Obstetric Anatomy and Physiology
The Uterus
Table of Contents
Definition
The uterus is a hollow, muscular, pear-shaped organ situated in the pelvic cavity between the bladder and rectum. It is the organ in which the fetus develops during pregnancy and from which menstruation occurs.
Situation
The uterus lies in the pelvic cavity, between the urinary bladder anteriorly and the rectum posteriorly. It is supported by ligaments and surrounded by peritoneum. It is positioned in such a way that it leans forward over the bladder in a position known as anteversion and anteflexion.
Shape
The uterus resembles an inverted pear. It is broad at the top (fundus) and tapers down to the cervix. The cavity of the uterus is triangular in shape.
Size
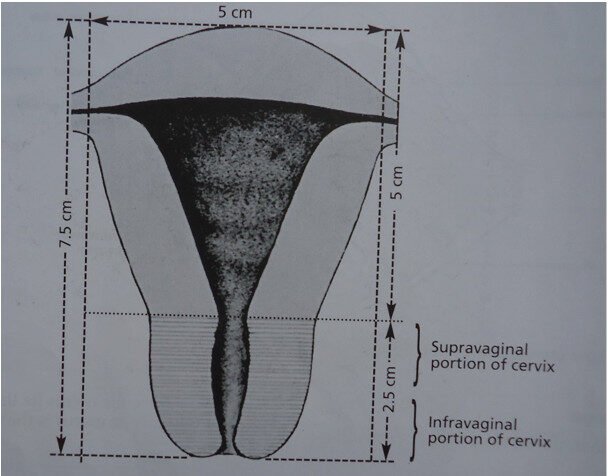
In a non-pregnant adult female, the uterus measures approximately:
- Length: 7.5 cm
- Width: 5 cm
- Thickness: 2.5 cm
The size varies with age, parity, and hormonal status. In a multiparous woman, the uterus may be slightly larger.
Measurements of the uterus
Gross Structure (Name the parts below)
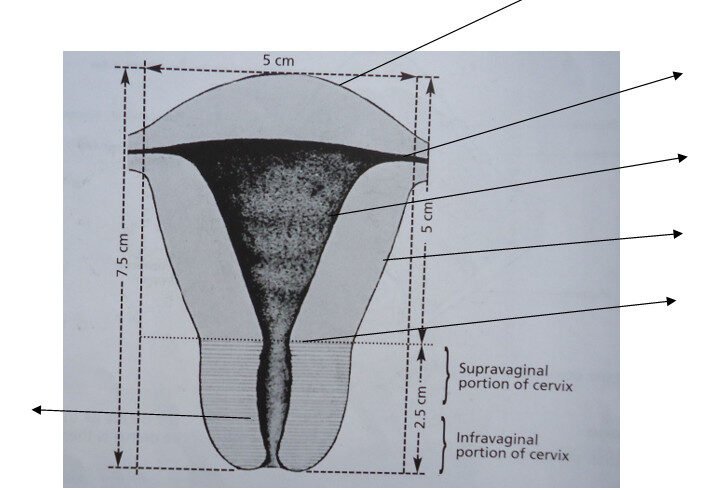
The uterus is divided into three main parts:
1. Fundus
- The upper rounded portion above the openings of the uterine tubes.
- It is the site where the uterine tubes enter the uterus.
2. Body
- The central portion between the fundus and cervix.
- It contains the uterine cavity, which is triangular in shape.
- The body forms the bulk of the uterus and is the site of implantation during pregnancy.
3. Cervix
- The lower narrow portion that projects into the vagina.
- It connects the uterine cavity to the vaginal canal via the cervical canal.
- The cervix is discussed in detail in Section 2.8.
Microscopic Structure
The uterine wall consists of three layers:
1. Endometrium (Inner lining)
- Composed of columnar epithelium and glandular tissue.
- Undergoes cyclical changes during the menstrual cycle:
- Proliferative phase: Thickens under the influence of estrogen.
- Secretory phase: Becomes glandular under progesterone.
- Menstrual phase: Sheds if fertilization does not occur.
- Provides the site for implantation of the fertilized ovum.
2. Myometrium (Middle muscular layer)
- Thick layer of smooth muscle fibers arranged in longitudinal, circular, and oblique directions.
- Responsible for uterine contractions during menstruation and labor.
- The muscle fibers increase in size and number during pregnancy.
3. Perimetrium (Outer serous layer)
- A thin layer of peritoneum covering the fundus and body.
- It is continuous with the broad ligament.
- It provides a smooth surface and reduces friction with surrounding organs.
Blood Supply
Diagram Showing Blood Supply To The Uterus
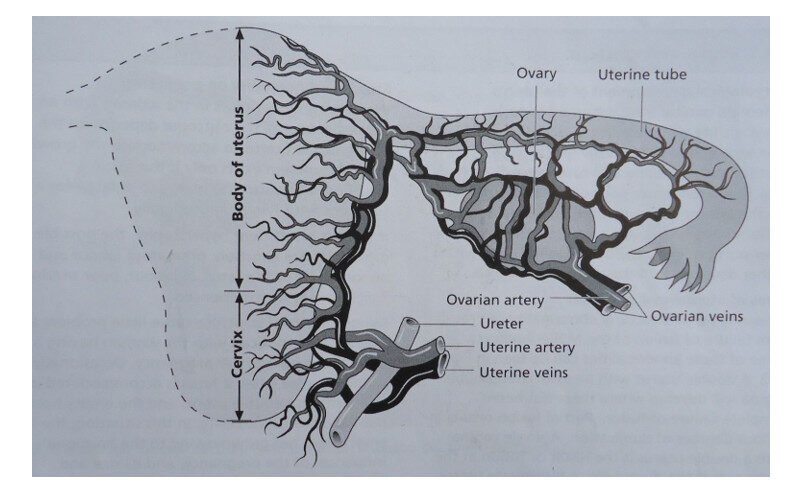
Arterial Supply
- Uterine arteries (branches of the internal iliac arteries).
- Anastomose with ovarian arteries.
Venous Drainage
- Uterine veins drain into the internal iliac veins.
- Venous plexuses surround the uterus and drain into systemic circulation.
Lymphatic Drainage
- Drains into the external iliac, internal iliac, and sacral lymph nodes.
- Important in the spread of infections and malignancies.
Nerve Supply
- Sympathetic and parasympathetic fibers from the uterovaginal plexus (Frankenhäuser plexus).
- Responsible for pain sensation during menstruation and labor.
- Autonomic innervation regulates uterine contractions and vascular tone.
Anatomical Relations
Anteriorly
- Urinary bladder
- Uterovesical pouch
Posteriorly
- Rectum
- Pouch of Douglas (rectouterine pouch)
Laterally
- Broad ligaments
- Ureters
Superiorly
- Intestinal loops
Inferiorly
- Cervix and vagina
Supports of the Uterus
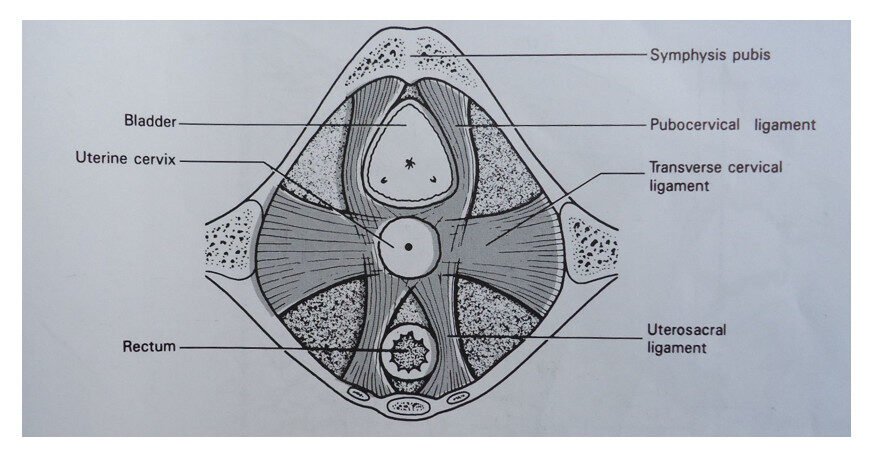
The uterus is supported by several structures:
1. Muscular Support
- Pelvic diaphragm: Composed of levator ani and coccygeus muscles.
- Perineal body: Central tendon of the perineum.
2. Fibromuscular Ligaments
- Uterosacral ligaments: Extend from the cervix to the sacrum.
- Cardinal (transverse cervical) ligaments: Extend from the cervix to the lateral pelvic walls.
- Pubocervical ligaments: Run anteriorly from the cervix to the pubic bone.
- Round ligaments: Extend from the uterine horns to the labia majora via the inguinal canal.
3. Peritoneal Support
- Broad ligaments: Double folds of peritoneum that support the uterus laterally.
Functions of the Uterus
- Menstruation: The endometrium sheds periodically in response to hormonal changes.
- Fertilization and Implantation: Provides the site for implantation of the fertilized ovum.
- Pregnancy: Supports and nourishes the developing fetus.
- Labor: Contracts to expel the fetus during childbirth.
- Involution: Returns to its non-pregnant state after delivery.
- Protection: Forms a barrier against ascending infections during pregnancy via the cervical mucus plug
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowWe are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

