Introduction to Midwifery
Physiology and Management 3rd Stage of Labor
Table of Contents
THE PROCESS OF PLACENTAL SEPARATION AND EXPULSION {PHYSIOLOGY}
It undergoes 3 steps which include:
- Placental separation
- Descent of the placenta
- Expulsion of the placenta
PLACENTAL SEPARATION
It is as a result of the following:
- The abrupt decrease in size of the uterine cavity
- The retraction process
- The formation of retro placental clot
BEFORE PLACENTAL SEPARATION
Per abdomen:
- Uterus become discoid in shape, firm in feel and ballotable
- Fundal height reaches slightly below the umbilicus
Per vagina:
- There may be slight trickling of blood
- Length of the umbilical cord as visible from the outside remains the same
SIGNS OF PLACENTAL SEPARATION {AFTER SEPARATION}
Per abdomen:
- Uterus become globular, firm and ballotable
- Fundal height is slightly raised
- Supra pubic bulging
Per vagina:
- Slight gush of fresh bleeding
- Lengthening of the cord
DESCENT OF THE PLACENTA
You will see the following:
- Sudden trickle or gush of fresh blood
- Lengthening of the umbilical cord
- Change in the shape of the uterus to globular
- Change in the position of the uterus
EXPULSION OF THE PLACENTA
The placenta may be expelled by:
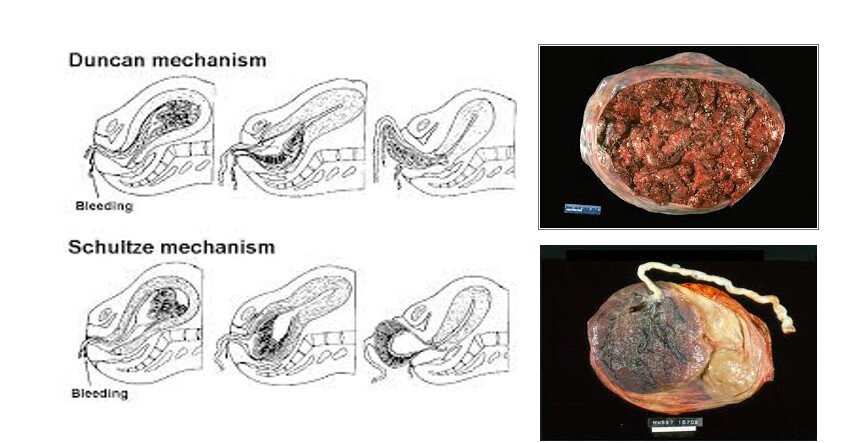
- The Schultz mechanism
- Mathew Duncan mechanism
HAEMOSTASIS It is achieved through:
- Retraction of the oblique uterine muscle fibres
- Vigorous uterine contraction following placental separation
- Transitory activation of the coagulation and fibrinolytic systems
MANAGEMENT OF THIRD STAGE OF LABOUR
- Do not massage the uterus before placental separation, except when partial separation has occurred by natural processes and excessive bleeding evident
ACTIVE MANAGEMENT OF THE THIRD STAGE OF LABOUR
- Ensure Active Management of the third stage of labor is offered to all mothers
- Administer a uterotonic agent within 1 minute of childbirth:
- Oxytocin (10 IU IV/IM)
- Misoprostol (400-600 μg orally)
- Carbetocin (100 mcg IV/IM)
- Ergometrine (0.2 mg IM)
- Delay cord clamping and cutting for 3 minutes or until the cord stops pulsating
- Clamp and cut the cord
- Put ties tightly around the cord at 2 cm and 5 cm from baby’s abdomen
- Cut between ties with sterile instrument
- Observe for oozing blood
CONTROLLED CORD TRACTION
- Wait for a contraction and then place left hand above the symphysis pubis hold back the uterus
- Wind the cord around the clamp and with the right apply firm steady traction on the cord in a downward, outward and then upward movement
- Receive the placenta with both hands when it appears at the vulva
- Deliver the membranes slowly
- Perform examination of the placenta immediately for completeness
- Massage the uterine fundus and expel clots from the uterus and vagina
POST-DELIVERY CARE
- Clean the vulva, and examine vaginal walls, cervix and perineum for tears and lacerations
- Repair episiotomy and/or tears after infiltrating with 1% lignocaine
- Assess blood loss (one kidney dish is approximately 500 mls of blood)
- Examine placenta for infarcts, retro placental clot, cord vessels, etc.
- If the mother has chosen to breastfeed, put the baby on breast within the first one hour
MONITORING MOTHER AND BABY EVERY 15 MINUTES FOR 2 HOURS
Mother:
- For emergency signs, e.g., difficulty in breathing, central cyanosis and shock using rapid assessment and management (RAM)
- Feel if uterus is well contracted
- Mood and behavior
- Record findings, treatments and procedures in Labor Progress Chart
- Give supportive care
- Do not leave the woman alone. Encourage her to be with her birth companion
Baby:
- Breathing: listen for grunting, look for chest in-drawing and fast breathing
- Warmth: Ensure the baby is kept warm by wrapping it in a dry clean cloth and put a cap on the head also check the temperature every after 30 minutes
- Feeding: Ensure that the baby is feeding adequately
- Check the cord for bleeding and ensure it is well ligatured
At the end of the third stage following the expulsion of the placenta, the fundus is expected to be about 4 cm below the umbilicus
COMPLICATIONS OF THE THIRD STAGE
- Postpartum haemorrhage
- Hematoma formation
- Retained placenta
- Inversion of uterus
- Shock
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowWe are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

