Obstetric Anatomy and Physiology
Varieties of the Placenta
Table of Contents
VARIETIES OF THE PLACENTA (ANATOMICAL VARIATIONS)
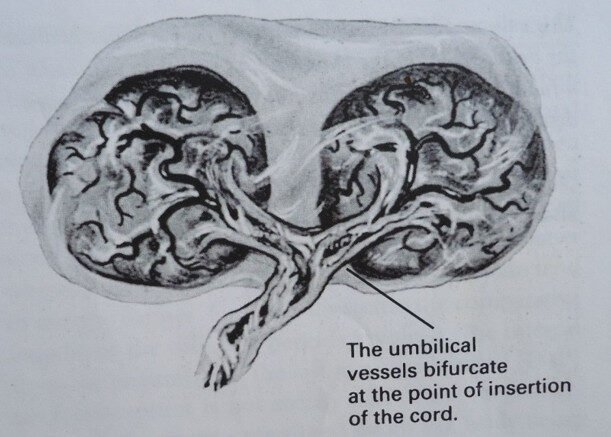
1. PLACENTA BI-PARTITA (TRIPARTITE)
This occurs when there are two (Bi-partita) or three (Tri-partite) complete lobes. Their blood vessels unite before joining the umbilical cord. The umbilical cord is single but supplies both/all lobes. In most cases, no complications are associated with this.
Dangers to the Mother: Too large a surface area of the placental site, which can cause Postpartum Hemorrhage (P.P.H.).
Bipartite placenta
2. PLACENTA ACCRETA
This is a placenta that embeds deeply in the uterine muscle instead of remaining confined to the endometrium. The placenta will not separate during the third stage of labor. This failure of separation may necessitate the removal of the uterus (a doctor may perform a hysterectomy).
3. PLACENTA PREVIA
The placenta is partly or wholly embedded in the lower uterine segment. If the uterus stretches, the placenta may start separating and cause Antepartum Hemorrhage (A.P.H.). This type may prevent normal vaginal delivery.
4. PLACENTA CIRCUMVALLATE
This involves a double fold of membranes surrounding the placental edges, which has very little significance.
Potential Danger: There is a possibility of causing A.P.H. due to Braxton Hicks contractions, which can cause the folded portion to detach from the uterine wall.
The circumvallate placenta

5. CALCIFICATION
These appear as gritty patches and feel like sand to the touch, resulting from excessive deposition of lime salts over the placenta. When pregnancy is advanced, the placenta can become too old to adequately nourish the fetus, and intra-uterine Anoxia may occur.
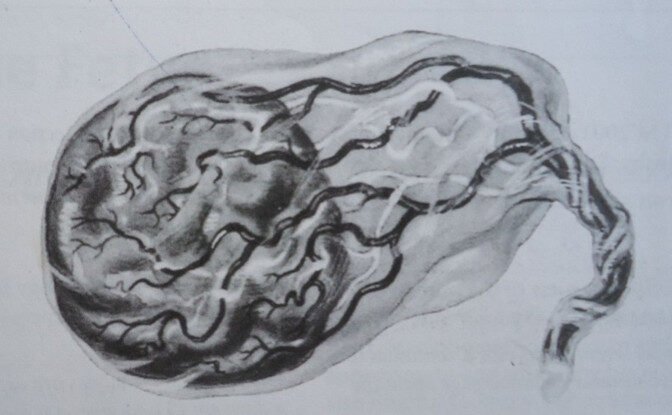
6. PLACENTA VELAMENTOSA
This usually occurs in a low-lying placenta where the blood vessels run in front of the presenting part of the fetus. During artificial rupture of membranes, the second stage of labor, or even spontaneous rupture, this can cause severe bleeding that may affect the mother or fetus, a condition called Vasa Previa.
Results:
Small-for-dates baby.
Anoxia to the fetus.
Retention of the placenta because the cord is inserted in the membranes, which may not be strong enough.
Velamentous insertion of the cord
PATHOLOGICAL CONDITIONS
1. Hydatidiform Mole
During the early weeks of placental development, the chronic villi undergo cystic degeneration. As a result, the embryo dies due to lack of nourishment, and this is considered an abnormal pregnancy.
2. Infarcts or Premature Degeneration
These are areas of enclosed chronic villi, appearing red in the early stage and white later with a solid cartilaginous consistency. They are produced by increased concentration of tissue Thromboplastin and always appear on the maternal surface.
They are associated with the normal degenerative process of the placenta at term but can be severe in cases of hypertension, syphilis, and P.E.T. (Pre-Eclampsia Toxemia) diseases.
3. Edema
This results in a large, pale, water-logged placenta weighing as much as half the weight of the fetus. It is associated with hydrops fetalis and is due to hemolytic disease of the newborn caused by Rhesus ISO-immunization. Other associated conditions include Diabetes and Syphilis.
EXAMINATION OF THE PLACENTA AND MEMBRANES
Reasons for Examination of the Placenta
To determine whether the placenta and the membranes have been completely delivered. If any part (like a cotyledon or a Succenturiate lobe) is retained in the uterus, there is a high risk of hemorrhage and infection.
To determine the weight, general appearance, and consistency of the placenta to provide information about the baby.
To check for specific abnormalities, either structural (e.g., abnormal position of the insertion of the cord, presence of more or fewer blood vessels) or diseases (e.g., infarcts, edema).
To remove blood clots from the placenta so that it can be weighed to estimate blood loss.
In the case of twins, to find out whether the twins were monozygotic (sharing one placenta) or dizygotic (if each had one placenta).
Method of Examination
The duty of a midwife as regards the management of labor is not complete until the placenta and membranes have been examined.
General Inspection: The placenta is held by the cord, and the membranes are left to hang to see if there is a hole where the baby passed. It is then placed on a flat surface, and the length of the cord is noted, along with any abnormality.
The Fetal Surface: Inspected to see the insertion of the cord and to see if the blood vessels terminate at the edge of the placenta. Also note if the membranes are complete and no blood vessels run through to the edge.
The Maternal Surface: All clots are removed and placed in a measuring jar. The cotyledons are inspected to see if they are complete. The placenta is held in a cupped hand so that cotyledons can be fitted into one another to confirm that none are missing. If the placenta is abnormally big or small, it should be weighed and kept for doctor’s inspection.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowWe are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

