Communicable Diseases
MEASLES
Table of Contents

Learning Objectives
- Describe the etiology, transmission, signs, and symptoms of Measles, including the pathognomic Koplik’s spots.
- Explain the nursing management and supportive care for a patient with Measles, covering aims such as infection control, temperature control, and nutritional support.
- Identify the common complications of Measles affecting various body systems like the respiratory, central nervous, and gastrointestinal systems.
- Differentiate between Measles and Rubella (German Measles) based on their symptoms, complications, and impact, particularly the risks of Congenital Rubella Syndrome.
- Understand the cause, transmission, and clinical manifestations of Onchocerciasis (river blindness), including its effects on the skin and eyes.
- Outline the diagnosis, treatment, and prevention strategies for Onchocerciasis, such as the use of Ivermectin and the destruction of the black fly vector.
MEASLES
Definition
- Is a highly contagious, acute viral infection characterized by a generalized skin rash with a pathognomic koplick’s spots.
- It is a persistent cause of childhood morbidity and mortality in developing countries i.e. one of the childhood killer diseases.
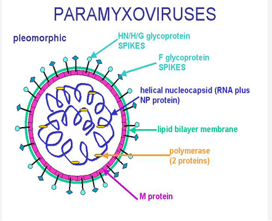
AETIOLOGY
- It is caused by a measles virus belonging to the genous morbilli virus of paramyxo viruses’ family.
- These viruses are multi-shaped, spherical structures, having a diameter of 100 to 250 nm and consisting of six proteins. The inner capsid is composed of a wheel helix of RNA and an outer envelope.
TRANSMISSION
- Air borne, inhaling droplets, coughed by an infected person.
- Ingestion (oral faecal).
- Direct contact with infected stool.
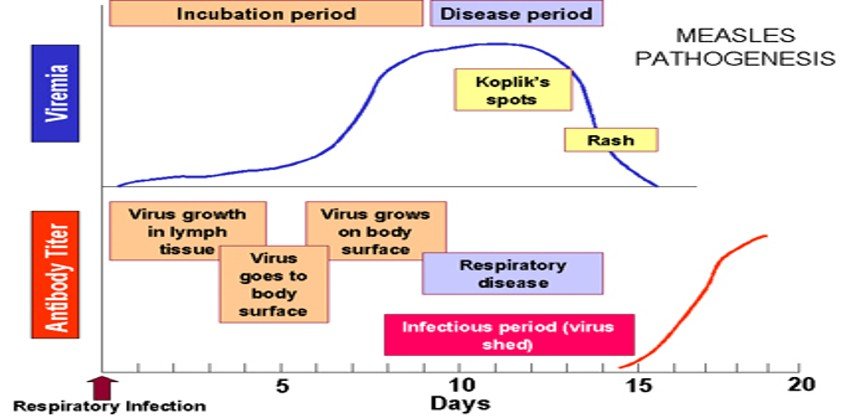
- Patients are contagious 1 to 2 days before the onset of symptoms until 4 days after the appearance of the rash. Infectivity peaks during the prodromal phase.
PREDISPOSING FACTORS
- Unprotected communities with low immunization coverage.
- Malnourished children.
- Overcrowding and poor ventilation.
- Children with previous severe infections e.g. TB.
INCUBATION PERIOD
- 10 to 14 days.
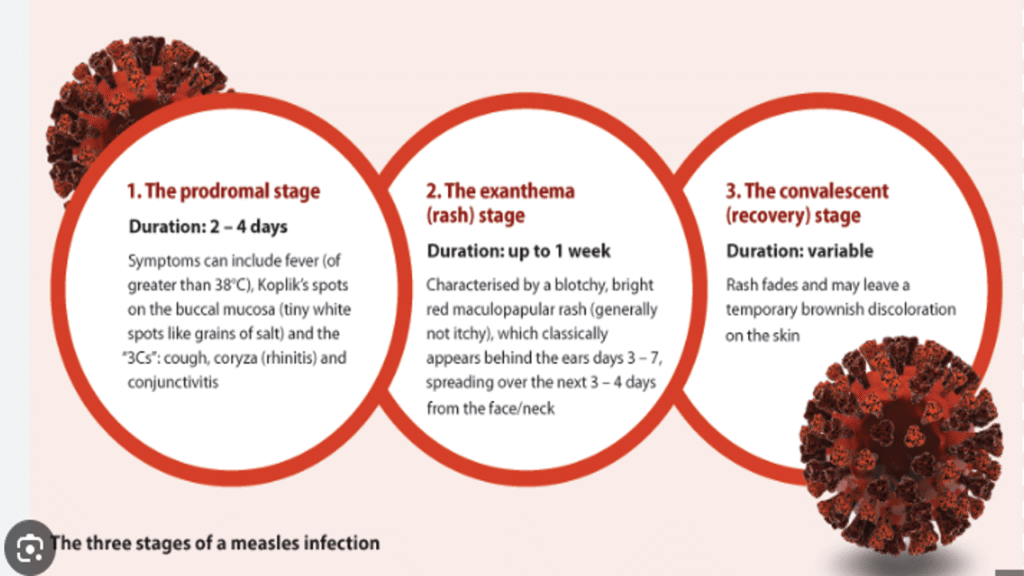
Stages
- Prodromal stage.
- Eruptive stage.
- Post-measles stage.
Agent
- Agent- RNA virus ( Paramyxo virus family, genus Morbillivirus ).
- Source of infection-cases of measles, but not carriers.
- No animal reservoir.
- Infective material- Nasal secretion ,Respiratory tract &Throat.
- Communicability- Highly infectious during prodromal period and at the time of eruption.
- Secondary attack rate- > 80%.
Host factors
- Measles is a human disease.
- There is no known animal reservoir, and an asymptomatic carrier state has not been documented.
- ❑ Age- 6 months to 3 years even up to 10 years.
- ❑ Incidence equal in both sexes.
- ❑ Immunity – life long immunity.
- ❑ Malnourished children are susceptible.
Measles Pathogenesis
- Respiratory transmission of virus.
- Replication in nasopharynx and regional lymph nodes.
- Primary viremia 2-3 days after exposure.
- Secondary viremia 5-7 days after exposure with spread to tissues.
Courtesy : Adapted from Mims et al. Medical Microbiology, 1993, Mosby.
Virulence factors
1. Portal of entry:
- Respiratory mucus membrane.
- It first infects the respiratory mucosa, spreads through the lymphatics and bloodstream, and can then infect the conjunctiva, respiratory tract, urinary tract, GI tract, endothelial cells, and the central nervous system.
2. Attachment:
- Hemagglutinin.
- Hemagglutinin in an integral membrane protein found on the surface of the measles virus.
- Hemagglutinin binds to CD46, a glycoprotein found on the surface of most cells.
- (CD46 protects host cells from autoimmune destruction by binding to C3b and C4b and cleaving them).
3. Evade the immune system:
- Immunosuppression:
- The measles virus blocks Tcell proliferation response to IL-2.
- The measle’s Hemagglutinin protein and fusion proteins bind to lymphocytes and interrupt IL-2 cell signaling.
4. Destruction of tissue:
- a serious febrile illness. The maculopapular rash, which starts at the hairline and spreads over the whole body, is caused by immune T-cells targeted to the infected endothelial cells of the small blood vessels. T-cell deficient individuals do not have the rash, but do have uncontrolled disease which usually results in death.
- The damage, as well as the control of the disease, is most probably caused by the immune system.
Maculopapular rash
- Maculopapular describes a rash that contains both macules and papules. A macule is a flat discolored area of the skin, and a papule is a small raised bump. A maculopapular rash is usually a large area that is red, and has small, confluent bumps.

SIGNS AND SYMPTOMS
❖Measles begins with a 2 to 4 day complain of coughing/ barking cough, conjunctivitis with lacrimation, nasal discharge and increasing fever as high as 40.60c (sign of secondary viraemia). This stage may be confused with influenza.
❖Just before the onset of a rash, koplick’s spots appear as a 1 to 2 mm (blue-white spots on the bright red background) on the inside of the chick muscles, (buccal mucosa). They disappear after the onset of rash. This is a pathognomic sign found only in measles.
❖The rashes that are flat, red, irregular soon develop and become raised up in 3 to 5 days after the onset of the beginning symptoms, it also affects the GIT and respiratory tract as well; and these last for 4 to 7 days before they disappear. The mucus membrane of the mouth cavity is inflamed and become reddened.
❖The rash begins from behind the ears, spreads down to the trunk, including the limbs (soles and palms). At this point, the patient is the most severe stage with the disease.
❖Skin desquamation may occur.
❖Fever may reduce between the 4th to 5th day after rash onset.
❖Other associated symptoms are; Lymphadenopathy, diarrhea, vomiting and splenomegaly.
Signs and symptoms cont’d Generalized rash lasting minimum three days Fever.
Signs and symptoms cont’d Red eyes Red lips and sores in the mouth.
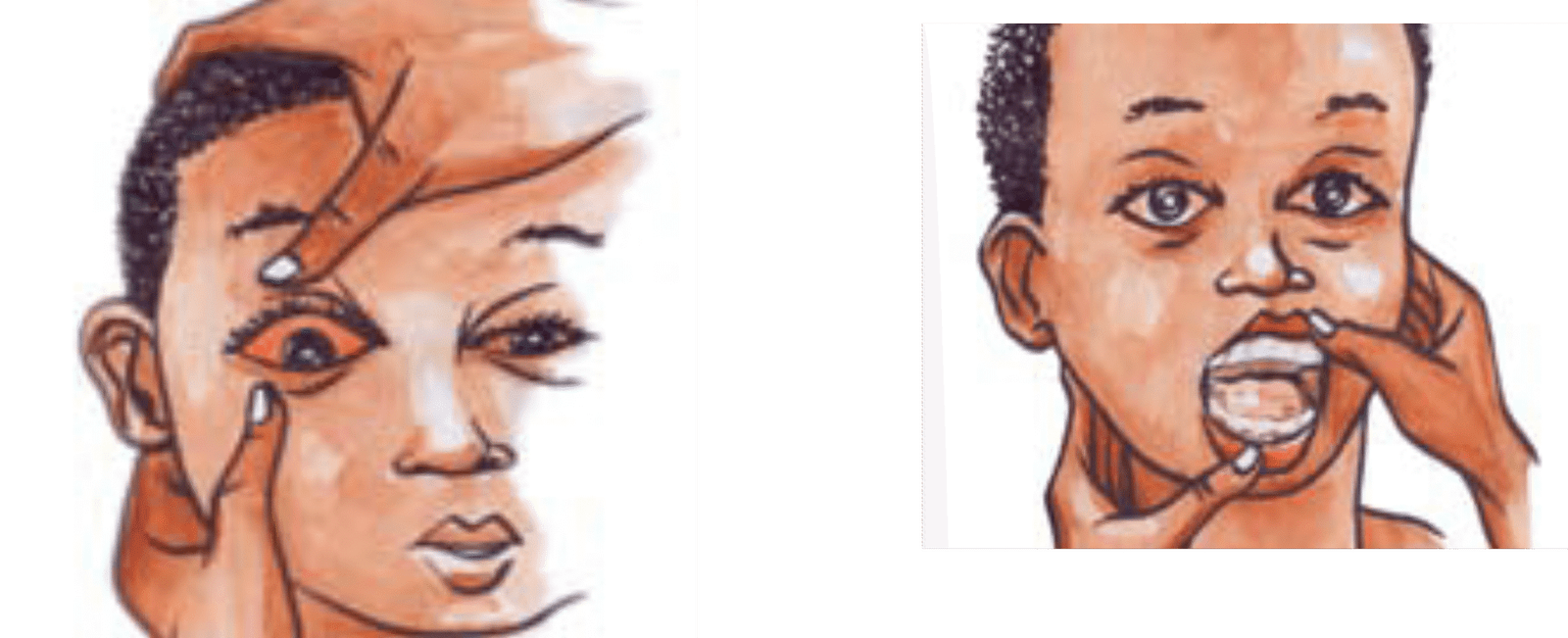
Signs and symptoms cont’d Dry cough Running nose.
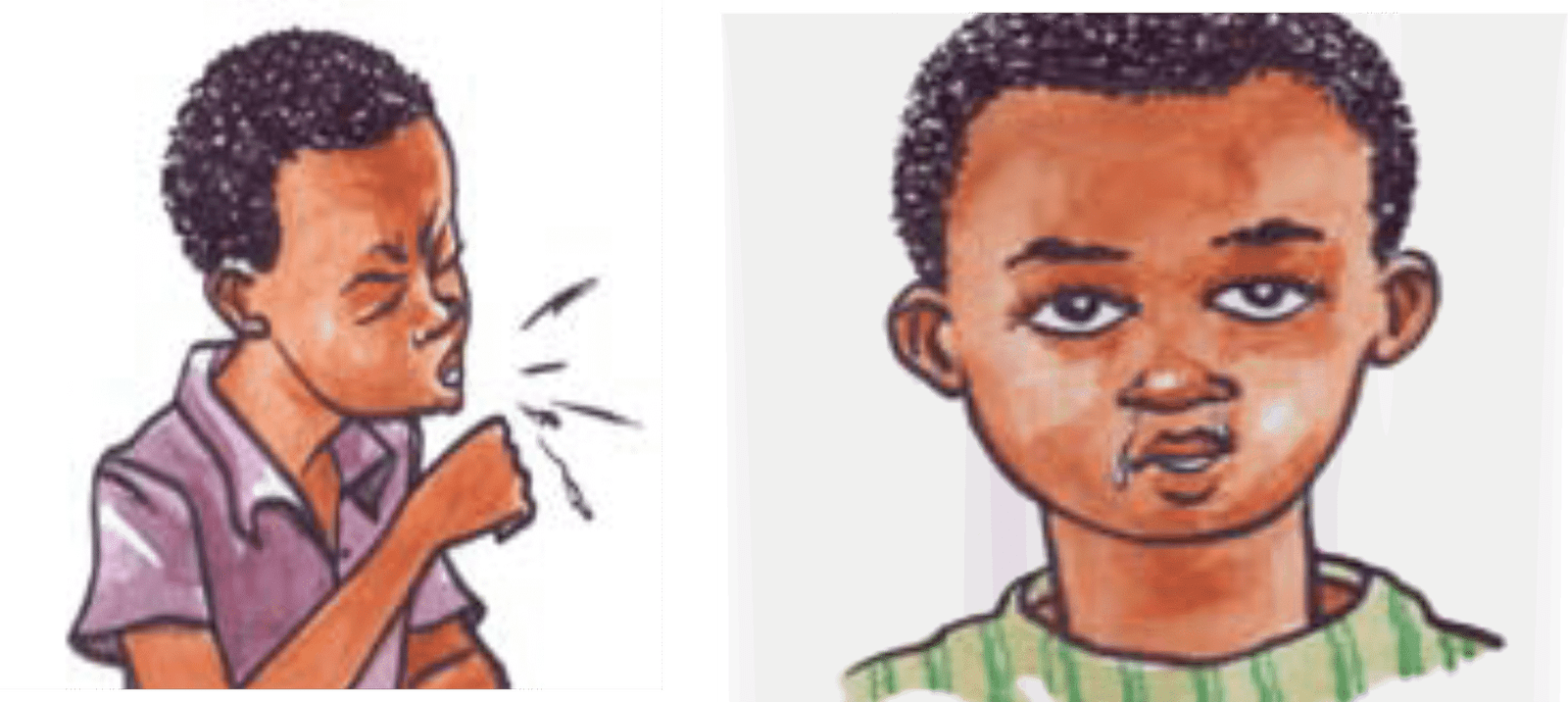
DIFFERENTIAL DIAGNOSIS
- Rubella.
- Other viral disease causing skin rash.
DIAGNOSIS
- Koplick’s spots (diagnostic).
- Investigate complications.
MANAGEMENT (supportive and symptomatic based)
Aims
➢To prevent the spread of the disease.
➢To provide respiratory comfort and rest.
➢To control the temperature.
➢To rehydrate the patient.
➢To raise the nutritional status of the patient.
Special management
▪ Admission; In children’s ward in an isolation room.
▪ Infection control techniques;
▪ Isolation of the patient to prevent further spread.
▪ Isolation door labeling “infectious” to prevent others from coming into the room.
▪ Proper hand washing. ▪ Care of infectious linens i.e. disinfect before taking to laundry.
Patient’s comfort at prodromal state;
▪ Encourage rest to conserve energy for the body to use in fighting infection and in between coughs.
▪Give plenty of fluids/ breast feed to soothe the throat and to liquefy secretions.
▪ Administer cough linctus (syrups 5mls 3 to 4 times a day) to suppress the cough.
▪Offer pain relievers to the child. ▪ Relieve any nasal congestion or discharge.
Temperature control
▪ The patient is tepid sponged with Luke warm water to reduce the temperature.
▪Good room ventilation is ensured to offer fresh air and to dilute the viral load in the room.
▪ Application of cold compresses.
▪ Plenty of cold fluids orally or per NG tube or I.V depending on the patient’s condition to reduce the fever.
▪ Constant changing of bed linen for patient’s comfort and avoid over heating the patient.
Mouth mucous membrane;
▪ Inspect the mouth 3 times a day for inflammation, or bleeding and record the observations and report to the doctor your findings.
▪ Provide mouth care with a mild mouth wash like sodium bicarbonate, normal saline-warm or chlorhexidine every 4 hourly or after each feeds.
▪Use cotton swabs for cleaning the mouth cavity and gum.
▪ Let the mother not to give hot, spicy or rough foods to the child.
▪Give patient vitamin A 200,000iu i.e. first dose at diagnosis, second dose the next day and the third dose, 2 to 4 weeks later for healing purposes and epithelial tissue repair.
Eyes;
- Hygiene of the eyes should be maintained followed by application of tetracycline eye ointment 1% B.D for 5 days.
Diarrhoea and vomiting; (dehydration)/ feeding
▪Give the patient enough oral fluids (tea, liquid porridge, milk, etc) orally or per NG tube (ORS) to replace the lost fluids.
▪ Administer IV fluids (dextrose 5%, normal saline, ringers lactate) to replace the lost fluids.
▪Give patient plenty of juice to encourage appetite and provide vitamin C for healing purposes.
▪ Let the child have balanced diet full of protein (soup or tissue if able to eat) for healing purposes and tissue repair.
▪ Encourage carbohydrates for energy.
Skin care;
▪ Daily bathing 2 or 3times a day to clean the skin, to prevent infection of the rashes.
▪ Care of the mouth and eyes.
Prophylactic antibiotics;
- to prevent complications.
- Penicillins are given for otitis media or pneumonia e.g. benzyl penicillin 50,000iu per kg plus CAF 25mg /kg IM/ IV as prescribed or CAF ear/ eye drops 0.5% 2 to 4 drops (for children), or Amoxyl or Bactrium.
SUMMARY OF NURSING CARE
- Outpatient (mild type)
- Tell parent to barrier nurse the child.
- Bring to clinic if condition worsens.
- Give frequent small fluids and plenty of drinks.
- Severe form (or child malnourished)
- The child is admitted in isolation for barrier nursing due to low immunity, mask worn, hand washing, disinfection of contaminated articles.
- Observations; Temperature 4 hourly, give paracetamol, tepid sponge.
- Febrile convulsions; give anti- malarials as per the hospital policy.
- Turn convulsing patient to the side to protect air way.
- Never give anything to eat or drink.
- Clear air way; If convulsing, give diazepam 2mg for less than 1 year, 5 mg up to 3 years rectally or IV slowly or Phenobarbital 10 to 15 mg /kg IM.
COMPLICATIONS
- RESPIRATORY SYSTEM
- Laryngitis
- Croup
- Bronchitis
- Pneumonia
- Bronchiectasis
- CNS
- Encephalitis
- Mental retardation
- Epilepsy
- GIT
- Gastro-enteritis
- Hepatitis
- Messenteric adenitis
- Appendicitis
- Illeo-colitis
- EENT
- Otitis media
- Corneal ulceration
- OTHERS/ RARE
- Myocarditis
- Glomerulonephritis
- Exacerbate TB due to low immunity.
COMMON COMPLICATIONS OF MEASLES
❑ Laryngo-tracheo bronchitis.
❑ Pneumonia.
❑ Otitis media.
❑ Febrile convulsions.
❑ Conjunctivitis, corneal ulcers, cloudy cornea, dry eye (xerophthalmia).
❑ Malnutrition.
❑ Diarrhoea.
❑ Stomatitis (sore mouth).
RUBELLA/ GERMAN MEASLES
Definition
oThis is a mild viral disease resembling measles, characterized by mild fever, appearance of rash on the 3rd day, lymphadenopathy. oIt used to be the disease of the “whites” and it is a disease of pregnant women on the first trimester. It is an acute viral infection of children and adults with the greatest presentation as subclinical. oIn adults, it causes arthritis, in pregnancy, causes a group of malformation referred to as congenital rubella syndrome in a high proportion of infected fetuses.
AETIOLOGY
- It is caused by Rubella virus which is an RNA stranded virus, closely related to the alpha viruses. This virus does not need a vector for transmission. It is composed of an RNA and protein inner helical capsid surrounded by a lipid containing envelope with a diameter of roughly 60nm.
TRANSMISSION
- Airborne.
- Transplacentally.
INCUBATION PERIOD
- 12-23 days with an average of 18 days.
PATHOGENESIS AND PATHOLOGY
oThe virus which is spread in droplets shed in the respiratory secretions, which infects the respiratory tract and the blood stream. oInfants with rubella may excrete the virus from the airway and urine until 2 years. After an attack, specific antibiotics and cell-mediated immunity develop for future protections. oThe rash is immunologically cell-mediated and its onset coincides with development of specific antibodies. oThe proposal fetal damage caused by the virus includes; cataracts, deafness, mutism, tissue necrosis without inflammation, chromosomal damage, fetal growth retardation, cardiac abnormalities.
SIGNS AND SYMPTOMS
- 1 to 5 days of low graded fever.
- Flu-like illnesses followed by malaise and conjunctivitis.
- Post auricular, occipital or posterior cervical lymphadenopathy spotted rashes appear after 5-10 days. When total blood count is done, leucopenia and thrombocytopenia is revealed.
SIGNS AND SYMPTOMS IN CHILDREN. CONGENITAL RUBELLA SYNDROME
- Deafness and complications later, since its transmitted from mother to child trans-placentally.
- Cataracts, micropthalmia (tiny eye) congenital glaucoma following a corneal ulceration, microcephaly (very small heads), mutism, cardiac abnormalities, meningo-encephalitis, hepatosplenomegaly with jaundice.
TREATMENT: SYMPTOMATIC
- There is no treatment available or necessary for patients suffering from Rubella. The specific defense mechanism and humoral immunity takes place.
- Pregnant mothers should be kept away from known cases of Rubella.
PREVENTION
- Administration of live attenuated Rubella vaccine.
- Not necessary except for pregnant mothers.
- Only young girls can be exposed to infection so that an active natural immunity is obtained for fetal protection.
CONTROL
- Passive immunization with human gamma globulin vaccine is done.
COMPLICATIONS IN UNBORN CHILDREN
- Eye; Microphthalmia and cataracts.
- Ears; Partial/ complete deafness.
- Heart; Patent ductus arteriosus, arterial or ventricular septal defects.
- CNS; Microcephaly and mental retardation. Others; Hepato spleenomegally, thrombocytopenia, intra-uterine fetal death, spontaneous abortion.
ONCHOCERCIASIS
- Onchocerciasis also known as river blindness,
- is a disease caused by infection with the parasitic worm -Onchocerca volvulus.
- It is the second most common cause of blindness due to infection, after trachoma.
Transmission
- The parasite worm is spread by the bites of a black fly (Simulium fly). These flies live near rivers therefore the name of the disease.
Signs and symptoms
- Skin
- Intense itching o Swelling
- Acute papular onchodermatitis – scattered pruritic papules
- Depigmentation – ‘leopard skin’ appearance, usually on anterior lower leg
- Scaly, wrinkled skin (Lizard’s skin)
- Hanging groin
- Skin nodules
- Lymphadenopathy.
- Ocular involvement
- Provides the common name associated with onchocerciasis, river blindness.
- Sclerosing Keratitis.
- Iridocyclitis.
- Corneal opacities.
- Others
- Onchocerciasis has been associated with an unusual form of epilepsy and Nodding Disease Syndrome.
- Growth retardation.
- Elephantiasis of scrotum.
Life cycle
➢A Simulium female black fly takes a blood meal on an infected human host, and ingests microfilaria.
➢The microfilaria enters the gut and thoracic flight muscles of the black fly, progressing into the first larval stage.
➢The larvae mature into the second larval stage, and move to the proboscis and into the saliva in its third larval stage. Maturation takes about seven days.
➢The black fly takes another blood meal, passing the larvae into the next human host’s blood.
➢The larvae migrate to the subcutaneous tissue and undergo two more molts. They form nodules as they mature into adult worms over six to 12 months.
➢After maturing, adult male worms mate with female worms in the subcutaneous tissue to produce between 700 and 1,500 microfilariae per day.
➢The microfilaria migrates to the skin during the day, and the black flies only feed in the day, so the parasite is in a position for the female fly to ingest it. Black flies take blood meals to ingest these microfilariae to restart the cycle.
Diagnosis
- From history and examination.
- Skin snip (biopsy).
- Blood for microfilaria, microscopy.
- Immune diagnosis- it looks at hypersensitivities.
- Excision of nodules for adult worms.
Treatment
- Ivermectin (Mectizan); infected people can be treated with two doses of ivermectin 150mcg/kg, six months apart, repeated every three years.
- Antibiotics: doxycycline is used to kill the Wolbachia bacteria that live in adult worms.
Prevention and control
- Ivermectin treatment of affected people.
- Prophylaxis treatment with Evermectin in endemic areas (mass treatment).
- Destruction of simulium flies with insecticides or river dosing.
- Health education about settlement along rivers.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowGet in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

