Conditions of the eye
Subtopic:
Proptosis
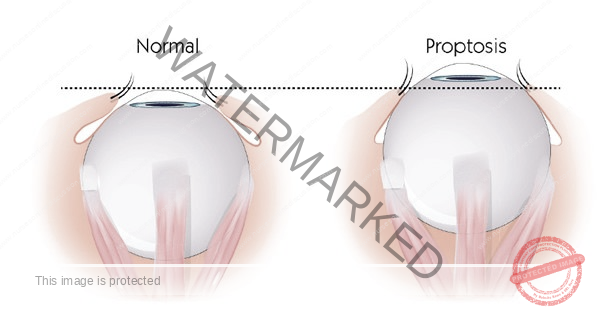
Proptosis of the eye, also known as exophthalmos, is a condition characterized by the bulging or protrusion of one or both eyes from their normal position within the eye sockets. This occurs due to changes in the space behind the eyeball.
It can arise from various underlying factors that affect the tissues and structures surrounding the eyes within the bony orbit.
Causes and Risk Factors:
Thyroid Eye Disease: A frequent cause of proptosis is thyroid eye disease, also termed Graves’ ophthalmopathy. This autoimmune condition involves the immune system mistakenly attacking the tissues around the eyes, leading to inflammation and the forward displacement of the eyeballs.
Orbital Cellulitis and Infections: Infections within the eye socket, referred to as orbital cellulitis, can induce swelling and subsequent proptosis. This is an emergent condition requiring prompt treatment.
Orbital Tumors: Growths within the eye socket, whether non-cancerous (benign) or cancerous (malignant), can exert pressure and cause the eyes to bulge outwards. These growths necessitate timely evaluation and appropriate medical or surgical intervention.
Trauma or Injury: Significant physical trauma or injury to the eye itself or the bony orbit surrounding it can cause the eye to shift from its normal position, resulting in proptosis.
Allergic Reactions: Severe allergic responses affecting the eye and surrounding tissues can trigger substantial swelling, which in turn can push the eyes forward.
Risk Factors:
Thyroid disorders, such as hyperthyroidism (overactive thyroid gland), significantly increase the risk.
A prior history of injuries or surgical procedures involving the eyes can be a contributing factor.
A family history of thyroid eye disease or other eye-related conditions may predispose individuals.
Certain types of infections capable of affecting the eye socket and adjacent tissues can elevate the risk.
Classifications of Proptosis:
Proptosis, also known as exophthalmos, can be categorized using several different criteria to understand its nature and cause:
Based on Onset:
a. Acute Proptosis: Characterized by a sudden development of bulging eyes. This rapid onset is often linked to infections, physical trauma, or acute inflammatory conditions.
b. Chronic Proptosis: Defined by a gradual and persistent outward movement of the eye. This slower progression is commonly associated with conditions like thyroid eye disease or slowly developing tumors.
Based on Cause:
a. Thyroid-Related Proptosis: Specifically caused by thyroid eye disease, and is frequently seen in conjunction with hyperthyroidism (Graves’ ophthalmopathy).
b. Inflammatory Proptosis: Arises due to infections or autoimmune disorders that cause inflammation and swelling within the tissues surrounding the eye.
c. Neoplastic Proptosis: Results from the presence of tumors, either benign or malignant, located within the bony orbit of the eye.
d. Traumatic Proptosis: Occurs as a direct consequence of injuries or fractures affecting the eye and the surrounding bony structures of the orbit.
e. Allergic Proptosis: Develops due to severe allergic reactions that impact the eye and the tissues within the eye socket.
Based on Uni or Bilaterality:
a. Unilateral Proptosis: Indicates that only one eye is affected by the bulging. This is often observed in localized conditions or following trauma to a single eye.
b. Bilateral Proptosis: Signifies that both eyes are exhibiting the outward protrusion. This is more commonly seen in systemic conditions or those related to thyroid disorders.
Based on Severity:
a. Mild Proptosis: Involves a minimal degree of eye protrusion and typically does not significantly affect vision or the normal functioning of the eye.
b. Moderate Proptosis: Characterized by a noticeable bulging of the eye, which may result in a mild to moderate impact on eye movement and sharpness of vision (visual acuity).
c. Severe Proptosis: Represents a pronounced outward bulging of the eye that can lead to significant visual impairment, restricted movement of the eye, and the potential for complications.
Eye Structure: Anatomy of the eye
The eye is a complex organ comprised of several key components:
Cornea: This is the transparent, outermost front part of the eye that allows light to enter the eye, initiating the process of vision.
Iris: The colored part of the eye, which functions like a diaphragm in a camera, controlling the size of the pupil to regulate light entry.
Pupil: The black circular opening in the center of the iris that adjusts in size to manage the amount of light entering the eye.
Lens: Situated behind the iris, this transparent structure focuses incoming light onto the retina, allowing for clear vision at varying distances.
Retina: The light-sensitive layer lining the back of the eye, where images are formed and then converted into electrical signals.
Optic Nerve: This crucial nerve transmits the visual information as electrical signals from the retina to the brain, where they are interpreted.
Orbit and Eye Socket:
The orbit, also known as the eye socket, is a bony cavity within the skull that provides housing and protection for the eye and its associated structures.
The orbit is formed by the fusion of several bones, including the frontal bone, maxilla, and zygomatic bone, among others. Its primary functions are to safeguard the eye and to offer stable points of attachment for the muscles that control eye movement.
Within the orbital cavity are various soft tissues vital for eye function:
Extraocular Muscles: These six muscles are responsible for controlling the movement of the eyeball in different directions, enabling a wide range of gaze.
Fat Tissue: This adipose tissue acts as a cushion, providing support and protection for the eye within the bony confines of the orbit.
Blood Vessels and Nerves: A network of blood vessels ensures the eye receives necessary nutrients and oxygen, while nerves transmit sensory information to and from the eye, including visual signals and sensations.
Pathophysiology
Proptosis arises when there is an abnormal increase in the volume of tissue within the orbit, which forces the eye to bulge forward out of its normal position. This increase in volume can be due to various factors.
This increase in volume can be caused by swelling of tissues, the growth of abnormal masses, or the displacement of normal structures within the confined space of the eye socket. As a consequence of proptosis, the eyeball is pushed outwards, leading to several observable and functional effects:
Visible Bulging: The affected eye or eyes will appear more prominent compared to the other eye due to this forward displacement from the socket.
Limited Eye Movement: The increased pressure and altered positioning within the orbit can impede the normal range of motion of the eye, making it difficult to move the eye fully in all directions.
Exposure of the Eye Surface: The bulging eye may not be able to close completely, leaving the surface of the eye exposed. This can lead to problems with proper lubrication, resulting in dryness, irritation, and potential damage to the cornea.
Vision Problems: The misalignment of the eyes caused by proptosis can lead to double vision (diplopia), as the brain receives two different images. Additionally, the altered shape of the eyeball can cause blurred vision.

Signs and Symptoms of Proptosis
A. Bulging or Protruding Eye(s): A key indicator of proptosis is the noticeable outward projection of one or both eyeballs from their usual position within the eye sockets. The affected eye(s) may appear larger and more prominent than normal, a change that can be alarming to the individual.
B. Redness and Swelling: Proptosis often presents with redness and puffiness around the affected eye(s) and the surrounding tissues. The increased pressure within the confined space of the eye socket can trigger inflammation, resulting in a visibly swollen and irritated appearance of the eye area.
C. Vision Changes and Diplopia (Double Vision): Alterations in eyesight are common in proptosis. The shifted position of the eye can disrupt its normal alignment, leading to double vision, medically known as diplopia. This occurs when the images perceived by each eye are no longer correctly aligned and merged by the brain, resulting in the perception of two overlapping images instead of a single, clear one.
D. Pain or Discomfort: Individuals with proptosis may experience varying degrees of pain or unease in and around the affected eye(s). The pressure exerted and the stretching of tissues within the eye socket can cause this pain, which may be exacerbated by eye movements or physical touch.
E. Eyelid Abnormalities: Proptosis can influence the position and functionality of the eyelids. Some individuals may find it difficult to fully close the affected eye, leading to incomplete blinking. This can result in corneal exposure, which may cause dryness and irritation of the eye’s surface.
F. Photophobia (Light Sensitivity): The increased protrusion of the eyeball can make it more susceptible to light, leading to discomfort or even pain when exposed to bright light. This heightened sensitivity is known as photophobia.
G. Watery Eyes: Proptosis can disrupt the normal flow and drainage of tears, leading to excessive tearing, a condition known as epiphora.
H. Displacement of the Eye Muscles: The abnormal positioning of the eye may cause the extraocular muscles, which are responsible for controlling eye movement, to become misaligned. This can lead to limited or unusual eye movements.
I. Changes in Eye Appearance: Beyond the obvious bulging, proptosis can cause other alterations in the way the eye(s) look. This may include a widening of the palpebral fissure, which is the opening between the upper and lower eyelids, or changes in the apparent position of the iris.
J. Pressure Sensation: Some individuals experiencing proptosis may describe a distinct feeling of pressure or heaviness around the eyes. This sensation is due to the increased volume of tissue occupying the space within the eye socket.
Diagnosis of Proptosis
Clinical Examination by Healthcare Professionals: The initial step in diagnosing proptosis involves a comprehensive clinical evaluation conducted by medical professionals, typically ophthalmologists or specialized eye doctors. During this examination, several assessments may be performed to evaluate the condition of the eyes and surrounding structures:
Visual Acuity Test: This standard test measures the sharpness of the patient’s vision at various distances, often using a Snellen eye chart.
Eye Movement Examination: This assessment checks for any limitations or abnormalities in the movement of the affected eye(s), helping to identify potential muscle or nerve issues.
Pupil Examination: The doctor will evaluate the size and reactivity of the pupils to light, which can indicate neurological or eye-related problems.
Eye Pressure Measurement: Also known as tonometry, this test measures the pressure inside the eye (intraocular pressure), which can be elevated in conditions like glaucoma.
Slit-Lamp Examination: A specialized microscope with a bright light is used to examine the front structures of the eye in detail, including the cornea, iris, and lens, looking for any abnormalities.
Fundoscopy: Using an ophthalmoscope, the doctor visualizes the back of the eye, including the retina and optic nerve, to check for signs of disease or damage.
Imaging Studies (MRI, CT Scan) for Accurate Assessment: To gain a detailed view of the eye and the structures within the orbit, imaging studies are crucial. The two most common modalities used for diagnosing proptosis are:
Magnetic Resonance Imaging (MRI): This non-invasive technique uses powerful magnets and radio waves to create highly detailed images of the eye, orbit, and surrounding soft tissues. MRI is particularly useful for identifying abnormal growths, inflammation, or subtle changes in the eye and orbital structures.
Computed Tomography (CT Scan): CT scans use X-rays to create cross-sectional images of the eye and orbit. They provide precise information about the bony structures and can effectively identify fractures, tumors, or other conditions affecting the eye socket.
Differential Diagnosis
When diagnosing proptosis, it’s important to consider other conditions that may present with similar symptoms. This process of differential diagnosis helps to narrow down the possibilities and arrive at the correct diagnosis. Key conditions to consider include:
Thyroid Eye Disease (Graves’ Ophthalmopathy): This autoimmune condition is a frequent cause of proptosis and may be accompanied by other signs of hyperthyroidism, such as rapid heartbeat and weight loss.
Orbital Cellulitis: An infection of the tissues surrounding the eye, characterized by redness, swelling, and pain in the affected area.
Orbital Tumors: Growths, whether benign or malignant, within the eye socket that can physically push the eye forward.
Allergic Reactions: Severe allergic reactions can cause significant swelling and redness of the eyes and surrounding tissues.
Traumatic Eye Injury: Significant physical trauma to the eye or surrounding structures can lead to eye displacement and proptosis.
Management of Proptosis
The management of proptosis depends on the underlying cause and the severity of the condition. Treatment strategies can range from medical management to surgical interventions.
Medical Management:
Treating Underlying Conditions (e.g., Thyroid Disorders): If proptosis is a symptom of an underlying condition like thyroid eye disease, the primary focus is on managing that condition. For example, in Graves’ ophthalmopathy, treatment to control the overactive thyroid using medications, radioactive iodine, or surgery may help to stabilize or improve the eye symptoms.
Corticosteroids and Immunosuppressive Therapy: In cases of proptosis associated with inflammation or autoimmune conditions, corticosteroids (steroids) may be prescribed. These anti-inflammatory medications help to reduce swelling and inflammation around the eyes. For more severe cases, immunosuppressive therapy may be used to modulate the immune system’s response and manage the underlying cause of the inflammation.
Surgical Interventions: (Pre and Post operative care)
Surgical options are considered when medical management is insufficient or when there are structural issues contributing to the proptosis.
Orbital Decompression Surgery: This surgical procedure aims to reduce pressure within the eye socket by creating more space. It involves removing or reshaping portions of the bony orbit to allow the displaced eye to move back to a more normal position. This surgery is commonly performed for patients with proptosis caused by thyroid eye disease or other conditions causing compression of the optic nerve.
Orbital Tumor Removal: If proptosis is caused by benign or malignant tumors within the orbit, surgical removal of the tumor may be necessary. The goal is to excise the tumor completely while preserving the surrounding eye structures and restoring a more natural eye position.
Eye Realignment Surgery: In cases of proptosis resulting from muscle imbalances or nerve problems, eye realignment surgery may be recommended. This procedure aims to reposition the affected eye(s) to improve their alignment and reduce or eliminate double vision.
Nursing Care for Patients with Proptosis
Nurses play a crucial role in the care and management of patients with proptosis, providing education, monitoring, and emotional support.
Patient Education:
Understanding the Diagnosis and Treatment Plan: Nurses are responsible for educating patients about their proptosis diagnosis, explaining the underlying cause, and discussing the available treatment options. They should ensure that patients fully understand this information and address any questions or concerns they may have in a clear and supportive manner.
Eye Care and Hygiene: Nurses should provide detailed guidance on proper eye care and hygiene practices to help prevent complications such as dry eyes and corneal exposure. This includes instructing patients on the correct use of lubricating eye drops, advising them to avoid rubbing their eyes, and emphasizing the importance of maintaining a clean eye area to reduce the risk of infections.
Monitoring and Assessment:
Visual Acuity Checks: Nurses should perform regular assessments of the patient’s visual acuity to monitor for any changes in their vision. Any abnormalities in visual acuity should be promptly recorded and reported to the healthcare team.
Assessing for Complications: Nurses are vigilant in monitoring for potential complications related to proptosis, such as signs of optic nerve compression, corneal exposure, and eye infections. Regular assessments are key to early detection of these issues, allowing for timely intervention.
Emotional Support for Patients and Families:
Addressing Psychological Impact: Living with proptosis can have a significant impact on a patient’s emotional well-being and self-esteem. Nurses should provide empathetic support, actively listen to patients’ concerns, and offer reassurance to help alleviate any anxiety or distress related to their condition.
Encouraging Coping Mechanisms: Nurses can recommend stress-reducing techniques and coping mechanisms to help patients manage their emotions and adapt to the challenges of living with proptosis. Encouraging patients to engage in hobbies, relaxation techniques, or support groups can be particularly beneficial.
Positioning the Patient After Surgery: Following orbital surgeries, nurses play a key role in positioning the patient to minimize swelling and promote comfort. Elevating the head of the bed and ensuring the patient’s head remains elevated can help reduce post-operative swelling and pressure around the eyes.
Other measures:
Lubricating Eye Drops: For patients experiencing dry eye symptoms due to incomplete eye closure, artificial tears or lubricating eye drops can provide relief by keeping the eyes moist and reducing discomfort.
Eye Protection: Patients with proptosis should be advised to wear appropriate eye protection, such as safety glasses or goggles, to safeguard their eyes from potential injury.
Eye Patching: In cases where there is significant corneal exposure, eye patches may be used to protect the cornea and promote healing.
Vision Therapy: For patients with residual double vision, vision therapy exercises may be prescribed to help improve eye muscle coordination and reduce the impact of diplopia.
Psychological Support: Dealing with proptosis and its effects on appearance and vision can be emotionally challenging. Providing psychological support and counseling can help patients cope with the condition and improve their self-esteem.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

