Pediatric Conditions of the Respiratory System
Subtopic:
Asthma in Children

Asthma is a long-term condition affecting the airways of the lungs. It’s characterized by inflammation that can be reversed, and it leads to a narrowing of the airways, making it difficult to breathe.
This inflammation is responsible for the recurring and recognizable signs of asthma, such as wheezing (a whistling sound often heard when breathing out), shortness of breath, a feeling of tightness in the chest, and coughing. These episodes typically improve with medications that help to open up the airways (bronchodilators).
Various substances involved in the body’s inflammatory response play a role in asthma, including mast cells, eosinophils, T-lymphocytes, macrophages, neutrophils, and epithelial cells.
While the exact cause of asthma is not fully understood, it’s believed to involve a combination of genetic predisposition and environmental triggers.
Classification of Asthma
Asthma can be broadly categorized into:
(a) Intrinsic asthma: This type is diagnosed when a specific external factor causing the asthma cannot be identified.
(b) Extrinsic asthma: This type, also sometimes called allergic asthma, is characterized by a clear external trigger, such as allergens like pollen or dust mites.
Levels of Asthma
These categories, established by the National Institutes of Health, help doctors and pediatricians assess the severity of a child’s asthma.
Intermittent asthma
Asthma is classified as intermittent if, without any ongoing controller medication, the following characteristics are observed:
Symptoms (such as difficulty breathing, wheezing, chest tightness, and coughing):
Occur on fewer than two days per week.
Do not significantly hinder normal daily activities.
Nighttime symptoms:
Occur on fewer than two nights per month.
Mild persistent asthma
Asthma is considered mild persistent if, without regular controller medication, the following are present:
Symptoms:
Occur more than two days a week but are not present every day.
The presence of symptoms more frequently than twice a week indicates a persistent, albeit mild, nature.
Attacks:
The asthma episodes interfere with the ability to perform routine daily activities.
Nighttime symptoms:
Occur more than twice a month, indicating a more consistent presence compared to intermittent asthma.
Moderate persistent asthma
Asthma is classified as moderate persistent if, without daily controller medication, the following are true:
Symptoms:
Occur on a daily basis.
The daily occurrence signifies a more constant underlying inflammation.
A short-acting inhaled asthma medication is needed every day to manage these symptoms.
Symptoms’ impact:
Symptoms interfere with the ability to participate in normal daily activities.
Nighttime symptoms:
Occur more than once a week, but not on every single night.
Severe persistent asthma
Asthma is considered severe persistent if, without consistent controller medication, the following characteristics are observed:
Symptoms:
Occur throughout the entire day, indicating a significant and constant airway obstruction.
Severely limit the ability to perform daily physical activities.
Nighttime symptoms:
Occur frequently, and may even happen every night, significantly disrupting sleep.
Etiology/Risk Factors.
The development of asthma is complex and influenced by a combination of factors, both from within the individual (endogenous) and from their surroundings (environmental). Genetic makeup plays a significant role, and exposure to various triggers can initiate or worsen asthma symptoms.
These factors include:
Endogenous factors (factors originating from within the body)
(a) Genetic predisposition: Asthma tends to run in families, indicating a genetic component. The likelihood of developing asthma is higher if close relatives also have the condition. Identical twins show a higher rate of both having asthma compared to non-identical twins, further supporting the role of genes.
(b) Atopy: This refers to a genetic tendency to develop allergic reactions. People with atopy are prone to developing hypersensitivity reactions to common substances, leading to conditions like hay fever (allergic rhinitis), atopic eczema (dermatitis), and asthma. Atopy is characterized by the body’s increased production of a specific antibody called IgE in response to allergens, and often there’s a family history of allergic diseases.Infection and Diseases
(a) Upper Respiratory Tract viral infections: Viral infections affecting the nose and throat are common triggers for asthma exacerbations (flare-ups).
* Rhinitis and Sinusitis: Inflammation of the nasal passages and sinuses can worsen asthma symptoms.
* Postnasal drip: Mucus dripping down the back of the throat can irritate the airways and trigger coughing and asthma symptoms.
* Respiratory syncytial virus infection in infancy: RSV infection during infancy is linked to an increased risk of developing asthma later in life.Drugs: Certain medications can trigger or worsen asthma symptoms in susceptible individuals.
Beta 2 blockers: These medications, often used for heart conditions, can cause the airways to narrow (bronchoconstriction) in some individuals with asthma.
ACEI like Captopril: Angiotensin-converting enzyme inhibitors (ACEIs), a class of drugs used to treat high blood pressure, can cause coughing, which may exacerbate asthma symptoms in some people.
Environmental Factors.
(a) Air Pollution: Exposure to various air pollutants can irritate the airways and trigger asthma symptoms.
* Air pollutants, such as sulfur dioxide, nitrogen dioxide, and diesel particulates released from vehicle exhaust, can worsen asthma.
* Indoor air pollution: Exposure to pollutants inside homes and buildings can also trigger asthma. This includes nitrogen oxides released from cooking stoves and exposure to secondhand cigarette smoke (passive smoking).
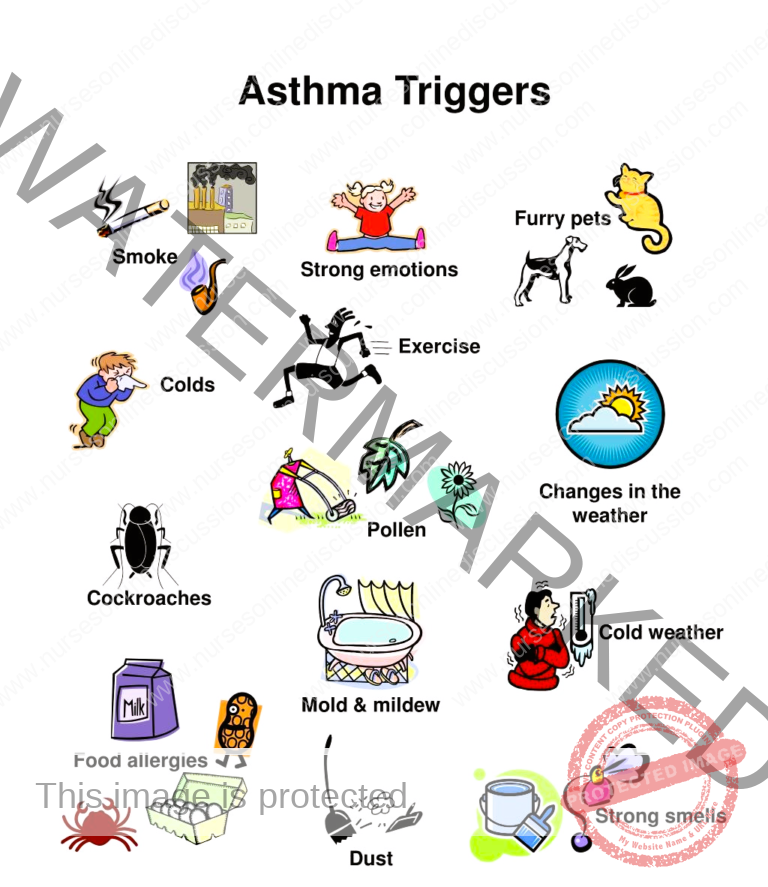
(b) Allergens: Exposure to substances that trigger allergic reactions (allergens) is a significant risk factor for many people with asthma.
* Indoor allergens: Common indoor triggers include allergens from pets like cats, cockroaches, and house dust mites, which are often found in bedding (pillows, mattresses), furniture, carpets, and drapes.
* Outdoor allergens: Common outdoor triggers include pollen grains from trees, grasses, and weeds, as well as animal fur.
* All these inhaled allergens are frequent triggers for asthma attacks.
* Food: Certain food allergies can sometimes trigger asthma symptoms in sensitive individuals. Common culprits include nuts, chocolate, and milk.
(c) Occupational Exposure: Exposure to certain substances in the workplace can lead to occupational asthma.
* Occupational asthma is a recognized condition, and it’s relatively common in some professions.
* Over 200 different substances (sensitizing agents) have been identified as potential triggers for occupational asthma.
* Examples include certain chemicals and fungal amylase, an enzyme found in wheat flour that can affect bakers.
(d) Changes in the weather: Fluctuations in weather conditions, such as changes in temperature or humidity, can sometimes trigger asthma symptoms.
(e) Irritants: Exposure to various irritants can inflame the airways and trigger asthma. This includes things like household cleaning sprays and fumes from paints.
(i) Others may include:
* Strong emotions: Intense emotions like fear or even laughing can sometimes trigger asthma symptoms.
* Exercise or hyperventilation: Physical exertion or rapid, deep breathing can trigger exercise-induced asthma in some individuals.
* Temperature and weather changes: As mentioned earlier, variations in temperature and weather patterns can be asthma triggers for some people.
Pathophysiology of Asthma
Asthma’s fundamental problem is reversible inflammation in the airways, leading to a reduction in the diameter of breathing passages.
Trigger Factor
Exposure to a specific stimulus sets off airway inflammation, initiating the activation of mast cells located within the respiratory tracts.
Activation
Upon activation, mast cells release various chemical mediators. These substances sustain the inflammatory process, causing:
Increased blood flow to the affected area.
Vasoconstriction (narrowing of blood vessels).
Excessive mucus production.
Influx of leukocytes (white blood cells) to the inflammation site.
Contraction of airway smooth muscles.
Overall bronchoconstriction (narrowing of airways).
Narrow Breathing Passages
The immediate bronchial constriction triggered by allergens directly results from the release of mediators from mast cells. These mediators directly induce the contraction of the muscles surrounding the airways.
Asthma features
With the progression of asthma, inflammation intensifies, and other elements can contribute to airflow limitation. Noticeable signs include:
Wheezing during respiration.
Coughing.
Dyspnea (shortness of breath).
Chest tightness.
Full Pathophysiology Context
Exposure to an inciting agent triggers the release of diverse substances from immune cells, including mast cells, eosinophils, basophils, neutrophils, and macrophages.
The process commences with the activation of T-lymphocytes. These cells produce lymphokines, which amplify the immune response, notably by stimulating IgE antibody production and subsequently initiating allergic reactions.
The early phase reaction involves the release of IgE antibodies and the activation of cells bearing receptors specific to these antibodies, particularly mast cells in the airways.
These activated cells generate pro-inflammatory mediators like histamine, eicosanoids, and reactive oxygen species (ROS). These molecules contribute to the inflammatory process.
Some substances, such as histamine, adenosine, bradykinin, and major basic protein, are preformed and stored within cellular granules.
Other substances, such as lipid mediators derived from arachidonic acid like leukotrienes and prostaglandins, are synthesized and released immediately in response to asthmatic triggers.
These pro-inflammatory mediators induce:
Contraction of airway smooth muscles.
Stimulation of mucus secretion.
Vasodilation (widening of blood vessels).
Airflow obstruction is caused by inflammatory mediators leading to microvascular leakage, resulting in plasma exudation into the airways.
This plasma protein leakage leads to a thickened, congested, and swollen airway wall, ultimately narrowing the airway lumen (passage).
The late-phase reaction develops approximately 6 to 9 hours post the initial early-phase reaction. It is characterized by the recruitment and activation of other immune cells, such as eosinophils, CD4+ cells, basophils, neutrophils, and macrophages. Adhesive interactions between these cells further contribute to the inflammatory environment.
T cells are recruited around 24 hours after the early-phase reaction and are believed to be involved in the chronic aspects of asthma and in increasing airway sensitivity to various stimuli (non-specific bronchial hyper-responsiveness).
Collectively, these substances contribute to airway inflammation, including:
Edema (swelling).
Desquamation of the bronchial epithelium (shedding of the bronchial lining).
Hypertrophy (enlargement) of respiratory tract smooth muscles.
These chemical mediators also increase the sensitivity of airway smooth muscles and increase bronchioles permeability to allergens, infectious agents, other inflammatory mediators, and irritants.
Consequently, mucus production is increased, potentially leading to mucus plugging of the airways. This impairs the airways’ ability to clear harmful substances.
Due to these combined effects, individuals experience airway obstruction and require accessory muscles to aid breathing.
Airway obstruction in asthma results from a combination of:
Bronchial inflammation.
Smooth muscle constriction around airways.
Blockage of the airway lumen by mucus, inflammatory cells, and cellular debris.
Symptoms associated with this obstruction include:
Dyspnea (difficulty breathing).
Coughing.
Wheezing (whistling sound during breathing).
Headache.
Tachycardia (rapid heart rate).
Syncope (fainting).
Diaphoresis (excessive sweating).
Pallor (paleness).
Cyanosis (bluish discoloration due to low oxygen).
Clinical Manifestations
Principal symptoms
Recurrent wheezing episodes.
Episodes of breathlessness.
Typical symptoms
Wheezing sound.
Chest tightness.
Shortness of breath.
Non-productive cough (cough without much phlegm).
Signs
Diaphoresis (excessive sweating).
Tachycardia (rapid heart rate).
Widened pulse pressure (increased difference between systolic and diastolic blood pressure).
Low blood oxygen levels.
Central cyanosis (bluish discoloration of central body parts).
Tachypnoea (increased breathing rate, >25 breaths/minute).
Bluish discoloration.
Weak respiratory effort.
Bradycardia or arrhythmia (slow or irregular heartbeats).
Hypotension (low blood pressure).
Extreme fatigue.
Disorientation.
Loss of consciousness.
Acute severe asthma
Breathing rate ≥ 25 breaths per minute.
Heart rate ≥ 110 beats per minute.
Inability to speak in full sentences without pausing for breath.
Diagnosis and Investigations
To diagnose asthma, healthcare professionals confirm the presence of recurring symptoms indicative of airway obstruction.
Family history of asthma: Asthma has a genetic predisposition.
Physical Examination: Auscultation (listening with a stethoscope) to detect wheezing, observing for dyspnea, and checking for cyanosis.
Diagnostic techniques: Chest X-rays, blood and sputum tests, skin allergy tests, and a complete blood count (CBC).
Management of Asthma
Aims
The main objectives in managing asthma are to achieve and maintain control of asthma symptoms. Another vital goal is preventing asthma attacks or flare-ups. Maintaining lung function as close to normal and stable as possible is also key. It is important to minimize or prevent adverse effects from asthma medications. A significant long-term aim is to prevent the development of permanent limitations in airflow. Ultimately, preventing asthma-related deaths is paramount. Restoring lung function to a typical level, or the best level achievable, is crucial for quality of life. Reducing the frequency and severity of acute asthma episodes is a central aim. For children, ensuring normal growth and development is a critical consideration. Minimizing school absenteeism due to asthma is another practical goal of effective management.
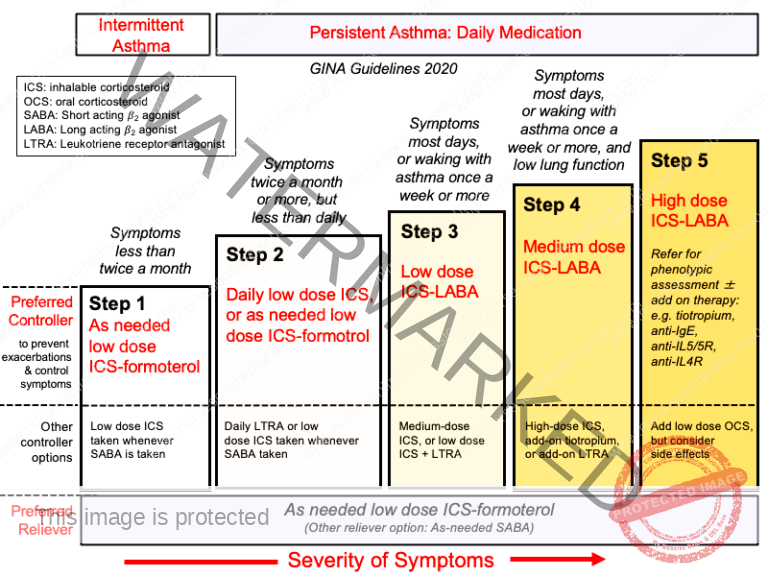
Step Ladder Management
This stepwise approach to asthma treatment involves adjusting medication intensity based on symptom control, increasing treatment when needed and potentially decreasing it if control is sustained.
Step 1: For individuals experiencing infrequent asthma symptoms, occasional use of inhaled short-acting beta-2-agonist bronchodilators is recommended. These medications offer rapid symptom relief by relaxing the muscles surrounding the airways. They are used “as needed” for acute symptom management.
Step 2: If symptoms become more persistent or occur more often, introducing regular preventative therapy is advised. Inhaled corticosteroids (ICS) are the preferred initial controller medication because of their effectiveness in reducing airway inflammation, which is the underlying cause of asthma. These are taken daily to prevent symptoms.
Step 3: If asthma control remains less than optimal despite consistent inhaled corticosteroid use, the next step involves adding a long-acting beta-2-agonist (LABA). Examples of LABAs, such as salmeterol and formoterol, provide extended bronchodilation when used in combination with an inhaled corticosteroid. LABAs work synergistically with ICS to improve asthma control.
Step 4: When asthma control is still insufficient even with the combination therapy from Step 3, adding a fourth medication might be considered. Examples include leukotriene receptor antagonists, which block the action of inflammatory leukotrienes, or theophyllines, which act as bronchodilators with some anti-inflammatory properties. These are add-on therapies for more difficult-to-control asthma.
Step 5: In severe, difficult-to-control asthma cases, continuous or frequent use of oral corticosteroids may be necessary. These are potent anti-inflammatory medications but are usually reserved for severe cases due to the potential for systemic side effects with prolonged use. Oral corticosteroids are used as a last resort for severe exacerbations and chronic severe asthma.
Peak Flow Monitoring
Peak flow meters. Devices used to measure the maximum rate of air exhaled during a forceful breath.
Daily peak flow monitoring. Recommended for individuals meeting one or more of the following conditions:
Experiencing asthma that is consistently moderate to severe.
Having difficulty in perceiving changes in their breathing or worsening symptoms.
Showing reactions to environmental or work-related factors without a clear cause.
Based on clinical judgment or patient preference.
Function. Utilized to assess the severity of asthma; when combined with symptom tracking, it provides insight into the current level of asthma control.

Pharmacological Management
Quick Response Medicines
These medications are for immediate relief of acute asthma symptoms. They are used during asthma attacks to quickly open up the airways.
Bronchodilators
These drugs function by relaxing airway muscles, facilitating easier breathing during an asthma attack. They provide rapid relief.
These are the primary treatment for sudden asthma symptoms. They offer quick relief by stimulating beta-2 receptors in the lungs, resulting in rapid bronchodilation. Examples include:
Salbutamol (albuterol)
Terbutaline
Levalbuterol
Pirbuterol
These are typically administered via inhaler or nebulizer for fast action.
These medications operate by blocking acetylcholine action, a neurotransmitter that can cause airway constriction and mucus production. Ipratropium is a commonly used anticholinergic, especially in acute asthma flare-ups, often combined with a beta-2 agonist for enhanced effect.
While mainly used for long-term control, intravenous corticosteroids like hydrocortisone can be used in severe acute asthma attacks. They work to reduce airway inflammation and prevent further worsening. Their effect is not instant, but they are vital in controlling the underlying inflammatory process during severe episodes.
Long term Medicines
These medications are used regularly to manage asthma symptoms and prevent exacerbations. They are taken daily to keep asthma under control.
Anti-inflammatory drugs
These medications target the underlying inflammation in the airways, which is the hallmark of asthma.
Montelukast is a leukotriene receptor antagonist that blocks leukotrienes, inflammatory chemicals implicated in asthma. Levocetirizine, an antihistamine, is not a primary long-term asthma controller but may be used in patients where allergies are a trigger.
Inhaled corticosteroids (ICS) are the foundation of long-term asthma management. They effectively reduce airway inflammation, thus decreasing the frequency and severity of asthma symptoms. Consistent daily use is key for their preventative action.
Bronchodilators
These medications provide prolonged bronchodilation, lasting up to 12 hours. They are always used in combination with an inhaled corticosteroid and should never be used alone for asthma management due to safety concerns. Examples include:
Salmeterol
Formoterol
They enhance asthma control when used with ICS.
Theophylline is a bronchodilator with mild anti-inflammatory properties. It is used less often now because of its narrow therapeutic window and potential side effects, but may be considered in some patients with difficult-to-manage asthma. Dosage is carefully adjusted based on individual needs and monitoring of blood levels to ensure safety and effectiveness.
Nursing Care after an Acute Attack
These are the immediate nursing actions for a patient who has just experienced an acute asthma attack.
Administer high flow oxygen to alleviate hypoxemia (low blood oxygen). Supplemental oxygen helps to improve blood oxygen saturation, addressing the oxygen deficit during an asthma attack.
Position the patient in a propped-up position in bed to facilitate improved breathing. Using a semi-Fowler’s or high-Fowler’s position aids lung expansion and enhances ventilation by using gravity.
Establish IV access for intravenous medication administration. IV access allows for prompt delivery of necessary drugs to treat the acute exacerbation.
Administer IV fluids if dehydrated and encourage oral fluid intake. Dehydration can worsen mucus plugging and hinder secretion clearance. IV fluids rehydrate, and oral intake supports ongoing hydration.
Implement a fluid balance chart if the patient is receiving IV fluids. Accurate monitoring of fluid intake and output is crucial, especially with IV fluids, to prevent fluid overload or further dehydration.
Monitor all patient vital signs to assess treatment response. Regular vital sign checks (heart rate, blood pressure, respiratory rate, oxygen saturation) help evaluate the patient’s reaction to interventions and identify any deterioration.
Provide emergency treatments like nebulized salbutamol or IV aminophylline /hydrocortisone to relieve breathing difficulty. These medications are essential for quickly reversing bronchospasm (nebulized salbutamol) and reducing airway inflammation (IV hydrocortisone, IV aminophylline – a bronchodilator).
Administer all prescribed medications and monitor for any drug side effects. Ensuring timely administration of all ordered medications, including maintenance drugs, is vital. Close observation for any adverse drug reactions is also a crucial nursing responsibility.
NURSINGDIAGNOSIS
These are clinical judgments regarding patient responses to actual or potential health problems.
Impaired breathing pattern related to severe lung inflammation, evidenced by wheezing. This diagnosis identifies altered breathing rate, depth, and rhythm due to lung inflammation, with wheezing as a sign.
Impaired tissue oxygenation related to airway inflammation, evidenced by cyanosis. This indicates insufficient oxygen reaching tissues due to airway inflammation, with cyanosis (bluish skin) as evidence.
Extreme anxiety related to recurrent life-threatening asthma attacks, evidenced by frequent questioning. This acknowledges significant patient anxiety due to asthma attack recurrence and potential danger, with frequent questions as a behavioral indicator.
Ineffective airway clearance related to increased mucus and bronchospasm, evidenced by wheezing and dyspnea. This highlights difficulty clearing secretions and maintaining open airways due to mucus and airway narrowing, with wheezing and shortness of breath (dyspnea) as key signs.
Impaired gas exchange related to altered oxygen delivery. This focuses on compromised oxygen and carbon dioxide exchange in the lungs due to asthma.
Complications of Asthma
These are potential negative outcomes that can result from asthma.
Airway infection like bronchiolitis. Inflamed asthma airways can be more susceptible to infections like bronchiolitis, inflammation of small lung airways.
Cor pulmonale; Heart Failure secondary to chronic lung disease. Cor pulmonale is right-sided heart failure from chronic lung disease. Chronic severe asthma can lead to cor pulmonale, straining the right heart. Rheumatic heart disease is a separate condition mainly affecting heart valves.
Pneumonia. Inflammation and mucus in airways can increase pneumonia risk, a lung infection.
Hypoxic respiratory failure in severe disease. In severe asthma, lungs may not provide enough oxygen, leading to hypoxic respiratory failure.
Atelectasis. Lung collapse, partial or complete, can occur due to mucus plugging airways.
Pneumonia (repeated emphasis).
Status asthmaticus. A severe, prolonged asthma attack unresponsive to usual treatments, a medical emergency.
Pneumothorax /Air-leak syndromes (rare). Rarely, pressure changes during severe attacks can rupture the lung, causing air leak into the chest space (pneumothorax) or other air leak syndromes.
Death. Despite treatment advances, asthma can be fatal, especially in severe exacerbations or if poorly managed.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

