Communicable Diseases
Elephantiasis (Bancroftian Filariasis)
Table of Contents

Learning Objectives
- Understand the causes and transmission of lymphatic filariasis, also known as Elephantiasis.
- Describe the pathology and clinical phases of lymphatic filariasis, from asymptomatic microfilaremia to chronic lymphedema.
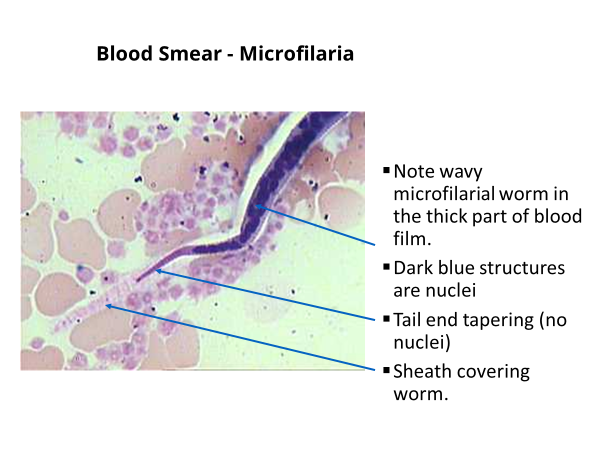
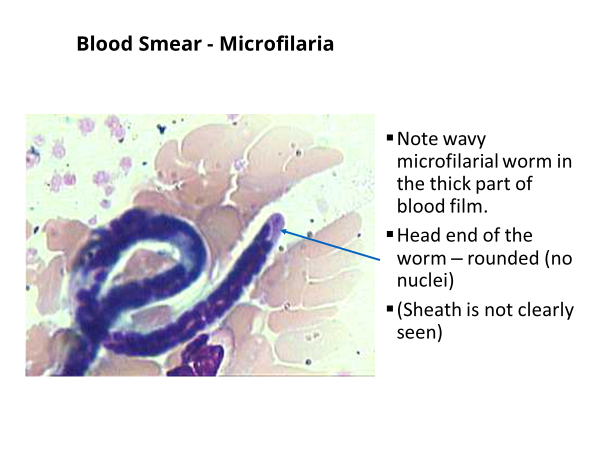
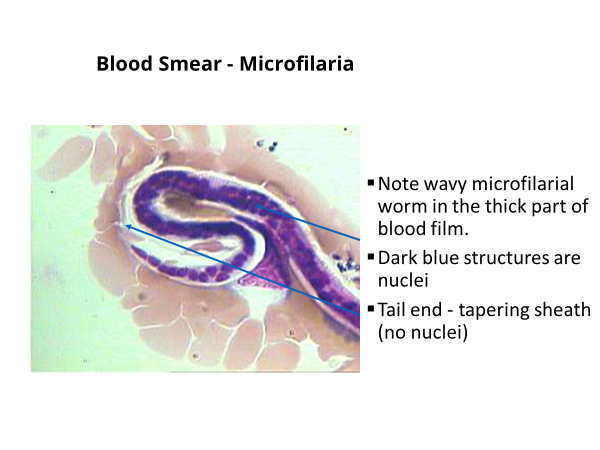
- Identify the diagnostic methods for Elephantiasis, focusing on the detection of microfilariae in blood smears.
- Outline the main chemotherapeutic agents used in filariasis treatment and their modes of action.
- Explain the management strategies for acute adenolymphangitis (ADL) and chronic lymphedema, including non-pharmacological approaches.
- Summarize the key components of lymphatic filariasis control programs, including vector control and morbidity management.
ELEPHANTIASIS
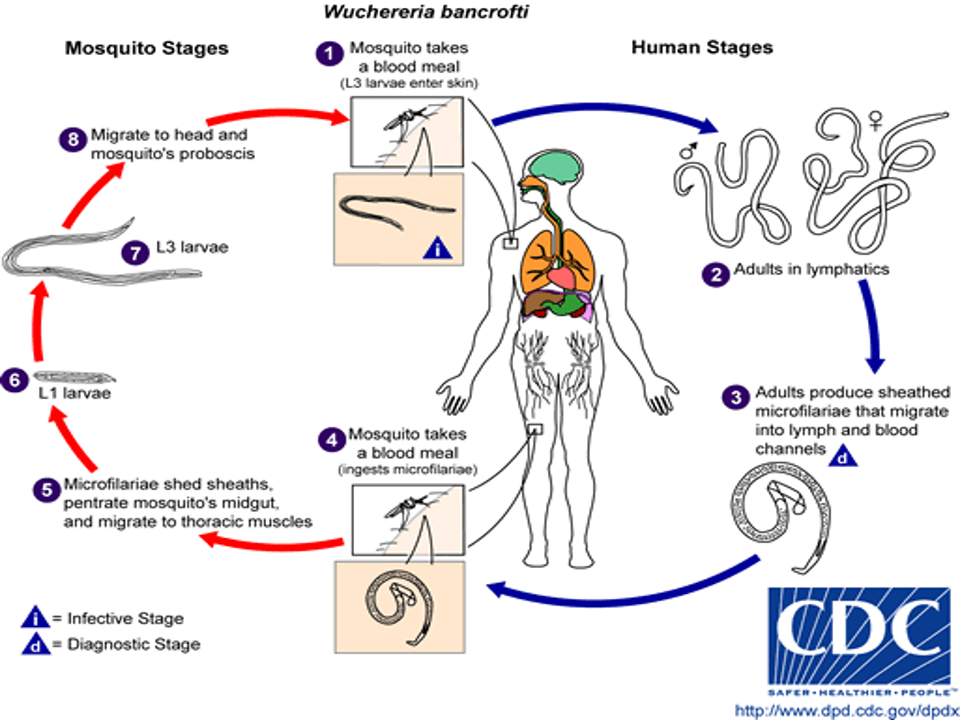
- Wuchereria bancrofti and Brugia malayi are filarial nematodes
- Spread by several species of night – feeding mosquitoes
- Causes lymphatic filariasis, also known as Elephantiasis
- Commonly and incorrectly referred to as “Elephantitis”
- Humans are the definitive host for the worms that cause lymphatic filariasis
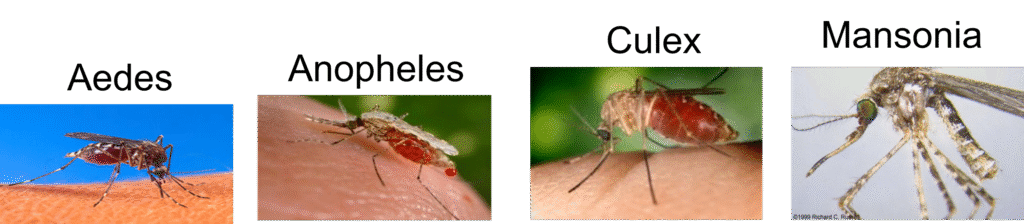
- Transmitted by Culex, Aedes, and Anopheles species
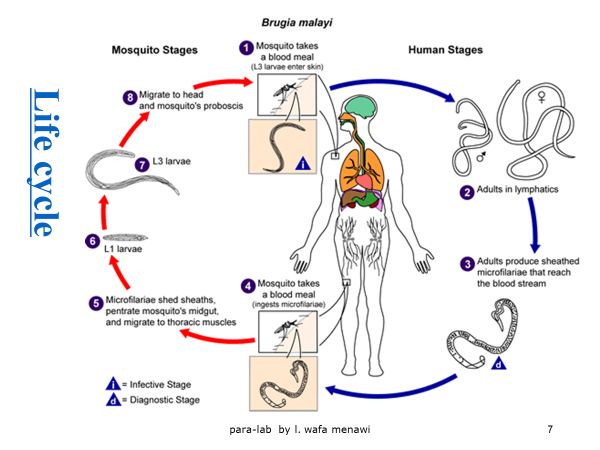
- B.malayi is transmitted by Anopheles and Mansonia species.
- Host: Mosqutoes (intermediate host)
- Human (final host)
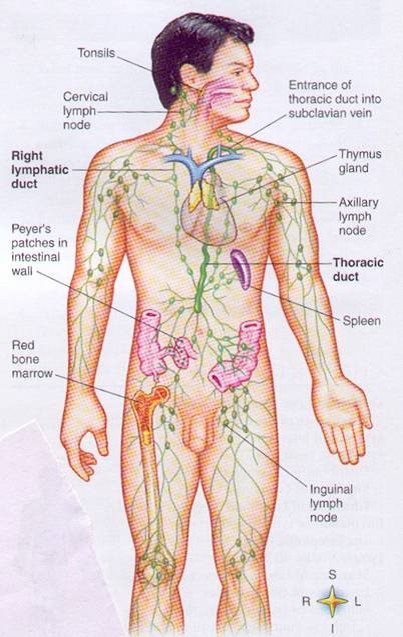
- Location: Lymphatics and lymph nodes
- Infective stage: Infective larvae
- Transmission stage: Microfilariae
- Diagnostic stage: Microfilariae
Life cycle
Wuchereria Life Cycle
Pathology of Lymphatic Filariasis
- The pathology associated with lymphatic filariasis results from a complex interplay of the pathogenic potential of the parasite, the tissue response of the host and external bacterial and fungal infections. Most of the pathology associated with LF is limited to the lymphatics.
- mediated both by an immune response to the adult worms as well as by a direct action of the parasite or the product released by them. In the absence of inflammation, marked lymphatic dilation with lymphoedema is seen in experimental animals with immune deficiency and when immuno competent cells are induced,itresults inflammatory granuloma reactions around the parasite and subsequent obstructions of the lymphatic vessel occurs leading to lymphoedema.
Clinical pictures
- Initially asymptomatic
- Symptoms develop with increasing numbers of worms
- Less than 1/3 of infected individuals have acute symptoms
- Clinical Course is 3 phases:
- Asymptomatic Microfilaremia
- Acute Adenolymphangitis (ADL)
- Chronic/Irreversible lymphedema
- Superimposed upon repeated episodes of ADL
Acute Adenolymphangitis
- Presents with sudden onset of fever and painful lymphadenopathy
- Retrograde Lymphangitis
- Inflammation spreads distally away from lymph node group
- Immune mediated response to dying worms
- Most common areas: Inguinal nodes and Lower extremities
- Inflammation spontaneously resolve after 4-7 days but can recur frequently
- Recurrences usually 1-4 times/year with increasing severity of lymphedema
- Secondary bacterial infections in edematous(elephantatic) areas
- Filarial fever (fever w/o lymphangitis)
- Tropical Pulmonary Eosinophilia
- Hyperresponsiveness to microfilariae trapped in lungs
- Nocturnal Wheezing
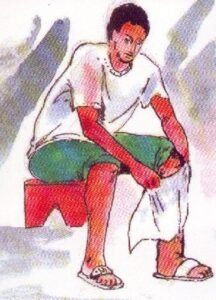
Chronic Manifestations
- Lymphedema
- Mostly LE and inguinal, but can affect UE and breast
- Initially pitting edema, with gradual hardening of tissues → hyperpigmentation & hyperkeratosis
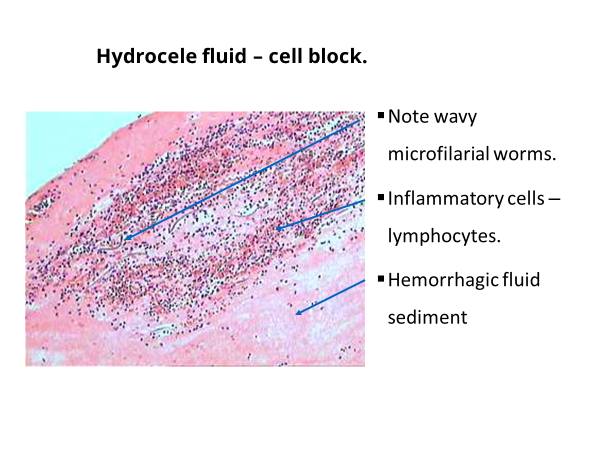
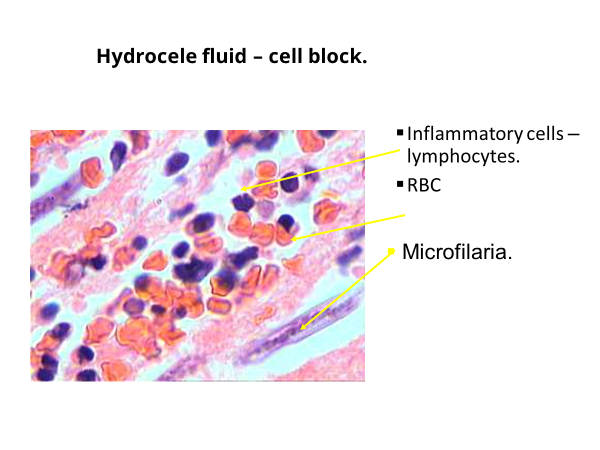
- Genitalia→Hydroceles
- Renal involvement
- Chyluria→lymph discharge into urine
- Loss of fat and protein→ hypoproteinemia & anemia
- Hematuria, proteinuria from ?immune complex nephritis
- Secondary bacterial/fungal infections
Diagnosis
- Elephantiasis: accumulation of lymph in extremeties, fibrosis, and thickening of skin.

Microfilariae are seen in blood smears and are DIAGNOSTIC

Blood Smear – Microfilaria
Management of Lymphatic Filariasis
- Treating the infection
- Treatment and prevention of Acute ADL attacks
- Treatment and prevention of Lymphoedema
- Treating the infection
- Remarkable advances in the treatment of LF have recently been achieved focusing not on individual but on community with infection, with the goal of reducing mf in the community, to levels below which successful transmission will not occur.
Chemotherapy of Filariasis
Drugs effective against filarial parasites
- Diethyl Carbomazine citrate (DEC)
- Ivermectin
- Albendazole
- Couramin compound
Treatment of microfilaraemic patients may prevent chronic obstructive disease and may be repeated every 6 months till mf and/or symptoms disappears.
Diethyl Carbomazine Citrate
(Hetrazan, Banocide, Notezine)
- Mode of action: DEC do not have direct action of parasite but mediate through host immune system.
- Very effective against mf (Microfilariacidal)
- Lowers mf level even in single dose
- Effective against adult worms in 50% of patients in sensitive cases.
- Dose: 6mg/Kg/12 days
- Recent dosage: 6mg/Kg single dose
- Adverse reactions are mostly due to the rapid destruction of mf which is characterised by fever, nausea, myalgia, sore throat, cough, headache.
- No effect on the treatment of ADL
- Drug of choice in the treatment of TPE ().therapeutic plasma exchange
Ivermectin
- Mode of action: Directly acts on mf and no action on adults.
- Very effective against mf (Microfilariacidal)
- Lowers mf level even in single dose of 200µg – 400µg/Kg body weight
- No action on TPE
- Drug of choice in Co-endemic areas of Onchocerciasis with LF.
- Adverse reactions are lesser but similar to that of DEC
- Microfilariae reappears faster than DEC
Albendazole
- This antihelmenthic kills adult worms
- No action on microfilariae
- Dose: 400mg/twice day /2 weeks
- With combination of DEC & Ivermectin, it enhances the action of the drugs.
- It induces severe adverse reactions in hydrocele cases due to the death of adult worms.
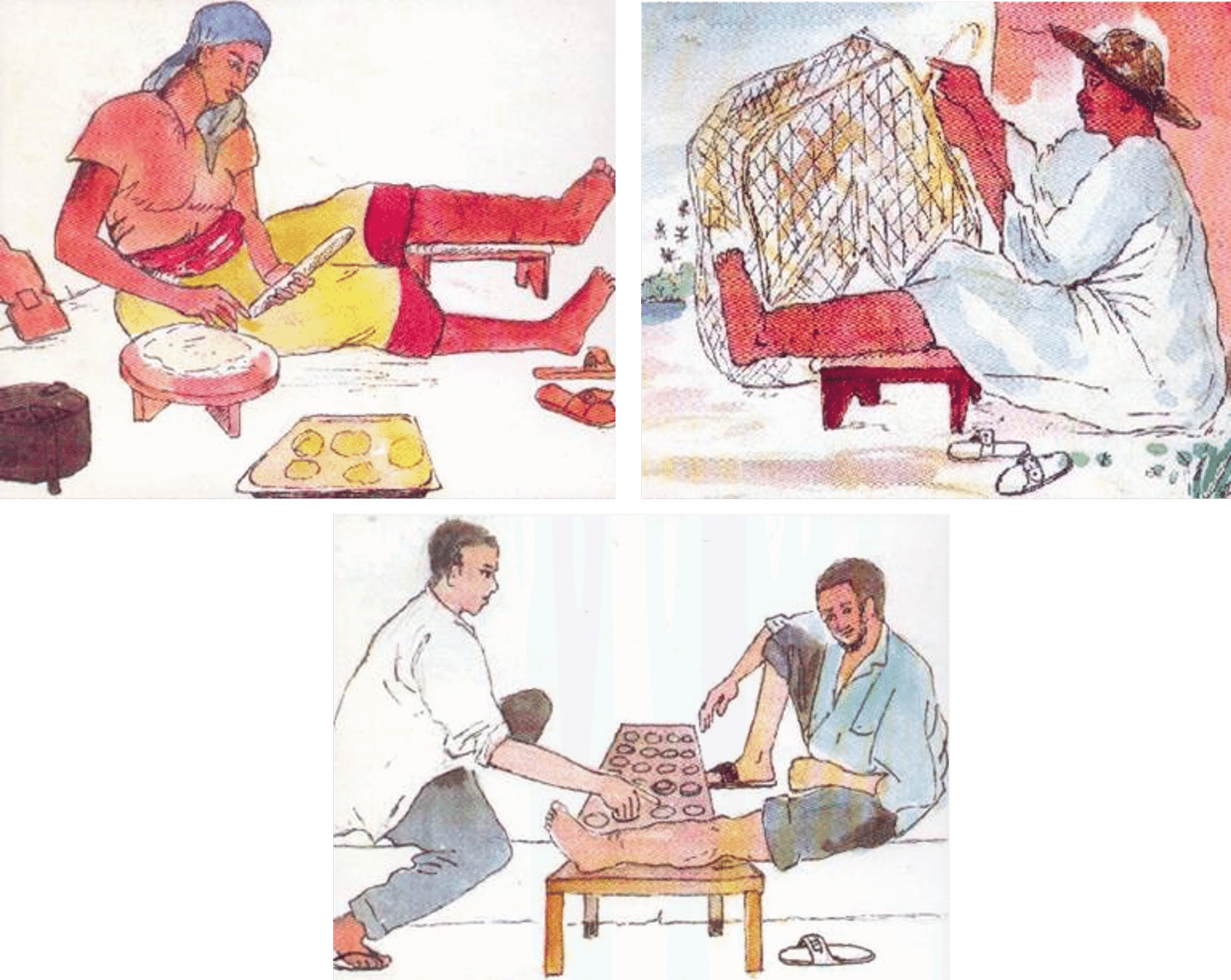
Treatment and Prevention of ADL
The most distressing aspect of LF is the acute attacks of ADL, which results in considerable economic loss and deterioration of quality of life. Prompt treatment and prevention of ADL are of paramount importance. ADL may be seen both in early & late stages of the disease. It is due to the infection & inflammation of the skin and affected area due to entry of bacteria or fungus through the entry lesions. The skin becomes warm, tender, painful, swollen, red. Patient develops fever, headache, chills and sometimes nausea and vomiting. Occasionally becomes septicemic.

- First sign will be enlarged, tender and painful L.nodes. SS of inflammation appears later lasting for 4-5days. Peeling & darkening of skin is common. Repeated attacks increase the size of the legs. Management includes symptomatic treatment like relieving pain, care of entry lesions etc. In patients with late stages of oedema, long term antibiotic therapy using oral Penicillin or long acting parentral Benzathil Penicillin are used to prevent ADL.
ADL

Cooling the Leg
Entry Lesions
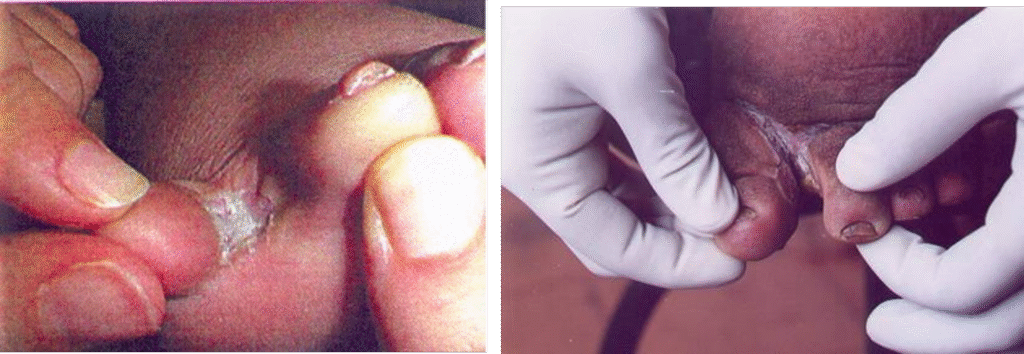
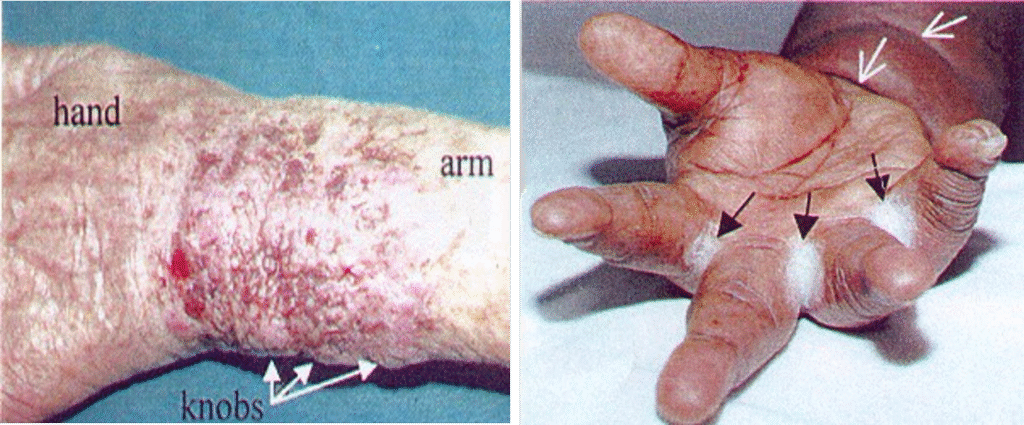
Ulcers

Surgical Treatment
- Hydrocele: Excision
- Scrotal Elip: Surgical removal of Skin & Tissue, preserving penis and testicles.
- Lymphoedema (Elephantiasis): Excision of redundant tissue, Excision of subcutaneous and fatty tissues,
- postral drainage and physiotherapy
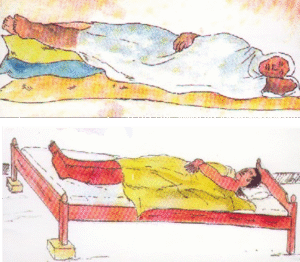
Treatment and Prevention of Lymphoedema and Elephantiasis
Early treatment with drugs may destroy the adult worms and logically prevent the later development of lymphoedema. Once lymphoedema is established there is no cure and the “foot care programme” may offer relief and prevent acute attacks thus preventing further progression of the swelling.
Lymphoedema management helps
- to eliminate the bad odour
- to prevent & heal entry lesion
- to help patients self-confident
- to reduce the size of the lyphoedema
- to prevent disability
- to prevent economic loss
Lymphoedema Management Basic Components and Benefit
Basic Components
- Hygiene
- Prevention & cure of entry lesions
- Exercise
- Elevation of foot
- Use of proper footwares
Hygiene
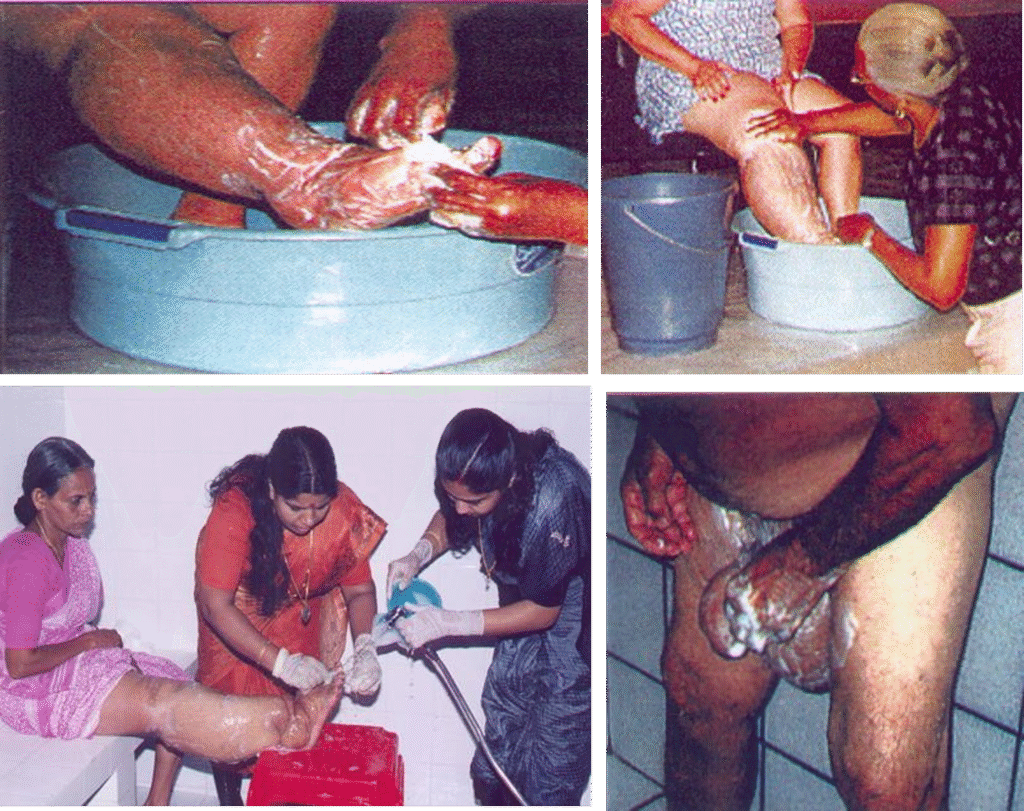
Drying the Leg
Prevention & Cure of Entry lesions
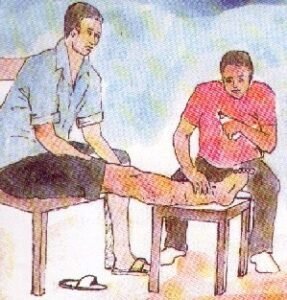
Exercise
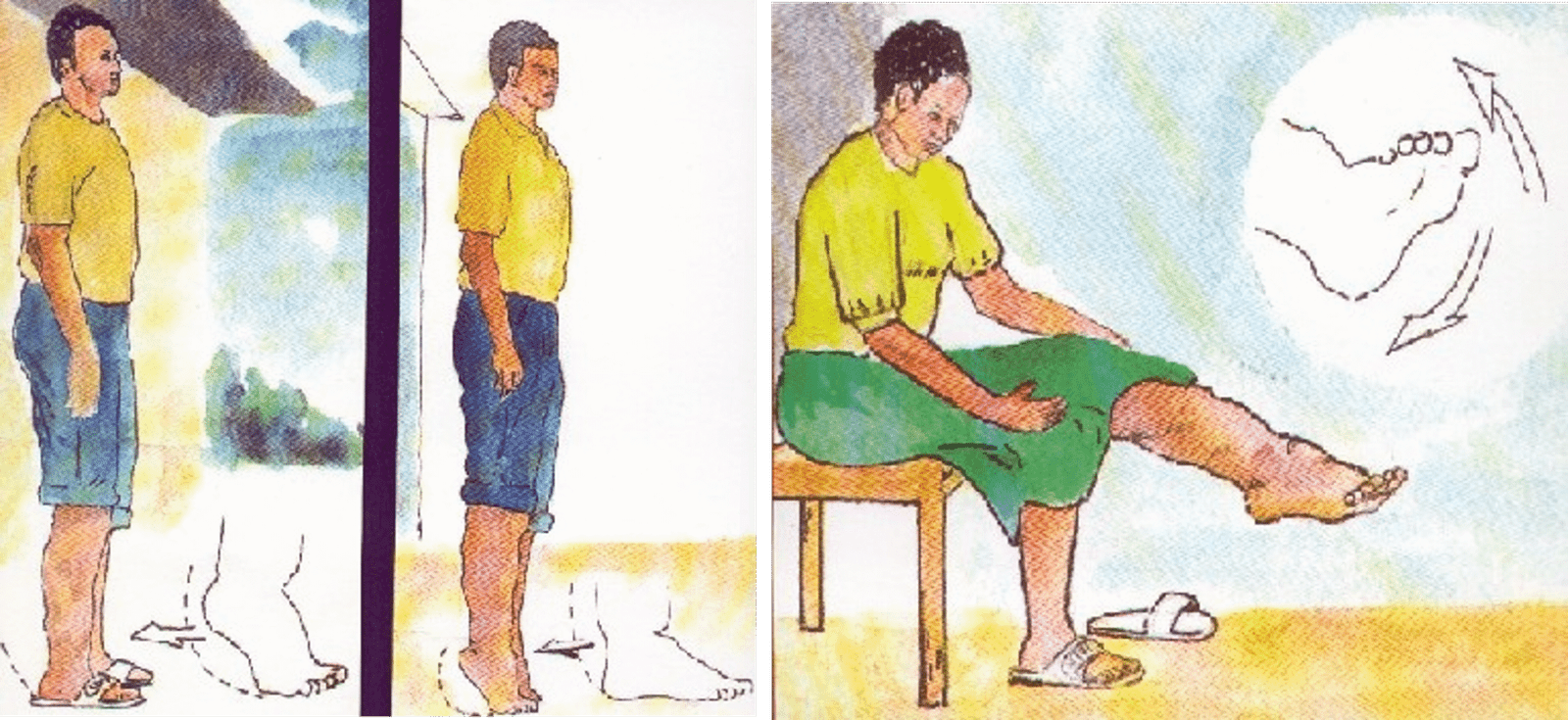
Elevation of Foot
Use of appropriate Foot ware

Lymphatic Filariasis Control Programme
The current strategy of filariasis control (Elimination) is based on:
- Interruption of transmission
- Control of Morbidity
Interruption of the transmission can be achieved through: a. Chemotherapy b. Vector control
An integrated programme is in place for the control of lymphatic filariasis. Earlier, vector control was the main method of control.
There are three main reasons why filariasis never causes explosive epidemics
- The microfilariae does not multiply in the vector
- Infective larvae do not multiply in man
- Life cycle of the parasite is relatively long (>15 )
- Case detection and treatment in low endemic areas are suitable for preventing transmission and controlling the disease.
- In high endemic areas, Mass chemotherapy is the approach.
- DEC medicated salt is also a form of Mass treatment using low dose of drug over a long period of time (1-2 gm /Kg of Salt).
Vector Control
Vector control involves anti larval measures, anti adult measures, personal prophylaxis. An integrated method using all the vector control measures alone will bring about sustained vector control.
I. Anti larval measures:
- Chemical control a. Mosquito larvicidal oil b. Pyrosene oil c. Organo phosphorous compounds such as Temephos, Fenthion,
- Removal of pistia plants
- Minor environmental measures
Vector Control
II. Anti adult measures:
Anti adult measures as indoor residual spay using DDT, HCH and Dieldrin. Pyrethrum as a space spray is also followed.
III. Personal Prophylaxis:
Reduction of man mosquito contact by using mosquito nets, screening of houses, etc.
Morbidity Management
- Control Morbidity (relief of suffering)
- Community-level care of those with disease
- Lymphoedema
- Acute inflammatory attacks
- Hydrocele repair
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowGet in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

