Introduction to Midwifery
Physiology and Management
Table of Contents
The second stage of labour begins with full dilatation of cervix and ends with the expulsion of the fetus.
PHASES AND DURATION OF SECOND STAGE OF LABOUR
The average duration is estimated to be 2 hours in primigravidae and 30 minutes in multigravida.
The stages are two and include:
- Propulsive phase: From full dilatation until head touches the pelvic floor
- Expulsive phase: Since the time mother has irresistible desire to bear down and push until the baby is delivered
PHYSIOLOGY OF SECOND STAGE OF LABOUR
The physiological changes result from a continuation of some forces which have been at work during the first stage of labor and a complex interplay of hormones including oxytocin, adrenaline and endorphins. These movements include:
- Descend
- Uterine action
- Rupture of membrane
- Soft tissue displacement
Descend
Descend of the fetal presenting part which began during the first stage of labour and reaches its maximum speed toward the end of the first stage of labour, continues its rapid pace through the second stage of labour until the pelvic floor.
Uterine Action
Contractions during the second stage are frequent, strong and slightly longer that is approximately every 2 minutes, lasting for 60-90 seconds. They are strong in intensity and become expulsive in nature. In natural course of labour there is often a lull or quiet period between first and second stage. The woman rests and may even nap. The fetal head descends through the pelvis the contractions become more forceful and the woman begins to voluntarily bear down with expiratory, grunty short pushes.
Rupture of Membrane
The membrane often rupture spontaneously at the onset of the second stage. The consequent drainage of liquor allows the hard round fetal head to be directly applied to the vaginal tissue and aid distension.
Soft Tissue Displacement
As the hard fetal head descends the soft tissue of the pelvis become displaced. Anteriorly the bladder is pushed upwards into the abdomen where it is at less risk of injury during fetal descent. Posteriorly the rectum becomes flattened into the sacral curve and the pressure of the advancing head expels any residual fecal matter. The levator ani muscles dilates, thin out and become displaced laterally. The perineal body is flattened, stretched and thinned. The fetal head become visible at the vulva advancing and receding during resting phase until crowning.
Hormones
- Oxytocin: As the labor progresses and the baby descends through the birth canal, oxytocin promotes rhythmic, coordinated contractions of the uterine muscles, helping to push the baby downward and expel it from the uterus
- Adrenaline (Epinephrine): Pressure on the cervix and pelvic floor triggers the release of adrenaline. It increases the strength and frequency of contractions, providing the extra energy needed for pushing. It also helps the mother to stay focused and alert during the intense physical exertion of childbirth
- Endorphins: These are natural pain killers released by the body helping the mother cope up with the intense sensations of labor and birth. It promotes feelings of euphoria and well-being
SIGNS OF SECOND STAGE OF LABOUR
- Expulsive contractions and urge to bear down
- Sweating
- Rupture of membrane
- Dilatation and gaping of anus and perineal bulging
- Progressive visibility of fetal head at the introitus
- Congestion of the vulva
MANAGEMENT OF SECOND STAGE OF LABOR
The Aims and Principles:
- To achieve delivery of a normal healthy child with minimal physical and psychological maternal effects
- Early anticipation, recognition and management of any abnormalities during labour course
- To prevent perineal tears
- To assist in the natural expulsion of the fetus slowly and steadily
General Measures
- The patient should be in bed
- Constant supervision
- Vaginal examination
- Preparation of equipment {should be on standby}
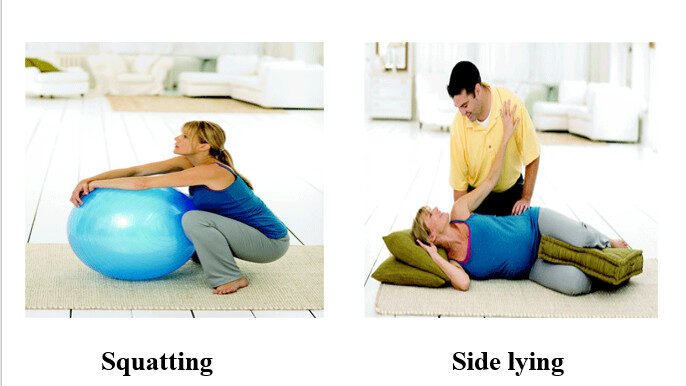
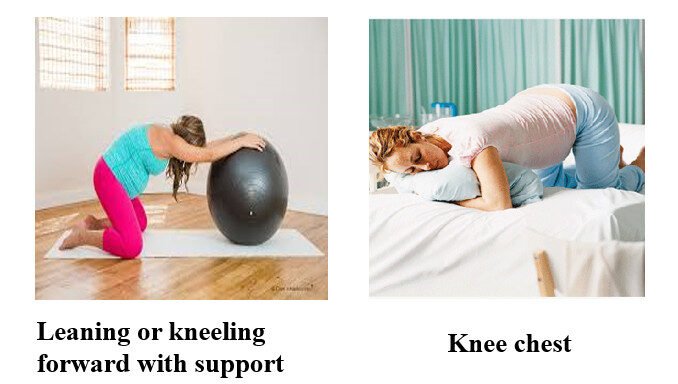
Position During Labor
- Standing supported squat
- Semi sitting
- Squatting
- Side lying
- Leaning or kneeling forward with support
- Knee chest
- Common position of labor: Lithotomy


Preparation of the Mother
- Change clothing into a hospital gown
- Provide preferable position
- Teach the mother on what she is going to do
- Explain to the mother the expectations of 2nd SOL
Preparation of the Unit
- Place obstetric delivery pack on the table
- Maintain sterility
- Cover the table with sterile drape
- Ensure availability of oxygen and suction source
- Maintain delivery record and newborn admission record
- Ensure availability of emergency drugs and neonatal resuscitation tray
Preparation for Delivery
- Positioning
- Midwife scrubs up and puts on sterile gown, boots, apron, mask and gloves {PPEs}, ensure you have baby’s clothes
- One sterile sheet is placed beneath the woman and another on her abdomen
- Essential aseptic procedures are remembered as 3C’s: clean hands, clean surfaces, clean cutting and ligaturing of the cord
- Get the obstetric delivery pack: 6 pieces of sterile gauze, two clamps (artery forceps), sterile gloves, umbilical clamps or sterile strings, scissors {straight and episiotomy}, bowl for holding placenta, sterile towels/cloths
- Oxytocin
Conduction of Delivery Undertakes 3 phases:
- Delivery of the head
- Delivery of the shoulders
- Delivery of the trunk
Delivery of Head
- Ask the woman to give only small pushes with contractions as the baby’s head delivers
- Place the fingers of one hand on the vertex to maintain flexion
- Once the baby’s head delivers, ask the woman not to push
- Wipe the baby’s mouth and nose with sterile gauze
- Feel around the baby’s neck for umbilical cord:
- If the cord is around the neck but is loose, slip it over the baby’s head
- If the cord is tight around the neck, double clamp and cut it before unwinding it from around the neck and cut
- Allow the baby’s head to turn spontaneously
- After the head turns, place a hand on each side of the baby’s head, tell the woman to push gently with next contraction
- Reduce tears by delivering one shoulder at a time. Move the baby’s head posteriorly to deliver the shoulder that is anterior. Do not panic, watch for restitution and external rotation of the head after a contraction
- Lift the baby’s head anteriorly to deliver the shoulder that is posterior
- Deliver the rest of the body {trunk} by lateral flexion
- Place the baby on the mother’s abdomen, thoroughly dry the baby and assess baby’s breathing
- Clamp, cut and tie the cord
- Ensure that the baby is kept warm on the mother’s chest
- Cover the baby in a soft, dry cloth and ensure the head is covered to prevent heat loss
- Palpate the abdomen to rule out presence of an additional baby(s) and proceed with active management of third stage
- Complete third stage of labor
- Ensure the woman is warm and comfortable and should be breastfeeding
Prevention of Perineal Tears Laceration
- More attention should be paid not to the perineum but to the controlled delivery of the head
- Delivery by early extension is to be avoided
- Spontaneous forcible delivery of the head is to be avoided
- To perform timely episiotomy
- To take care during delivery of the shoulders as the wider bisacromial diameter emerges out of the introitus
Episiotomy
Episiotomy A surgical planned incision on the perineum and posterior vaginal wall during the second stage of labor.
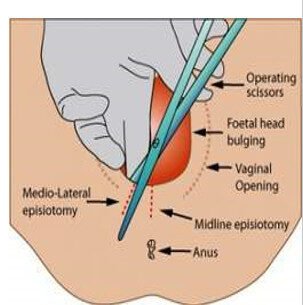
INDICATIONS
- Rigid perineum
- Anticipating perineal tear in case of big baby, shoulder dystocia
- Operative delivery like forceps or vacuum delivery
- Previous perineal surgery
IMMEDIATE CARE OF THE NEWBORN
- Baby should be placed on a clean flat surface covered with clean dry linen with the head slightly downwards soon after delivery
- Maintaining thermoregulation
- Suctioning to clear the air passages
- Maintaining cardio respiratory function
- Oxygen may be given as needed until the infant cries vigorously
- APGAR score
APGAR Score
| Category | 0 | 1 | 2 |
|---|---|---|---|
| Heart rate | Absent | <100 | >100 |
| Respiratory efforts | Absent | Slow irregular | Good crying |
| Muscle tone | Flaccid | Some flexion of extremities | Active motion |
| Reflex irritability | No response | Grimace | Vigorous cry |
| Colour | Blue, pale | Body pink, extremities blue | Completely pink |
Additional Immediate Care:
- Clamping and ligature of the cord ie 2-5 cm from abdomen
- Documenting urination/passage of meconium
- Administering vitamin K
- Prophylactic eye care
- Promoting parent-newborn bonding
- Quick check is made to detect any gross abnormality
NURSING CARE OF A PATIENT DURING 2ND SOL
- Never leave the patient alone once she has been transferred to the delivery room
- Alleviate anxiety by constantly communicating with the patient
- If possible, allow one caretaker to be with the patient during the delivery process
- Offer emotional support by constantly encouraging the patient
- Encourage the patient to rest between contractions and to push with contractions
- Position the patient’s legs for the lithotomy position
- Prepare the patient’s perineum
- Monitor the patient’s blood pressure and the fetal heart beat every 5 minutes and after each contraction
EVALUATIONS IN 2ND SOL
To evaluate the progress of second stage of labour check:
- Uterine contractions
- FHR for every 5 minutes – 15 minutes
- Descend and station of fetal head
- Progress through the mechanism of labor
RECORDS TO BE MAINTAINED
- Exact date and time of delivery
- Sex of the fetus
- Condition of the baby by APGAR after birth
- Type of delivery – spontaneous, forceps, vacuum
- Amount of blood loss
- Type of episiotomy if performed
- Condition of mother and baby throughout labour
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowGet in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

