Communicable Diseases
Ebola Virus Disease
Table of Contents

Learning Objectives
- Understand the basic characteristics, classification, and outbreak history of the Ebola virus.
- Identify the primary modes of Ebola virus transmission, including from wildlife to humans and between humans.
- Recognize when an individual with Ebola becomes infectious and which bodily fluids pose the highest risk.
- Describe the process for diagnosing Ebola, including the importance of patient history and available laboratory tests.
- Outline the key strategies for controlling Ebola outbreaks, focusing on community engagement and preventative measures.
- Explain methods to reduce Ebola transmission in community, healthcare, and post-recovery settings.
EBOLA VIRUS DISEASE
- Also known as Ebola Hemorrhagic fever.
Introduction
- Ebolavirus disease is caused by the Ebolavirus (EBV).
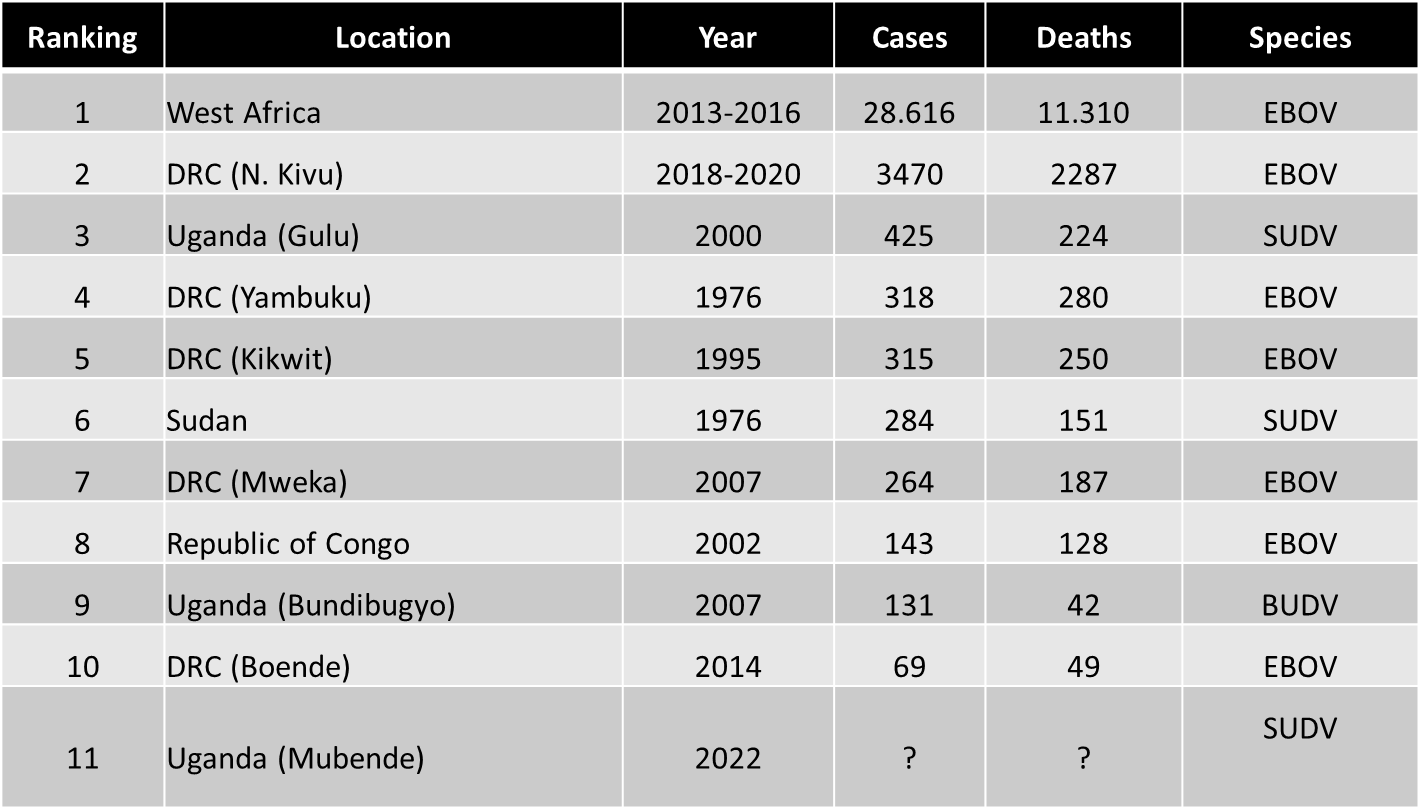
- First identified in 1976.
- It has since caused multiple outbreaks in DRC and.
- Neighboring countries like Uganda.
- The largest outbreak so far has been in west Africa.
- Lasting 2yrs with over 29000 cases.
Classification
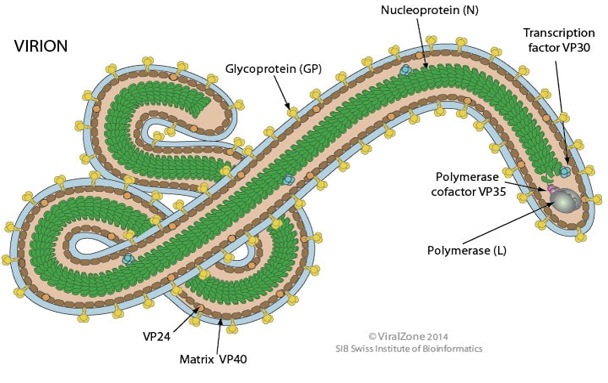
- EBV is a negative sense single stranded RNA virus.
- Resembling measles, mumps (paramyxoviruses) and Rhabdoviruses like rabies.
- It’s a member of Filoviridae family, from Latin word filum (thread like) base on its filamentous structure.
- Filoviridae family consist of 3 genera, Ebolavirus, Marburgvirus, & cuevavirus.
- Ebolavirus consists of six species: Zaire, Sudan, Bundibugyo, Tai forest, Reston and Bombali. First 4 cause human disease.
Structure of the Ebola Virus
Outbreak history
- Zaire identified in 1976, caused multiple outbreaks including the largest in 2014 west Africa, case fatality ~40 – 90%.
- Sudan identified in 1976, in 4 outbreaks in Uganda(2000) and Sudan(2x1970s &2004) case fatality averaged at 50%.
- Ivory coast virus (Tai forest) has caused on non fatal case, Bombali and Reston are not known to cause human disease.
- Bundibugyo emerged in Uganda 2007 case fatality 30%, DRC 2012.
- Hemorrhagic fever is no longer used to refer to EVD because only a small %age develop hemorrhage and usually in terminal phase.
- Sudan species:
- Two outbreaks in sudan in the 1970s.
- Gulu Uganda, 2000, 425 cases and 224 deaths. Case fatality as at 53%.
- Kibaale , Uganda 2012, 24 cases identified with 17 deaths.
- Luwero 2011, one case 12 year old from zirobwe, died following admission in GMH.
Transmission of Ebola virus
- Secondary human-to-human transmission occurs through direct contact with the blood, secretions, organs or other bodily fluids of infected persons.
- High transmission risk when providing direct patient care or handling dead bodies (funerals).
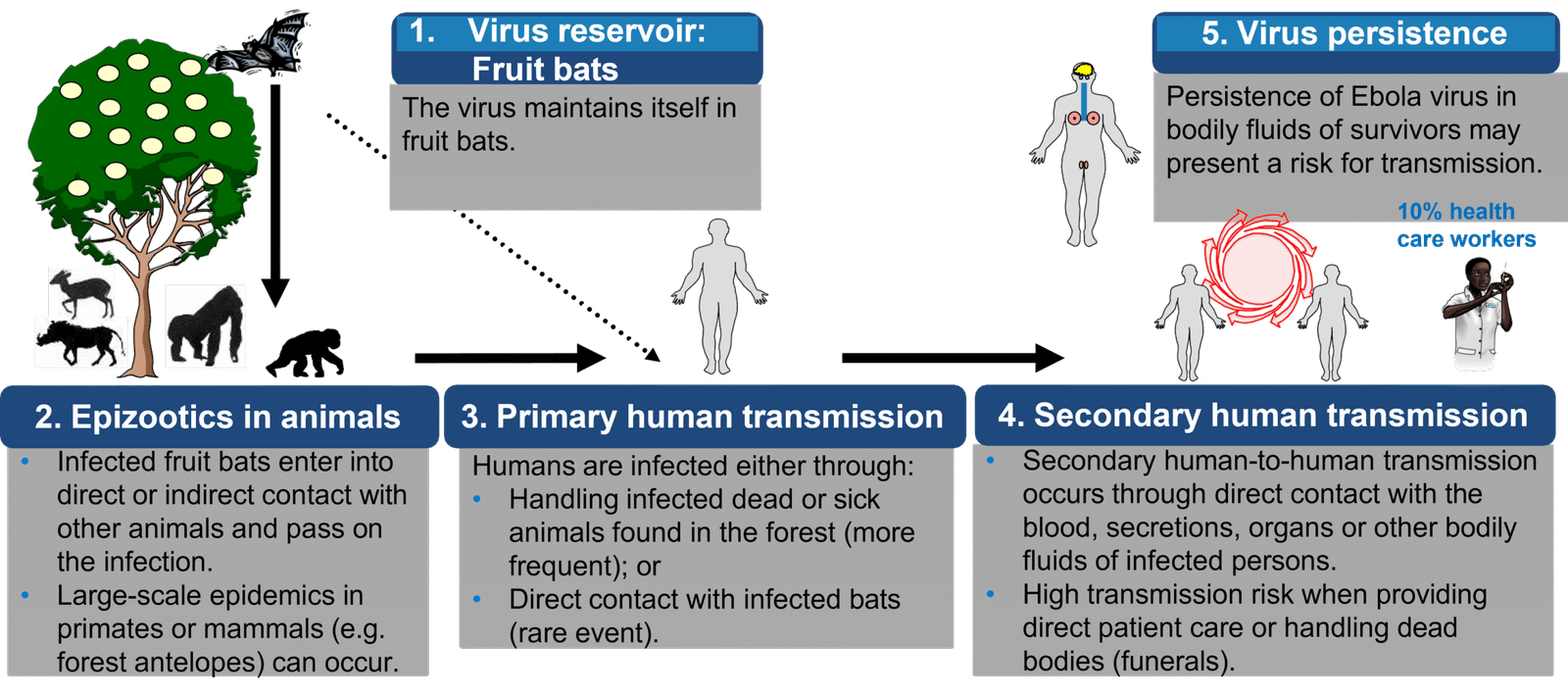
How is EBOD transmitted? (1)
- The virus spreads from person to person through:
- – Direct contact (through broken skin or mucous membranes) with the blood, secretions, organs or other bodily fluids of infected people. Among infected bodily fluids, the most infectious are blood, faeces and vomit.
- – Contact with surfaces and materials (e.g. bedding, clothing) contaminated with these fluids.
- Transmission can occur through needlestick injuries when managing a sick.
How is EBOD transmitted? (2)
EBOD is not spread through casual contact (see previous slide).
The risk of infection with Ebola virus is minimal if you have not been in close contact with the bodily fluids of someone sick with or deceased from EBOD.
How is EBOD transmitted? (3)
People are not infectious until they develop symptoms.
- The virus multiplies within the body before symptoms develop.
- Individuals become contagious when symptoms appear.
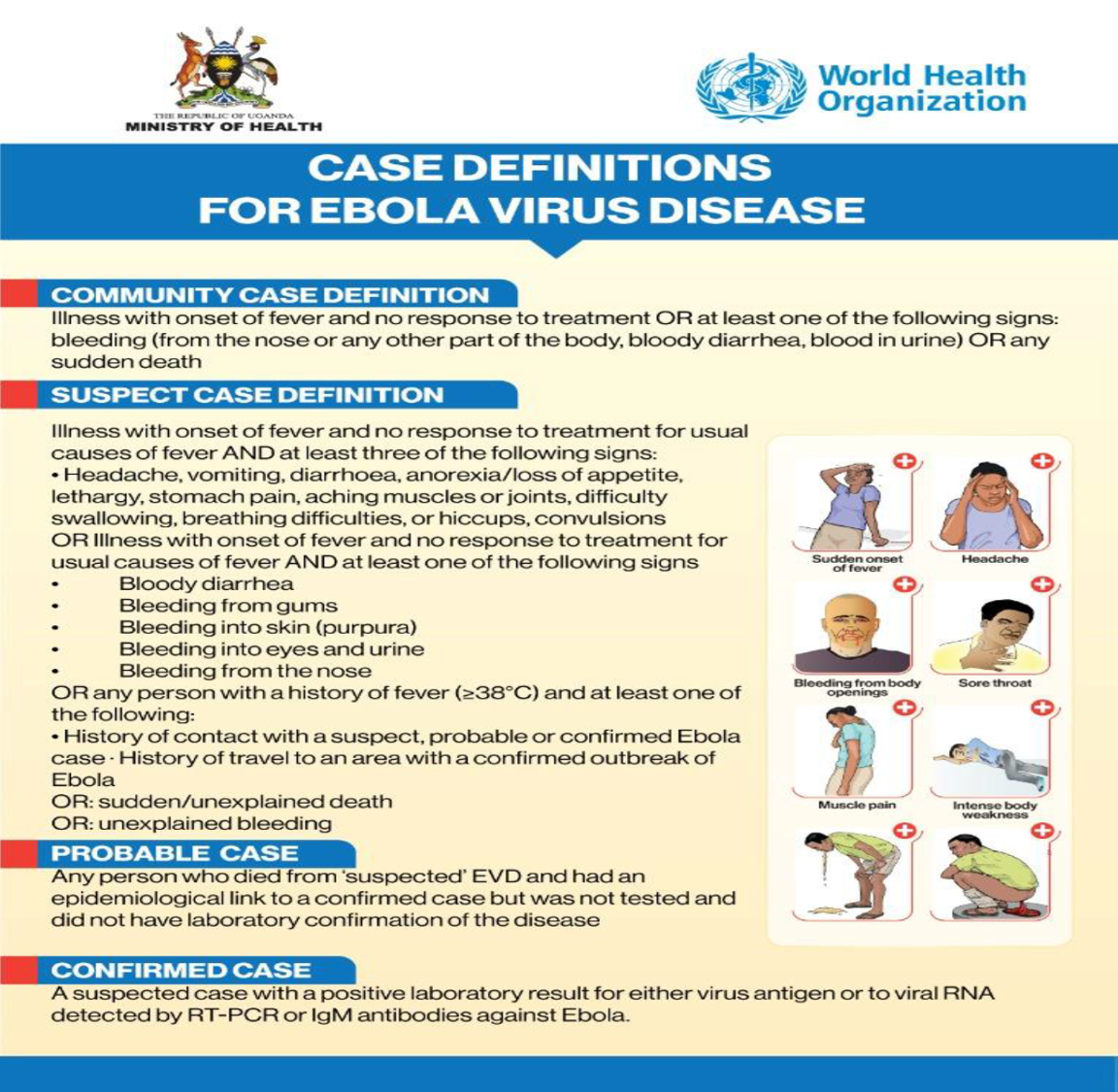
Ebola disease diagnosis
- Symptoms are non-specific; clinical diagnosis may be difficult.
- Differential diagnosis includes other viral haemorrhagic fevers, yellow fever, malaria, typhoid fever, shigellosis, and other viral and bacterial diseases.
- Patient history is essential and should include:
- – Contact with a dead or sick animal.
- – Contact with a suspected, probable or confirmed Ebola patient.

Ebola disease laboratory diagnosis
Tests for Ebola:
- – RT-PCR for definitive diagnosis in acute disease.
- – IgG and IgM ELISA for retrospective diagnosis in recovering patients.
- – Rapid antigen detection tests: screening tests for acute disease (requires confirmation).
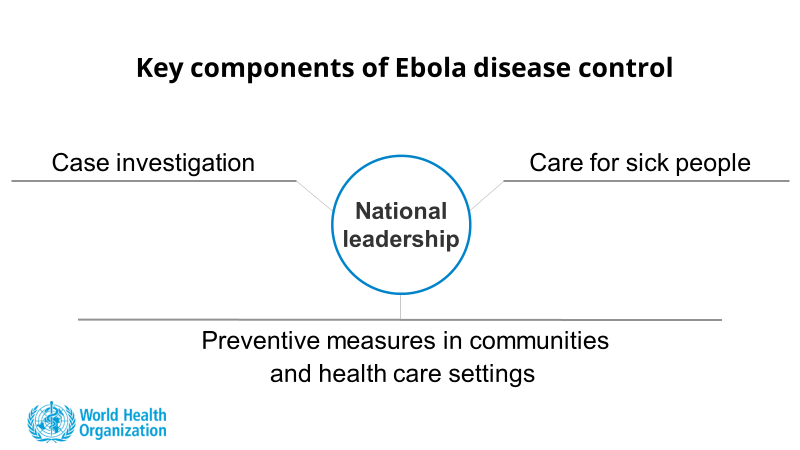
General strategy to control EBOD outbreaks
[Emergent pathogens, international surveillance and international health regulations (2005)]. Formenty P, Roth C, Gonzalez-Martin F, Grein T, Ryan M, Drury P, Kindhauser MK, Rodier G.
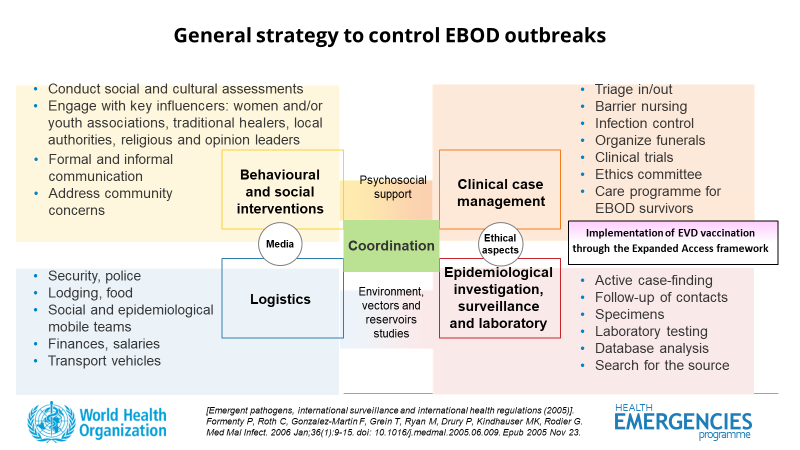
Community engagement and awareness
- Engage with communities to promote desired health practices and behaviours, particularly on caring for sick and/or deceased persons.
- Provide accurate and timely health advice and information about the disease.
Reducing wildlife-to-human transmission
- Reducing the risk of wildlife-to-human transmission from contact with infected fruit bats or monkeys/apes and the consumption of their raw meat.
- – Animals should be handled with gloves and other appropriate protective clothing.
- – Animal products (blood and meat) should be thoroughly cooked before consumption.
Reducing human-to-human transmission
- Reducing the risk of human-to-human transmission from direct or close contact with people with Ebola symptoms, particularly with their bodily fluids.
- – Gloves and appropriate personal protective equipment should be worn when taking care of ill patients at home.
- – Regular handwashing is required after visiting patients in a hospital, as well as after taking care of patients at home.
- – Organize safe and dignified burials for people who may have died of Ebola disease.

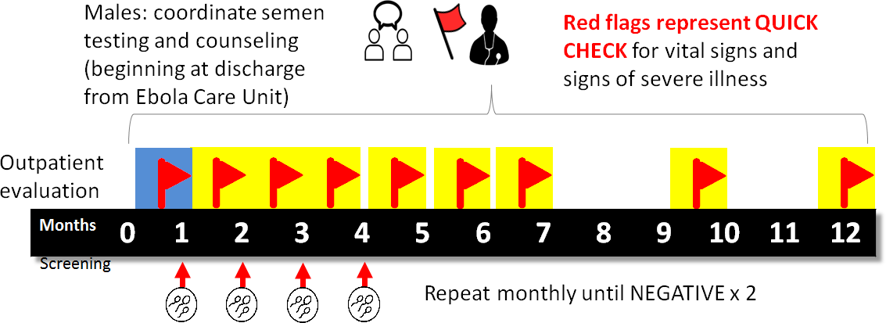
Reducing possible sexual transmission
- Reducing the risk of possible sexual transmission: WHO recommends that male survivors of Ebola disease practice safer sex and hygiene for 12 months from onset of symptoms (if no semen testing can be done) or until their semen tests negative twice for Ebola virus starting 1 month after recovery.
Controlling infection in health care settings
- Implement standard precautions with all patients – regardless of their diagnosis – in all work practices at all times, including safe injection practices.
- Health care workers treating patients with Ebola disease should apply extra infection control measures to prevent contact with the patients’ blood and bodily fluids and contaminated surfaces or materials, such as clothing and bedding.
- Laboratory workers are also at risk. Samples taken from suspected Ebola disease cases for diagnosis should be handled by trained staff and processed in suitably equipped laboratories.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowGet in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co