjunctivitis is a very common reason for experiencing a “red eye.” While it can be bothersome, it is frequently painless and is typically identified by the presence of a discharge that can be either thick and pus-like or thin and watery.
Types of Conjunctivitis
Bacterial Conjunctivitis: This type of conjunctivitis is caused by bacteria, such as Staphylococcus or Streptococcus species.
Acute Viral Conjunctivitis: Viruses are another common cause, with the herpes simplex virus being one example.
Allergic Conjunctivitis: This occurs when the eye is exposed to allergens like smoke, certain cosmetic ingredients, or medications.
Bacterial Conjunctivitis in Detail
Several factors can make someone more susceptible to bacterial conjunctivitis:
Flies: These insects can carry and transmit bacteria to the eyes.
Poor Hygienic Conditions: Lack of proper hygiene increases the risk of bacterial spread.
Hot, Dry Climates: These conditions can potentially irritate the eyes, making them more vulnerable to infection.
Poor Sanitation: Inadequate sanitation can contribute to the spread of bacteria.
Dirty Habits: Habits like touching the eyes with unwashed hands increase the risk of infection.
Common Bacterial Causes:
Staphylococcus aureus is frequently identified as the culprit in bacterial conjunctivitis.
Pneumococcus bacteria can also lead to this condition.
Streptococcus pyogenes (also known as beta-hemolytic streptococcus) is a more aggressive bacterium that can sometimes cause a more severe form of conjunctivitis with the formation of pseudomembranes.
Pseudomonas aeruginosa is a particularly concerning organism as it can readily invade the cornea, potentially leading to more serious complications.
Neisseria gonorrhoeae is known to cause a severe, pus-producing conjunctivitis in adults and a condition called ophthalmia neonatorum in newborns.
Neisseria meningitidis can result in a conjunctivitis with a discharge that is a mix of mucus and pus.
Corynebacterium diphtheriae can cause an acute form of conjunctivitis characterized by the formation of membranes.
How Bacterial Conjunctivitis Spreads (Mode of Infection):
The bacteria causing conjunctivitis can reach the eye from several sources:
External Sources (Exogenous Infections):
Direct Contact: Close personal contact with an infected individual can spread the bacteria.
Vector Transmission: Flies can act as carriers, transferring bacteria from one person to another.
Material Transfer: Contaminated objects, such as the infected fingers of healthcare workers, shared towels, handkerchiefs, or even medical instruments like tonometers, can spread the infection.
Spread from Nearby Infections (Local Spread): Infections in adjacent structures, like an infected tear sac, eyelids, or the nasopharynx (the upper part of the throat behind the nose), can spread to the conjunctiva.
Internal Spread (Endogenous Infections): In rare instances, bacteria can reach the conjunctiva through the bloodstream. This is less common but can occur in infections like gonococcal and meningococcal infections.
What Happens in the Eye (Pathology):
When bacteria infect the conjunctiva, a series of changes occur:
Vascular Response: The blood vessels in the conjunctiva become congested and more permeable, leading to increased blood flow and the formation of new, tiny blood vessels.
Cellular Response: Immune cells, primarily polymorphonuclear leukocytes (a type of white blood cell), move into the conjunctival tissue and the conjunctival sac to fight the infection.
Conjunctival Tissue Response: The conjunctiva becomes swollen (edematous). The surface epithelial cells can become damaged, loosen, and shed. There is also an increase in the production of new epithelial cells in the deeper layers and an increase in goblet cells, which produce mucus.
Conjunctival Discharge: The discharge seen in bacterial conjunctivitis is a mixture of tears, mucus, inflammatory cells, shed epithelial cells, fibrin (a protein involved in clotting), and the bacteria themselves. In severe cases, red blood cells may leak from the blood vessels, making the discharge appear blood-tinged.
Acute Bacterial Conjunctivitis: A Closer Look
Acute bacterial conjunctivitis is marked by significant redness of the conjunctiva and a discharge that is a mix of mucus and pus (mucopurulent). This is the most frequent type of bacterial conjunctivitis. The bacteria most commonly responsible are Staphylococcus aureus, Pneumococcus, and Streptococcus species.
How Long is it Contagious? (Infectious Period)
An individual with bacterial conjunctivitis remains contagious as long as there is discharge coming from their eye.
Recognizing the Signs (Clinical Presentation):
The conjunctiva will appear infected, often more noticeably in the fornices (the pockets where the eyelids meet the eyeball), as this area has a rich blood supply.
A key symptom is discharge, which is often most noticeable in the mornings. Upon waking, the eyelids may be stuck together due to the dried discharge.
The eyelids themselves might appear red and inflamed.
The condition can affect one eye (unilateral) or both eyes (bilateral).
Importantly, vision is typically not affected, and there is usually no significant pain.
Patients might describe a sensation of grittiness or like there is a foreign object in their eye. There may be some discomfort and, occasionally, mild sensitivity to light (photophobia).
Vision might be slightly blurry due to mucus floating in front of the cornea.
A crucial sign to look for is the presence of flakes of mucopurulent discharge in the fornices, the corners of the eyes (canthi), and along the edges of the eyelids.
How it Progresses and How it’s Diagnosed (Clinical Course and Diagnosis):
Mucopurulent conjunctivitis often starts in one eye and then affects the other within a day or two. The symptoms usually reach their peak within three to four days. Even without treatment, mild cases may resolve on their own as the body’s immune system fights off the infection, typically within 10 to 15 days.
Diagnosis is usually made based on the clinical appearance of the eye. Sometimes, a microscopic examination or culture of the eye discharge is performed to identify the specific bacteria causing the infection. It can be difficult to distinguish between bacterial and viral conjunctivitis based on symptoms alone, often requiring laboratory tests for definitive identification.
Treating Bacterial Conjunctivitis (Management):
The primary approach to managing bacterial conjunctivitis involves cleaning the eyes to remove discharge and applying antibiotic medications directly to the eye (topical antibiotics).
While bacterial conjunctivitis can sometimes resolve on its own, topical antibiotics are often recommended, especially if there is no improvement after about 3 days.
To help with light sensitivity, dark goggles can be worn. However, it is generally recommended to avoid patching the eye in cases of mucopurulent conjunctivitis. Exposure to air helps keep the temperature of the conjunctival sac lower, which can inhibit bacterial growth.
Steroid eye drops should not be used, as they can worsen the infection and potentially lead to a bacterial corneal ulcer.
Topical Antibiotics Commonly Used:
Treatment often starts with eye drops containing chloramphenicol (1%), gentamicin (0.3%), tobramycin (0.3%), or framycetin (0.3%). These are typically used 3–4 times a day. An antibiotic ointment can be used at night, which provides extended antibiotic coverage and can help reduce the morning stickiness of the eyelids.
In more severe cases, quinolone antibiotic eye drops, such as ciprofloxacin (0.3%), ofloxacin (0.3%), gatifloxacin (0.3%), or moxifloxacin (0.5%), might be considered as alternatives.
Chronic Bacterial Conjunctivitis:
Chronic bacterial conjunctivitis, also known as chronic catarrhal conjunctivitis or simple chronic conjunctivitis, is a long-lasting inflammation of the conjunctiva that is generally milder than the acute form.
Viral Conjunctivitis in Detail
Viral conjunctivitis can be caused by several types of viruses, including:
Adenovirus (a very common cause)
Herpes simplex virus
Poxvirus
Mycovirus and Paramyxovirus
Signs of Viral Conjunctivitis:
The eye will appear red or pink.
Chemosis, which is swelling of the conjunctiva, may be present, especially in severe cases.
Small bumps called follicles may be visible on the palpebral conjunctiva (the lining of the eyelids).
In severe cases of adenoviral conjunctivitis, there may be bleeding from the conjunctival blood vessels.
Managing Viral Conjunctivitis (Treatment):
The main focus of treating viral conjunctivitis is on relieving symptoms, as the infection typically needs to run its course. Supportive care includes:
Applying cold compresses to the eyes can help reduce swelling and discomfort.
If there is sensitivity to light (photophobia), wearing dark glasses can provide relief.
Artificial tear eye drops can help keep the eyes lubricated and comfortable.
Topical antibiotics are often prescribed to prevent a secondary bacterial infection from developing.
Topical antiviral medications are generally not effective for adenoviral conjunctivitis.
Topical steroid eye drops are usually avoided during the active phase of the infection, as they can allow the virus to multiply more readily and prolong the period of contagiousness. However, weak steroids like fluorometholone or loteprednol (0.5%) may be used in specific situations, such as when subepithelial infiltrates (collections of inflammatory cells) develop or when membranes form on the conjunctiva.
Providing a clear explanation of the condition to the patient can help them understand what is happening and reduce anxiety.
Preventing the Spread of Viral Conjunctivitis:
Preventive measures are crucial to control the spread of viral conjunctivitis and include:
Frequent hand washing with soap and water is essential.
Individuals with viral conjunctivitis should try to limit close contact with others to avoid spreading the infection.
Avoid rubbing the eyes.
Do not share towels or handkerchiefs.
Proper disinfection of ophthalmic instruments and clinical surfaces after examining a patient is vital to prevent transmission in healthcare settings.
Allergic Conjunctivitis
Allergic conjunctivitis is an inflammation of the conjunctiva that occurs due to an allergic reaction, a type of hypersensitivity response. These reactions can be immediate (involving antibodies) or delayed (involving immune cells).
Types of Allergic Conjunctivitis:
Simple Allergic Conjunctivitis:
Seasonal allergic conjunctivitis (SAC)
Perennial allergic conjunctivitis (PAC)
Vernal Keratoconjunctivitis (VKC)
Atopic Keratoconjunctivitis (AKC)
Simple Allergic Conjunctivitis Explained:
Simple allergic conjunctivitis is a milder form of allergic reaction in the eye, characterized by itching, redness, and a mild papillary response (small bumps on the inner surface of the eyelid).
What Causes It? (Etiology):
Simple allergic conjunctivitis is a type I immediate hypersensitivity reaction. This means it’s triggered by allergens and involves the release of histamine and other substances mediated by immunoglobulin E (IgE) antibodies.
Subtypes of Simple Allergic Conjunctivitis:
Seasonal Allergic Conjunctivitis (SAC): SAC is a response to allergens that are present during specific seasons, such as pollen from trees and grasses. It is very common and often occurs alongside allergic rhinitis (hay fever).
Perennial Allergic Conjunctivitis (PAC): PAC is triggered by allergens that are present year-round, such as house dust mites, animal dander, and mold. It tends to have a more gradual onset and is a chronic condition.
Signs and Symptoms:
Symptoms: The primary symptoms are intense itching and a burning sensation in the eyes. This is often accompanied by a watery or mucus-like discharge and mild sensitivity to light (photophobia).
Signs: The conjunctiva will appear red (hyperemia) and swollen (chemosis), giving it a characteristic swollen and “juicy” appearance. Swelling of the eyelids (lid edema) is also common.
How it’s Diagnosed:
Diagnosis is typically based on:
The patient’s reported symptoms and the observed signs.
Testing to rule out infection (normal conjunctival flora).
Finding a high number of eosinophils (a type of white blood cell associated with allergies) in the eye discharge.
Treatment Options:
Elimination of Allergens: If possible, identifying and avoiding the specific allergens triggering the reaction is the ideal approach.
Topical Vasoconstrictors: Over-the-counter eye drops containing vasoconstrictors like naphazoline, antazoline, or tetrahydrozoline can provide quick relief from redness by narrowing the blood vessels in the conjunctiva.
Artificial Tears: Lubricating eye drops like carboxymethyl cellulose can soothe irritated eyes and sometimes provide relief in mild cases.
Mast Cell Stabilizers: Medications like sodium cromoglycate and nedocromil sodium are effective at preventing allergic reactions by stabilizing mast cells, which release histamine. They are particularly helpful for preventing recurrences in individuals with atopic conditions.
Steroids: In severe cases, topical steroid eye drops may be prescribed to reduce inflammation.
Cool Compresses: Applying cool water to the face with the head tilted downwards can help constrict blood vessels and reduce discomfort.
Other Forms of Conjunctivitis
Fungal Conjunctivitis:
Fungal conjunctivitis is less common and is often caused by Candida albicans. Newborns can contract this during birth if the mother has a vaginal yeast infection. A key sign is the presence of fine, white plaques on the conjunctiva. Treatment typically involves antifungal eye drops and ointments containing nystatin.
Parasitic Conjunctivitis:
In tropical regions, parasites such as those causing onchocerciasis (river blindness) and schistosomiasis (bilharzia) can lead to conjunctivitis.
Prevention of Conjunctivitis (General)
General preventive measures for conjunctivitis include:
Excluding individuals with active conjunctivitis from public places, such as schools or workplaces, until the eye discharge has completely stopped.
Maintaining good personal hygiene, especially thorough hand washing with soap and warm water.
Avoiding the sharing of personal items like towels and washcloths.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

