Diploma in Midwifery
Anaemia in Pregnancy
Table of Contents
Anaemia during pregnancy is characterized by a lower-than-normal count of red blood cells or a decreased level of haemoglobin in the mother’s bloodstream. Clinically, pregnancy-related anaemia is defined when the haemoglobin concentration in the blood falls below 11 grams per deciliter (g/dl). This threshold indicates a significant reduction from healthy levels.
Essentially, anaemia signifies a diminished capacity of the blood to transport oxygen throughout the body. This can stem from a reduced quantity of red blood cells, a low concentration of haemoglobin within those cells, or a combination of both factors. Red blood cells are vital for carrying oxygen to all tissues and organs; therefore, insufficient levels in pregnancy can lead to a critical oxygen deficit for both the expectant mother and the developing fetus.
The condition may arise from:
A decrease in the total number of red blood cells circulating in the body.
A reduction in the concentration of haemoglobin protein contained within the red blood cells.
A situation where both the number of red blood cells and their haemoglobin concentration are simultaneously reduced.
Classifications/Degrees of Anaemia
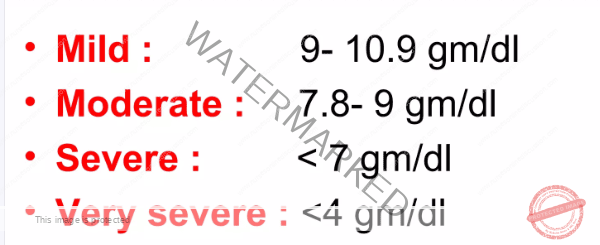
Anaemia during pregnancy is categorized into different levels based on the severity of the haemoglobin deficiency in the blood. These classifications help healthcare providers understand the extent of the anaemia and determine appropriate management strategies. The severity is generally determined by the measured haemoglobin levels and are as follows:
Mild Anaemia: This category indicates a slight reduction in haemoglobin. In cases of mild anaemia, the haemoglobin concentration in the blood typically falls within the range of 9.0 to 10.9 grams per deciliter (g/dL).
Moderate Anaemia: This level represents a more pronounced decrease in haemoglobin. When anaemia is classified as moderate, the haemoglobin levels are usually found to be between 7.0 and 8.9 grams per deciliter (g/dL).
Severe Anaemia: This is a serious condition characterized by a significant deficiency in haemoglobin. Severe anaemia is diagnosed when haemoglobin concentrations drop below 7.0 grams per deciliter (g/dL), indicating a critical need for intervention.
Very Severe Anaemia: This represents the most critical and dangerous level of anaemia. Very severe anaemia is identified when haemoglobin levels fall to extremely low levels, specifically below 4.0 grams per deciliter (g/dL). This level is a medical emergency and requires immediate and intensive treatment.
Causes of anaemia in Pregnancy
Anaemia during pregnancy can arise from a multitude of interconnected factors, broadly grouped into social, obstetric, medical, and other categories.
Socio-economic Factors:
Limited Knowledge of Food Utilization: A significant factor is a lack of awareness and understanding within communities about how to choose and prepare nutritious foods. This is particularly relevant to iron-rich dietary sources that are crucial during pregnancy. Insufficient knowledge about optimal food choices can lead to inadequate nutrient intake.
Financial Hardship: Poverty and limited financial resources directly impact access to adequate nutrition. Many individuals and families struggle to afford a consistently balanced diet that includes sufficient protein, iron, and other essential vitamins and minerals necessary to maintain healthy blood levels during pregnancy.
Country Instability/Insecurity: Situations of conflict, political unrest, and general insecurity within a country can significantly disrupt access to essential healthcare services and resources. Displacement of populations and unstable living conditions often lead to malnutrition, which in turn increases the risk of anaemia in pregnant women.
Cultural Beliefs and Superstitions: Deep-rooted cultural beliefs and traditional superstitions in some communities can inadvertently restrict the consumption of certain highly nutritious foods. For example, there might be cultural prohibitions against eating chicken, eggs, or specific types of meat during pregnancy, despite these being excellent sources of iron and protein.
Obstetrical Factors:
Frequent Childbearing: Women who experience pregnancies in quick succession, with short intervals between births, are at higher risk of developing anaemia. Closely spaced pregnancies can deplete the mother’s iron reserves over time as the body has less opportunity to replenish iron stores between pregnancies.
Repeated Haemodilution: During pregnancy, the body undergoes significant physiological changes, including a substantial increase in blood volume. This is a normal adaptation to support the growing fetus and placenta. However, this increase in blood volume leads to a dilutional effect, where the concentration of red blood cells and haemoglobin in the blood appears lower. This physiological haemodilution can contribute to a diagnosis of anaemia, even if the body’s red blood cell production is within a normal range.
Multiple Pregnancy: Carrying more than one fetus, such as in twin or triplet pregnancies, places an increased demand on the mother’s iron stores. Each fetus requires iron for its own growth and development, and the mother’s body also needs extra iron to support the expanded blood volume and increased oxygen transport necessary for multiple fetuses. This heightened demand can readily lead to iron deficiency anaemia.
Hyperemesis Gravidarum: Severe and persistent nausea and vomiting during pregnancy, a condition known as hyperemesis gravidarum, can significantly interfere with a woman’s ability to eat and absorb nutrients effectively. This can result in poor absorption of essential nutrients, including vitamin B12 and iron, both of which are crucial for the production of healthy red blood cells.
Pregnancy Complications and Blood Loss: Various obstetrical complications can lead to significant blood loss, thereby increasing the risk of anaemia. These conditions include spontaneous or induced abortions, ruptured ectopic pregnancies (where a fertilized egg implants outside the uterus), postpartum haemorrhage (excessive bleeding after childbirth – PPH), antepartum haemorrhage (bleeding from the vagina in later months of pregnancy – APH), and a history of heavy menstrual periods before pregnancy.
Medical Factors:
Recurrent Malaria Infections: Frequent episodes of malaria infection are a significant cause of anaemia, particularly in malaria-endemic regions. The malaria parasite directly invades and destroys red blood cells as part of its life cycle, leading to a reduction in red blood cell count and contributing to anaemia.
Hookworm Infestation: Infestation with hookworms, a type of parasitic worm, is another major cause of anaemia, especially in areas with poor sanitation. Hookworms live in the intestines and feed on blood, causing chronic blood loss from the intestinal tract. This continuous blood loss leads to iron deficiency and subsequently anaemia.
Systemic Infections: Various types of infections can impair the body’s ability to produce red blood cells effectively, thereby contributing to anaemia. These include severe infections like septicemia (blood poisoning), tuberculosis (TB), and other chronic infections that place a strain on the body’s resources and disrupt normal blood cell production processes.
Sickle Cell Anaemia: Sickle cell anaemia is an inherited genetic blood disorder. Individuals with this condition produce abnormal haemoglobin, which causes red blood cells to become sickle-shaped, rigid, and fragile. These abnormal red blood cells are prematurely destroyed (haemolysed) by the body, resulting in chronic anaemia.
Medications: Certain types of medications can have the side effect of interfering with the production of red blood cells in the bone marrow. For example, chloramphenicol, an antibiotic, is known to have this potential adverse effect and can contribute to the development of anaemia in susceptible individuals.
Other Factors:
Dietary Deficiencies: Inadequate dietary intake of key nutrients is a primary driver of anaemia, particularly nutritional anaemia. Deficiencies in iron, folate (vitamin B9), and vitamin B12 are especially common contributing factors. These nutrients are essential building blocks and cofactors for the production of healthy red blood cells.
Underlying Medical Conditions: Certain pre-existing medical conditions can impair the body’s ability to produce or maintain healthy red blood cell levels, predisposing individuals to anaemia. These conditions include chronic diseases such as celiac disease (an autoimmune disorder affecting nutrient absorption), chronic kidney disease, and certain types of cancers that can affect bone marrow function or nutrient utilization.
History of Pre-existing Anaemia: Women who have a history of anaemia prior to becoming pregnant are at a significantly higher risk of experiencing anaemia again during pregnancy. Pre-existing anaemia indicates underlying vulnerabilities in red blood cell production or iron stores that pregnancy can exacerbate.
Types of Anaemia
Anaemia can be classified into different types based on its underlying cause and mechanisms. Understanding these classifications is crucial for diagnosis and targeted treatment.
Physiological Anaemia:
Physiological anaemia, also known as dilutional anaemia of pregnancy, is a temporary and generally benign decrease in haemoglobin levels that occurs as a normal physiological adaptation to pregnancy. It is not a true anaemia in the pathological sense, but rather a consequence of the body’s adaptation to support the developing fetus.
Haemodilution: The primary mechanism of physiological anaemia is haemodilution. During pregnancy, there is a substantial increase in plasma volume (the fluid component of blood) relative to the increase in red blood cell mass. Blood volume can expand by 25-40% to meet the circulatory demands of the growing uterus, placenta and fetus. This disproportionate increase in plasma volume dilutes the concentration of haemoglobin in the blood, leading to a lower measured haemoglobin level, even though the total number of red blood cells may have increased or remained relatively stable.
Increased Iron Demand: While haemodilution is the main factor, the growing fetus also places an increased demand on the mother’s iron stores, particularly from the second trimester onwards. The fetus needs iron to build its own red blood cells and iron stores. This increased iron utilization can contribute to a relative iron deficiency, further influencing haemoglobin levels in physiological anaemia.
Physiological anaemia is typically mild and is generally considered a normal variation in pregnancy. Haemoglobin levels usually return to pre-pregnancy levels after childbirth, once the blood volume returns to its normal state. It is important to differentiate this physiological change from pathological anaemia which requires intervention.
Nutritional Anaemia:
Nutritional anaemia is the most common type of anaemia, and it results from a deficiency in one or more essential nutrients that are required for the production of red blood cells in the bone marrow. This type of anaemia is largely preventable and treatable with dietary modifications and appropriate supplementation.
Nutritional anaemia can manifest in various forms depending on the specific nutrient deficiency:
Iron Deficiency Anaemia: This is by far the most prevalent type of anaemia globally, particularly during pregnancy. It arises from insufficient intake, poor absorption, or increased loss of iron. Iron is a central component of haemoglobin, the protein in red blood cells responsible for oxygen transport. When iron stores are depleted, the body cannot produce sufficient haemoglobin. As a result, red blood cells produced are often smaller and paler than normal (microcytic and hypochromic anaemia). The increased iron demands of the developing fetus, particularly from the late second trimester onwards, significantly exacerbate the risk of iron deficiency. Conditions like severe morning sickness (hyperemesis gravidarum) can further contribute to iron deficiency by reducing dietary intake and impairing iron absorption from food.
Folate Deficiency Anaemia (Megaloblastic Anaemia): Folate, also known as vitamin B9, is crucial for DNA synthesis and cell division, including the production of red blood cells. A deficiency in folate disrupts DNA synthesis in the bone marrow, leading to the abnormal development of red blood cell precursors. This results in the production of large, immature red blood cells called megaloblasts, which are less effective at carrying oxygen. This type of anaemia is characterized by these abnormally large red blood cells.
Vitamin B12 Deficiency Anaemia (Pernicious Anaemia): Vitamin B12 is another essential vitamin vital for DNA synthesis, cell growth, and the maturation of red blood cells in the bone marrow. Similar to folate deficiency, a lack of vitamin B12 also leads to megaloblastic anaemia, with the production of large, immature and dysfunctional red blood cells. Inadequate protein intake can sometimes indirectly contribute to vitamin B12 deficiency, as protein is necessary for the absorption of vitamin B12.
Vitamin C Deficiency: Vitamin C, or ascorbic acid, is not directly involved in red blood cell production itself, but it plays a crucial role in enhancing the absorption of non-haeme iron (the type of iron found in plant-based foods) from the diet. A deficiency in vitamin C can therefore indirectly worsen iron deficiency anaemia by reducing the body’s ability to absorb iron effectively from food sources.
Aplastic Anaemia:
Aplastic anaemia is a rare but very serious and potentially life-threatening condition. It is characterized by a severe suppression of bone marrow activity. The bone marrow is the primary site of blood cell production in the body. In aplastic anaemia, the bone marrow fails to produce sufficient quantities of all types of blood cells, including red blood cells (leading to anaemia), white blood cells (leading to increased susceptibility to infections), and platelets (leading to bleeding problems).
Bone Marrow Failure: The underlying cause of aplastic anaemia is bone marrow failure. This means that the specialized cells in the bone marrow responsible for generating blood cells (haematopoietic stem cells) are damaged or destroyed, or their function is significantly impaired. Bone marrow failure can be triggered by various factors:
Drug-induced: Prolonged use of certain medications, such as chloramphenicol, and some anti-rheumatic drugs, can have a toxic effect on the bone marrow, leading to suppression of blood cell production.
Radiation Exposure: Exposure to high doses of ionizing radiation, such as in radiation therapy or nuclear accidents, can damage bone marrow cells and impair their ability to produce blood cells.
Diseases: Certain underlying diseases, including various types of leukemia (cancers of the blood and bone marrow), other forms of cancer that metastasize to the bone marrow, and autoimmune diseases (where the body’s immune system attacks its own tissues), can directly affect or damage bone marrow function.
Toxins: Exposure to certain toxic chemicals, such as benzene and some pesticides, can also damage bone marrow cells and lead to bone marrow failure.
In many cases, the exact cause of aplastic anaemia remains unknown (idiopathic). Aplastic anaemia requires urgent and intensive medical attention. Treatment options may include blood transfusions to manage the blood cell deficiencies, medications to suppress the immune system (if an autoimmune cause is suspected), and in severe cases, bone marrow transplantation to replace the damaged bone marrow with healthy stem cells.
Haemorrhagic Anaemia:
Haemorrhagic anaemia is a type of anaemia that develops as a direct consequence of excessive blood loss. When the body loses a significant amount of blood, it loses red blood cells along with it, leading to a reduction in the circulating red blood cell count and haemoglobin levels.
Haemorrhagic anaemia can result from both acute and chronic blood loss, which can occur due to a wide range of factors:
Obstetrical Causes:
Frequent Childbearing: As mentioned previously, closely spaced pregnancies can increase the risk of haemorrhagic anaemia because of potential blood loss during each delivery, particularly if iron stores are not adequately replenished in between pregnancies.
Obstetrical Complications: Various pregnancy complications, such as abortions (spontaneous or induced), postpartum haemorrhage (PPH – excessive bleeding after childbirth), and antepartum haemorrhage (APH – bleeding before delivery), are all direct causes of significant blood loss and can lead to haemorrhagic anaemia.
Ruptured Ectopic Pregnancy: A ruptured ectopic pregnancy, where a fertilized egg implants and grows outside the uterus (typically in a fallopian tube), is a medical emergency that causes significant internal bleeding and can rapidly lead to haemorrhagic anaemia.
Trauma and Accidents: Significant physical trauma, accidents causing injuries, or major surgical procedures can all result in acute and substantial blood loss, leading to haemorrhagic anaemia.
Gastrointestinal Bleeding: Chronic or acute bleeding from the gastrointestinal tract can be a cause of haemorrhagic anaemia. Conditions that can cause GI bleeding include peptic ulcers in the stomach or duodenum, gastritis (inflammation of the stomach lining), esophageal varices (swollen veins in the esophagus), haemorrhoids (piles), and bowel cancers.
Haemorrhagic anaemia can be further categorized based on the rate and duration of blood loss:
Acute Blood Loss: Acute haemorrhagic anaemia results from sudden and significant blood loss that occurs over a short period. This type of blood loss is often caused by traumatic injuries, major surgery, or sudden internal bleeding events. The body may not have enough time to compensate for the rapid loss of blood, leading to a rapid drop in red blood cell count and haemoglobin.
Chronic Blood Loss: Chronic haemorrhagic anaemia develops gradually over time due to persistent, slow blood loss. This type of blood loss may be less noticeable initially but over time, it depletes the body’s iron stores and reduces red blood cell production capacity. Common causes of chronic blood loss include heavy menstrual periods (menorrhagia) in women and slow, ongoing bleeding from the gastrointestinal tract (e.g., from ulcers or polyps).
Haemorrhagic anaemia can range in severity, from mild to life-threatening, depending on the amount and rate of blood loss. Treatment for haemorrhagic anaemia primarily focuses on identifying and stopping the source of bleeding. In cases of significant blood loss, treatment may also involve blood transfusions to replace the lost blood volume and red blood cells, and iron supplementation to replenish iron stores.
Haemolytic Anaemia:
Haemolytic anaemia is a type of anaemia characterized by the premature and accelerated destruction of red blood cells, a process called hemolysis. Normally, red blood cells have a lifespan of about 120 days in circulation before they are naturally removed and replaced by new cells. In haemolytic anaemia, red blood cells are destroyed at a faster rate than the bone marrow can produce new ones to replace them, leading to a shortage of healthy red blood cells in circulation.
Haemolytic anaemia can be caused by factors that are intrinsic to the red blood cells themselves (internal defects) or by factors that are extrinsic, meaning they originate from outside the red blood cells and cause their destruction.
Intrinsic Defects (Internal Factors): Haemolysis can be triggered by abnormalities or defects within the red blood cells themselves. These intrinsic defects are often genetic in origin:
Sickle Cell Disease: Sickle cell disease is a genetic disorder caused by a mutation in the gene that codes for haemoglobin. This mutation leads to the production of an abnormal form of haemoglobin called haemoglobin S. When haemoglobin S is deoxygenated, it causes red blood cells to change shape, becoming rigid and sickle-shaped instead of their normal flexible, disc-like form. Sickle-shaped red blood cells are fragile, less flexible, and prone to premature destruction (hemolysis). This chronic hemolysis is the hallmark of sickle cell anaemia.
Thalassemia: Thalassemia encompasses a group of inherited genetic blood disorders characterized by defects in the production of globin chains, which are essential components of haemoglobin. There are two main types: alpha-thalassemia and beta-thalassemia, depending on which globin chains are affected. These genetic defects lead to reduced or absent production of normal haemoglobin, resulting in weakened and abnormally shaped red blood cells that are more susceptible to destruction (hemolysis).
Extrinsic Factors (External Factors): Haemolysis can also be triggered by factors originating from outside the red blood cells that cause them to be destroyed prematurely:
Infections: Certain types of infections can cause haemolytic anaemia. Severe infections such as septicemia (blood poisoning), pyelonephritis (kidney infection), and streptococcal bacterial infections can release toxins or trigger immune responses that lead to the destruction of red blood cells.
Diseases (Malaria): Malaria, a mosquito-borne parasitic disease, is a significant cause of haemolytic anaemia, particularly in malaria-endemic regions. The malaria parasite infects red blood cells and multiplies within them, eventually causing the red blood cells to rupture and be destroyed (hemolysis). This parasitic destruction of red blood cells is a key mechanism of malaria-induced anaemia.
Mismatched Blood Transfusion: Receiving a blood transfusion of incompatible blood type can trigger a severe and rapid haemolytic reaction. The recipient’s immune system recognizes the transfused red blood cells as foreign and mounts an immune attack, leading to the destruction (hemolysis) of the transfused red blood cells.
Immune Reactions: In certain autoimmune disorders, or following certain blood transfusions or organ transplants, the body can produce antibodies that mistakenly target and attack its own red blood cells. These antibodies coat the red blood cells and cause their premature destruction by the immune system (autoimmune haemolytic anaemia).
Drugs: Certain medications can, in susceptible individuals, induce haemolytic anaemia as a side effect. For example, primaquine, an antimalarial drug, can trigger haemolysis in people with glucose-6-phosphate dehydrogenase (G6PD) deficiency, a genetic condition that makes red blood cells more vulnerable to oxidative damage.
Pernicious Anaemia:
Pernicious anaemia is a specific type of megaloblastic anaemia, meaning it is characterized by the presence of abnormally large, immature red blood cells (megaloblasts). Pernicious anaemia is caused by a deficiency in vitamin B12, but specifically due to a lack of intrinsic factor.
Intrinsic Factor Deficiency: Intrinsic factor is a protein produced by parietal cells in the lining of the stomach. It is essential for the absorption of vitamin B12 from the diet in the small intestine. In pernicious anaemia, there is a deficiency of intrinsic factor, which impairs the body’s ability to absorb vitamin B12 effectively, leading to vitamin B12 deficiency and subsequent megaloblastic anaemia.
Pernicious anaemia is less common during childbearing years, but it can occur due to several factors:
Autoimmune Destruction of Parietal Cells: In the vast majority of cases, pernicious anaemia is caused by an autoimmune reaction. The body’s immune system mistakenly attacks and destroys the parietal cells in the stomach lining. This autoimmune destruction of parietal cells leads to a significant reduction or complete absence of intrinsic factor production, resulting in vitamin B12 malabsorption.
Diseases of the Stomach: Certain diseases that affect the stomach lining or stomach structure can interfere with intrinsic factor production. Conditions such as stomach cancer, atrophic gastritis (chronic inflammation and thinning of the stomach lining), or surgical removal of part of the stomach (gastrectomy) can reduce or eliminate parietal cells and consequently intrinsic factor production.
Hyperemesis Gravidarum: Severe and prolonged hyperemesis gravidarum (severe morning sickness) can, in rare cases, lead to vitamin B12 deficiency. The persistent vomiting and reduced food intake in hyperemesis can result in poor vitamin B12 absorption, contributing to deficiency and potentially pernicious anaemia over time.
Gastrectomy or Gastric Bypass Surgery: Surgical procedures that involve partial or complete removal of the stomach (gastrectomy) or gastric bypass surgery (used for weight loss) can significantly reduce or eliminate the production of intrinsic factor in the stomach. This can lead to long-term vitamin B12 malabsorption and the risk of developing pernicious anaemia.
Other Causes: Certain conditions that affect the small intestine can also interfere with vitamin B12 absorption, even if intrinsic factor production is normal. These include Crohn’s disease and celiac disease. These conditions can damage the lining of the small intestine, impairing the absorption of various nutrients, including vitamin B12.
Signs and Symptoms of Anaemia in Pregnancy
The presentation of anaemia in pregnancy can vary, influenced by the severity of the condition and its underlying cause.
On History Taking
General Body Weakness: A common complaint is feeling unusually tired and weak overall. This fatigue arises because anaemia reduces the blood’s ability to carry oxygen, leading to insufficient oxygen supply to the body’s tissues and muscles, resulting in fatigue.
Dizziness and Faintness: Experiencing dizziness or feeling faint, particularly when standing up quickly. This occurs because reduced red blood cell count leads to decreased oxygen delivery to the brain, making the individual feel lightheaded and unstable.
Palpitations: An awareness of a rapid or irregular heartbeat. To compensate for the reduced oxygen-carrying capacity of the blood, the heart may beat faster and harder to circulate more blood and deliver sufficient oxygen throughout the body.
Loss of Appetite (Anorexia): A noticeable decrease in hunger or desire to eat. Anaemia can sometimes affect appetite, although the exact mechanism isn’t fully understood, it’s thought to be related to general unwellness and body imbalances.
Headaches: Frequent or persistent headaches may develop. Insufficient oxygen supply to the brain, a direct consequence of anaemia, can trigger headaches.
Breathlessness: Feeling unusually short of breath, especially with exertion or even at rest in severe cases. With less oxygen being carried in the blood, the lungs have to work harder to try and get more oxygen into the system, leading to breathlessness.
Shortness of Breath: A sensation of difficulty in getting enough air. The heart needs to pump harder and faster to circulate the reduced amount of oxygen available in the blood, leading to the feeling of being short of breath.
History of Heavy Bleeding: Enquiring about any past episodes of significant blood loss. Conditions like injuries, surgeries, or gastrointestinal bleeding can deplete iron stores and increase the risk of anaemia.
On Examination
Pale Mucous Membranes and Conjunctiva: Observing paleness in areas like the inner eyelids (conjunctiva), gums, lips, tongue, palms of hands, and soles of feet. These areas, normally pink due to blood flow, appear paler in anaemia due to the reduced concentration of haemoglobin in the blood, which gives blood its red colour.
Distention of the Jugular Veins: In severe anaemia, the jugular veins in the neck might become visibly swollen. This can indicate fluid overload or heart strain as the body tries to compensate for reduced oxygen carrying capacity and blood volume imbalances can occur.
Edema (Swelling): Noticing swelling, particularly in the ankles and feet, or in more severe cases, generalized swelling throughout the body. Severe anaemia can sometimes lead to fluid retention and edema, though this is less directly related to anaemia itself and more to associated complications or underlying conditions.
Enlarged Spleen and Liver: During abdominal examination, the spleen and liver might be felt to be larger than normal. Enlargement of these organs can occur in certain types of anaemia, especially haemolytic anaemias where there is increased red blood cell destruction or in conditions that affect blood cell production and storage.
Jaundice: Yellowing of the skin and the whites of the eyes. Jaundice can occur in haemolytic anaemias where the rapid breakdown of red blood cells releases bilirubin, a yellow pigment, into the bloodstream.
Cold Hands and Feet: Feeling coldness in the extremities, like hands and feet. Reduced blood circulation, a consequence of anaemia, can lead to decreased blood flow to peripheral areas, causing them to feel cold.
Laboratory Tests
Haemoglobin Level: This is the primary blood test for diagnosing anaemia. It measures the concentration of haemoglobin in the blood. A haemoglobin level below the normal range for pregnancy (typically less than 11 g/dL) confirms the presence of anaemia.
Increased Susceptibility to Infections: While not a direct laboratory test, anaemia can weaken the immune system. This lowered immunity makes pregnant women more vulnerable to various infections due to reduced oxygen and nutrient supply to immune cells.
Diagnosis
Diagnosis of anaemia is achieved through a combination of medical history, physical examination, and laboratory investigations.
History: A thorough medical history is taken, focusing on the patient’s symptoms, dietary habits, past medical conditions, medications being taken, and potential exposures to factors that could cause anaemia. This helps to identify potential causes and risk factors.
Physical Examination: A careful physical examination is conducted to look for visible signs of anaemia, such as pallor (pale skin and mucous membranes), edema (swelling), and to assess for organ enlargement, providing clues about the severity and possible causes.
Laboratory Investigations: A series of blood tests are crucial to confirm the diagnosis and determine the type and cause of anaemia.
Haemoglobin Estimation: This is the fundamental test to confirm anaemia by measuring the haemoglobin concentration in the blood.
Packed Cell Volume (PCV): Also known as haematocrit, PCV measures the proportion of blood volume occupied by red blood cells. It provides another indication of red blood cell concentration in the blood.
Blood Film: A blood sample is examined under a microscope to assess the characteristics of red blood cells. This analysis can reveal:
Microcytosis and Hypochromia: Red blood cells that are smaller than normal (microcytic) and paler in colour (hypochromic) typically suggest iron deficiency anaemia.
Megaloblastic Cells: Large, abnormally developed red blood cells (megaloblasts) are indicative of vitamin B12 or folate deficiency anaemia.
Sickle Cells: The presence of crescent or sickle-shaped red blood cells is diagnostic for sickle cell anaemia.
Target Cells: Red blood cells with a dark center and outer ring, resembling a bullseye (target cells), can be seen in thalassaemia and other conditions.
Reticulocytes: Counting reticulocytes, which are immature red blood cells, can assess the bone marrow’s response to anaemia and its ability to produce new red blood cells.
Blood Smear for Malarial Parasites: In malaria-prone regions, a blood smear is examined for the presence of malaria parasites to rule out malaria as a cause of anaemia.
Sickling Test: This test is performed to specifically detect the presence of sickle haemoglobin in cases where sickle cell disease is suspected.
Coombs Test: This test identifies antibodies attached to red blood cells. A positive Coombs test suggests autoimmune haemolytic anaemia where the body’s immune system is destroying its own red blood cells.
Bone Marrow Examination: In complex or unclear cases, a bone marrow aspiration and biopsy may be performed to directly assess the bone marrow’s ability to produce blood cells and to identify any abnormalities in blood cell production.
Urinalysis: Urine sample analysis is done to check for the presence of protein, which could suggest kidney disease as a contributing factor to anaemia, and to look for any red blood cells or other unusual components in the urine.
Stool Examination: A stool sample is examined for the presence of intestinal parasites, such as hookworms, which can cause chronic blood loss and lead to anaemia.
Haemoglobin Electrophoresis: This specialized test is used to identify and quantify different types of haemoglobin in the blood, and it is crucial for confirming the diagnosis of sickle cell disease and thalassaemia.
Iron Requirements During Pregnancy
Iron needs significantly increase during pregnancy to support both maternal and fetal health. The estimated total iron requirement during pregnancy is approximately 1,500 mg, distributed across various needs:
Increase in Maternal Haemoglobin (400-500 mg): The mother’s blood volume expands considerably during pregnancy to accommodate the growing fetus and placenta. This expansion necessitates an increased production of red blood cells, which require iron as a core component of haemoglobin, the oxygen-carrying protein.
The Fetus and Placenta (300-400 mg): The developing fetus actively accumulates iron during gestation, especially in the later trimesters, to build its own red blood cell supply and establish iron stores for postnatal life. The placenta also needs iron for its growth, function and to facilitate nutrient transfer to the fetus.
Replacement of Daily Loss (250 mg): Even in non-pregnant state, the body loses a small amount of iron daily through natural processes like shedding of cells from the skin, digestive tract, and in urine. These daily iron losses need to be replenished through dietary intake to maintain iron balance, and this requirement continues during pregnancy.
Replacement of Blood Lost at Delivery (200 mg): Childbirth typically involves some blood loss. Iron is needed to replace the red blood cells and haemoglobin lost during labour and delivery, ensuring the mother recovers adequately post-partum.
Other Essential Nutrients:
In addition to iron, other nutrients are crucial in preventing and managing anaemia during pregnancy:
Elemental Iron: Pregnant women are generally recommended to have a daily intake of 30 to 60 mg of elemental iron, usually through iron supplements, to meet their increased needs.
Folic Acid: Folic acid (vitamin B9) is vital, especially in early pregnancy, to prevent neural tube defects in the developing fetus. A daily intake of 400 micrograms (0.4 mg) is generally recommended to support fetal development and maternal red blood cell production.
Effects of anaemia on pregnancy and labour
Anaemia in pregnancy can have significant adverse effects on both the mother and the developing fetus, impacting the course of pregnancy and labour.
Effects on Pregnancy:
General Body Fatigue: Persistent and overwhelming tiredness is a major symptom. Reduced oxygen delivery throughout the body due to anaemia leads to widespread fatigue, breathlessness even with minimal activity, heart palpitations, and frequent headaches, significantly affecting the mother’s quality of life.
Placental Insufficiency: Inadequate oxygen supply to the placenta can compromise its function, leading to:
Intra-Uterine Fetal Death (IUFD): Severe placental insufficiency can result in fetal demise due to lack of sufficient oxygen and nutrients reaching the fetus.
Small for Gestational Age (SGA): Reduced nutrient and oxygen delivery to the fetus can impair growth, resulting in the baby being born smaller than expected for their gestational age (SGA).
Neonatal Death: Anaemia during pregnancy is associated with an increased risk of death in the newborn period, often linked to complications arising from placental insufficiency and prematurity.
Abortion and Premature Labour: Anaemia has been linked to an increased risk of both spontaneous abortion (miscarriage) and preterm birth (premature labour and delivery), potentially due to the stress it places on the mother’s body and the developing fetus.
Increased Risk of Complications: Anaemia during pregnancy elevates the risk of several serious maternal complications:
Postpartum Haemorrhage (PPH): Anaemia can impair the blood’s clotting ability, making mothers more susceptible to excessive and dangerous bleeding after childbirth (PPH).
Heart Failure: To compensate for reduced oxygen levels, the heart has to work much harder to pump blood, increasing the risk of developing heart failure, particularly in women with pre-existing heart conditions.
Venous Thrombosis: Anaemia can lead to changes in blood viscosity and blood flow, potentially increasing the risk of blood clots forming in the veins (venous thrombosis), a potentially life-threatening condition.
Infections: Anaemia can weaken the immune system, making pregnant women more vulnerable to various infections, both during pregnancy and after delivery.
Poor Lactation: Anaemia can negatively impact breast milk production and quality, potentially affecting the infant’s nutrition and health.
Effects on Labour:
Stress of Labour: Anaemic women may have reduced physiological reserves and find it harder to cope with the physical stress of labour. Even relatively minor blood loss during delivery can become dangerous for an anaemic mother.
Fetal and Maternal Distress: Low oxygen levels in the mother’s blood can lead to both fetal and maternal distress during labour. Fetal distress may necessitate interventions, and maternal exhaustion can complicate labour.
Increased Risk of Complications: Anaemia in labour increases the risk of several labour-related complications:
Instrumental Delivery: Fetal distress or maternal exhaustion due to anaemia may increase the likelihood of needing an instrumental delivery (using forceps or vacuum extraction) to expedite birth.
Postpartum Haemorrhage: As mentioned before, anaemia increases the risk of excessive bleeding after delivery.
Infection: Anaemic mothers are at higher risk of infections following childbirth.
Prolonged Labor: Anaemia might contribute to a longer and more exhausting labor process.
Management of anaemia in Pregnancy
The approach to managing anaemia in pregnancy depends on several factors including the severity of the anaemia, the gestational age of the pregnancy, and the underlying cause of the anaemia.
Early Pregnancy with Mild or Moderate anaemia in a Maternity Center and Hospital:
Outpatient Management: For cases of mild to moderate anaemia in early pregnancy, outpatient care may be sufficient in a maternity center setting:
Bed Rest: Advise the mother to rest adequately to reduce physical strain.
History Taking: A detailed history is taken to understand the woman’s diet, lifestyle, and living conditions to identify potential causes contributing to anaemia.
General Examination: A physical examination, possibly using a Tallquist haemoglobin colour scale book, is performed to estimate the degree of anaemia clinically.
Midwife Management: Midwives can effectively manage mild and moderate anaemia in early pregnancy through dietary advice and oral supplements.
Address Underlying Cause: Management focuses on addressing the identified underlying cause of anaemia through appropriate interventions.
Hospital Referral (Low Hb): If the haemoglobin level is found to be significantly low, typically below 60% (or severely anaemic levels in g/dL), the mother should be referred to a hospital for further, more intensive investigation and treatment.
Active Treatment for haemoglobin of 60% and Above: For haemoglobin levels of 60% (or equivalent in g/dL) and above in early pregnancy, active treatment in a maternity centre may include:
Antimalarial Medication: In areas where malaria is common, administering a prophylactic dose of antimalarial medication like three doses of Fansidar 960 mg tablets is advised.
Antihelminthic Medication: If hookworm infestation is suspected or common in the area, administer an antihelminthic medication like Mebendazole 200 mg twice daily for three days.
Iron and Folic Acid Therapy: Initiate iron supplementation with ferrous sulfate tablets (200 mg twice daily) and folic acid supplements (5 mg once daily).
Follow-up Review: Schedule a follow-up appointment after approximately 2 months to reassess haemoglobin levels and treatment effectiveness.
Referral for Late Moderate Anaemia: Note that moderate anaemia detected in late pregnancy should be referred to a hospital for further management even if it might have been manageable at a maternity centre in early pregnancy.
In the Hospital (for Moderate Anaemia or Referral): For mothers referred to the hospital or those presenting with moderate anaemia requiring hospital-level care:
Hospital Admission: Admit the mother to the antenatal ward for closer monitoring and management.
Detailed History: Obtain a detailed history focusing on diet, environmental factors, and hygiene practices.
Vital Signs Monitoring: Regularly monitor vital signs, including temperature, pulse rate, respiratory rate, and blood pressure.
Treat Underlying Cause: Diagnose and treat any identified underlying medical conditions contributing to anaemia.
Routine Nursing Care: Provide standard antenatal nursing care, ensuring comfort and well-being.
Hygiene Promotion: Maintain strict hygiene to prevent infections, which can worsen anaemia.
High-Protein Diet: Provide a diet rich in protein to support red blood cell production and overall health.
Severe anaemia in Early and Late Pregnancy:
In a Maternity Center (Severe Anaemia): Due to the severity, immediate referral to a hospital is crucial.
In the Hospital (Severe Anaemia): Hospital management of severe anaemia involves urgent and intensive care:
Hospital Admission: Immediate hospital admission is necessary.
History and Investigations: Obtain a focused history and conduct necessary investigations to determine the cause and severity.
Immediate Resuscitation: Emergency resuscitation measures are taken immediately.
Blood Transfusion: Blood transfusion with packed red blood cells is the most effective way to rapidly increase haemoglobin levels and oxygen-carrying capacity.
Parenteral Iron (Inferon): If blood transfusion is not immediately available, intravenous iron dextran (Inferon) infusion may be considered as an alternative, although it is slower acting. Note: Inferon total dose infusion is generally reserved for severe anaemia close to delivery due to potential risks.
Diuretics: Administer diuretics like Lasix 120 mg IV, particularly if there is a risk of fluid overload, especially after blood transfusion.
Post-Delivery Transfusion: After delivery, if transfusion is still required, packed red blood cells should be transfused, often with Lasix to prevent fluid overload.
Positioning and Nursing Care: Nurse the patient in a propped-up position in bed to aid breathing and provide comprehensive nursing care addressing all needs.
Mouth Care: Pay special attention to mouth care, as stomatitis (inflammation of the mouth) and glossitis (inflammation of the tongue) are common in severely anaemic patients.
High-Protein and Nutritious Diet: Provide a diet high in protein, including green leafy vegetables and fresh fruits, to support red blood cell production and overall recovery.
Fluid Balance Chart: Maintain a strict fluid balance chart to monitor fluid intake and output, and closely observe for signs of impending cardiac failure, such as increasing pulse rate and respiratory rate.
Breathlessness Monitoring: Closely monitor and report any breathlessness, especially in patients with underlying conditions like tuberculosis, as it could indicate worsening respiratory distress.
IV Inferon Administration Note: When using IV Inferon, it’s typically prepared by mixing 5 ampoules of 250 mg each (total 1250 mg) in 500 ml of dextrose 5% or normal saline and infused slowly.
Management During Labor:
1st Stage of Labor:
Comfortable Positioning: Ensure the mother is positioned comfortably in bed to facilitate breathing and comfort.
Light Analgesia: Consider providing light pain relief as needed to reduce stress and discomfort.
Oxygenation: Administer oxygen via mask or nasal cannula to increase maternal blood oxygen saturation and prevent fetal hypoxia, especially during contractions.
Strict Asepsis: Maintain strict aseptic techniques throughout labour and delivery to minimize the risk of infection.
2nd Stage of Labor: This stage usually proceeds without specific interventions directly related to anaemia, assuming maternal and fetal condition remains stable.
3rd Stage of Labor:
Active Management of 3rd Stage: Focus on active management of the third stage of labour to minimize blood loss. This includes early cord clamping and controlled cord traction to deliver the placenta efficiently and reduce postpartum haemorrhage risk.
Methergin or Oxytocin Administration: Immediately after delivery of the baby, administer a uterotonic medication such as 0.2 mg of Methergin (methylergometrine) or 20 units of oxytocin in 500 ml of Ringer’s Lactate intravenously, followed by 10 units of oxytocin intramuscularly. These medications help the uterus contract firmly, reducing postpartum bleeding.
Intensive Observation: Closely monitor the mother for signs of postpartum haemorrhage and other complications in the immediate postpartum period.
Blood Replacement: Be prepared to replace any significant blood loss promptly with fresh packed red blood cells if postpartum haemorrhage occurs.
Avoid Overloading: While replacing blood, be cautious not to over-transfuse or overload the patient with excessive fluids, particularly if there is underlying cardiac compromise. Replace blood loss appropriately but avoid fluid overload.
Puerperium (Postpartum Period):
Bed Rest: Encourage adequate bed rest in the postpartum period to allow the mother to recover and rebuild strength.
Infection Monitoring and Treatment: Closely monitor for any signs of postpartum infection and promptly treat any infections that develop to prevent further complications and delayed recovery.
Continuation of Iron Therapy: Continue iron supplementation as prescribed until haemoglobin levels return to within the normal range to replenish iron stores depleted during pregnancy and delivery.
Dietary Guidance: Reinforce the importance of maintaining a healthy, iron-rich diet postpartum to aid recovery and support lactation.
Counselling and Support: Provide counselling and practical support to the mother and family regarding newborn care, infant feeding, and managing household chores while the mother recovers, ensuring adequate rest and nutrition.
Prevention of anaemia:
Prevention is crucial in reducing the incidence and impact of anaemia during pregnancy. Effective preventive strategies include:
Good Antenatal Care: Regular and early antenatal care is vital to screen for and detect anaemia and malaria early in pregnancy. Early detection allows for timely intervention and treatment, preventing progression to severe anaemia.
Health Education: Provide comprehensive health education to pregnant women and communities about the importance of a balanced diet rich in iron, good personal hygiene practices, and environmental sanitation, including the proper use of latrines to prevent parasitic infections like hookworm.
Malaria Protection: In malaria-endemic regions, encourage and ensure the use of malaria preventive measures, such as insecticide-treated bed nets (ITNs) and intermittent preventive treatment in pregnancy (IPTp) with sulfadoxine-pyrimethamine (SP), to reduce malaria-related anaemia.
Blood Loss Reduction: Implement best practices in obstetric care during all stages of labour and delivery to minimize blood loss, particularly during the third stage of labour through active management.
Protein Replacement during Lactation: Advise mothers to consume adequate protein in their diet during lactation to support red blood cell production and overall recovery postpartum.
Folic Acid Supplementation: Provide routine folic acid supplementation, especially preconception and in early pregnancy, to prevent neural tube defects and also to contribute to healthy red blood cell production.
Routine Blood Examinations: Include routine haemoglobin testing as part of antenatal care to monitor haemoglobin levels regularly throughout pregnancy, allowing for early detection and management of anaemia.
Avoidance of Frequent Childbirths: Advise on family planning methods to encourage adequate spacing between pregnancies. Allowing sufficient time between pregnancies enables the mother’s body to recover iron stores and reduce the risk of depletion with subsequent pregnancies.
Dietary Advice: Provide specific dietary advice to pregnant women, emphasizing the importance of consuming iron-rich foods. Recommend incorporating foods like red meat, poultry, fish, beans, lentils, and dark green leafy vegetables into their daily diet.
Supplementary Iron Therapy: Prescribe iron supplements as needed based on individual risk factors, dietary intake, and haemoglobin levels. Routine iron supplementation is often recommended during pregnancy to meet increased iron demands.
Treatment of Underlying Illnesses: Promptly diagnose and effectively treat any underlying medical conditions that can contribute to anaemia, such as chronic infections, parasitic infestations (like hookworm), or chronic diseases. Early diagnosis and treatment are crucial for preventing and managing anaemia effectively.
Advice to the Mother:
Early Reporting of Pregnancy: Advise the mother to seek antenatal care as soon as she suspects or confirms pregnancy. Early antenatal visits enable timely initiation of prophylactic iron therapy and other preventive measures.
Explanation of Anaemia: Clearly explain to the mother what anaemia is, its causes in pregnancy, the potential dangers to herself and her baby, and how anaemia can be prevented and managed.
Importance of Rest: Advise the mother to prioritize rest and avoid overexertion to reduce fatigue and strain on her body, especially if she is anaemic.
Dietary Counseling: Thoroughly discuss dietary modifications. Provide detailed advice on the types of iron-rich foods to include in her daily diet and how to prepare them to maximize iron absorption.
Medication Adherence: Emphasize the importance of taking any prescribed iron or other medications regularly and as directed. Explain the benefits and potential consequences of non-adherence.
Mosquito Bite Prevention: Stress the need to prevent mosquito bites to avoid malaria, especially in malaria-prone regions. Advise on using bed nets, mosquito repellents, and appropriate clothing.
Family Planning Advice: Discuss family planning options to promote birth spacing and allow her body to recover and replenish iron stores between pregnancies.
Hospital Delivery Recommendation: Recommend and encourage delivery in a hospital or well-equipped health facility where skilled birth attendants and emergency obstetric care are available to manage any complications, including postpartum haemorrhage, effectively.
Complications of Anaemia in Pregnancy
Anaemia during pregnancy can lead to a range of complications affecting both the mother and the fetus.
Maternal Complications
Increased risk of Postpartum Haemorrhage (PPH): Anaemia impairs blood clotting, significantly increasing the risk of excessive bleeding after delivery.
Increased Risk of Infection: Weakened immune system due to anaemia makes mothers more susceptible to infections during and after pregnancy.
Increased Risk of Heart Failure: The strain on the heart to compensate for reduced oxygen levels can lead to heart failure, particularly in severe anaemia.
Fatigue and Weakness: Persistent and debilitating fatigue and weakness significantly impact the mother’s quality of life and ability to care for herself and her baby.
Shortness of Breath: Chronic breathlessness reduces activity tolerance and overall well-being.
Increased Risk of Preeclampsia: Some studies suggest a link between anaemia and an increased risk of developing preeclampsia, a serious pregnancy complication characterized by high blood pressure and protein in urine.
Increased Risk of Delayed Wound Healing: Anaemia can impair tissue repair and wound healing, potentially leading to delayed healing of episiotomy or caesarean section wounds.
Increased Risk of Death: In severe, untreated anaemia, particularly in low-resource settings, there is an increased risk of maternal mortality.
Fetal Complications
Premature Birth: Anaemia increases the risk of preterm delivery, resulting in babies being born too early and facing complications associated with prematurity.
Low Birth Weight: Fetal growth can be restricted due to inadequate oxygen and nutrient supply, leading to babies being born with low birth weight, increasing their vulnerability to health problems.
Fetal Growth Restriction: Anaemia can result in intra-uterine growth restriction (IUGR), where the fetus does not grow to its full potential size in the womb.
Stillbirth: Severe anaemia and placental insufficiency are associated with an increased risk of stillbirth (fetal death in late pregnancy).
Cerebral Palsy: Some studies have linked severe maternal anaemia to a slightly increased risk of cerebral palsy in offspring, possibly due to impaired fetal brain development.
Congenital Anomalies: While less direct, severe nutritional deficiencies contributing to anaemia might increase the risk of certain congenital anomalies.
Cognitive Impairment: Iron deficiency anaemia in pregnancy has been linked to potential long-term cognitive and developmental delays in children.
Delayed Development: Babies born to anaemic mothers may experience delayed developmental milestones in early childhood.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

