Palliative Care Emergencies
Subtopic:
Hypercalcemia
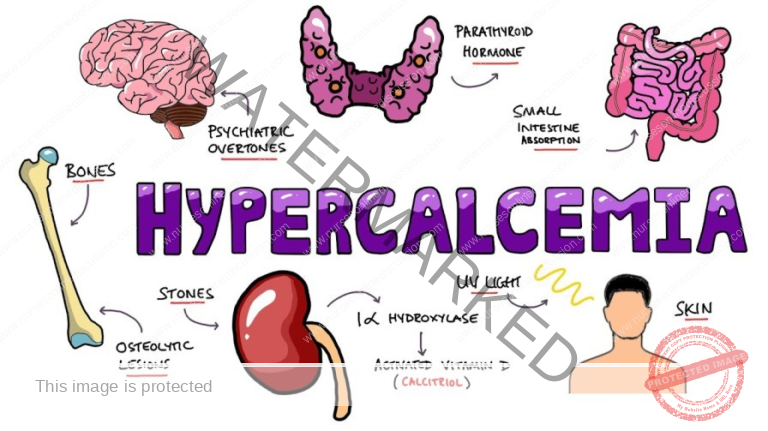
Hypercalcemia, a potentially life-threatening metabolic disorder, is frequently encountered in oncology settings, particularly in patients diagnosed with breast cancer, multiple myeloma, and tumors of the head, neck, and kidney.
It is clinically defined as a condition where the serum calcium level exceeds 10.4 mg/dL (or >2.60 mmol/dL).
Hypercalcemia specifically associated with cancer is termed Hypercalcemia of Malignancy (HCM). HCM is commonly linked to primary malignancies, including cancers of the:
Breast
Lung
Head and Neck
Kidney (Renal)
Esophagus
Gastrointestinal Tract
Cervix
Leukemias
Multiple Myeloma
Melanomas
The most prevalent mechanism underlying HCM is bone metastasis. Cancerous tumors metastasizing to bone tissue can trigger a pathological process leading to the release of calcium from the bones into the bloodstream, resulting in hypercalcemia. Furthermore, certain cancer treatment modalities, notably estrogen and anti-estrogen therapies, have also been associated with an increased risk of developing HCM in susceptible individuals.
While malignancy is a major cause, it’s important to note that non-cancer-related factors can also contribute to the development of hypercalcemia. These non-malignant factors include:
Prolonged immobility, leading to bone mineral loss and calcium release.
Dehydration, concentrating serum calcium levels.
Excessive dietary intake of calcium-rich foods or calcium supplements.
Over-supplementation with Vitamin D, enhancing calcium absorption.
Decreased levels of parathyroid hormone (hypoparathyroidism), disrupting calcium regulation.
Vitamin A intoxication (hypervitaminosis A), affecting bone metabolism.
Causes of Hypercalcemia:
Cancer-Specific Etiology: Certain cancer types exhibit a strong association with hypercalcemia. These malignancies frequently implicated in HCM include:
Breast cancer
Lung cancer (particularly squamous cell carcinoma)
Kidney (renal cell) cancer
Leukemias (certain types)
Multiple myeloma
Melanomas (metastatic melanoma)
The presence of these cancers can disrupt normal calcium homeostasis, often leading to the release of calcium from bone metastases into the bloodstream, contributing to hypercalcemia.
Cancer Treatment-Related Hypercalcemia: Specific cancer treatment modalities can paradoxically contribute to the development of hypercalcemia as a side effect. Notably, therapies such as:
Estrogen therapy (used in some breast cancers)
Anti-estrogen agents (e.g., tamoxifen, used in hormone-sensitive breast cancers)
can sometimes impact calcium regulation and contribute to elevated calcium levels in susceptible patients.
Non-Malignant Hypercalcemia Causes: Hypercalcemia can also arise from a variety of non-cancer-related factors, reflecting disruptions in normal calcium metabolism. These non-malignant causes include:
Prolonged immobility: Extended periods of immobility or bedrest can lead to bone mineral loss and subsequent release of calcium into the circulation, elevating serum calcium levels.
Dehydration: Fluid volume deficit or dehydration can concentrate serum electrolytes, including calcium, leading to a relative increase in measured calcium levels.
Excessive Calcium and Vitamin D Intake: Over-supplementation or excessive dietary intake of calcium and Vitamin D can overwhelm the body’s regulatory mechanisms and result in hypercalcemia.
Hypoparathyroidism (Decreased Parathyroid Hormone): Paradoxically, decreased levels of parathyroid hormone (PTH), which normally regulates calcium levels, can sometimes lead to hypercalcemia in certain conditions, disrupting calcium homeostasis.
Vitamin A Intoxication (Hypervitaminosis A): Excessive intake or supplementation with Vitamin A can, in rare cases, contribute to hypercalcemia by affecting bone metabolism and calcium release.
Lytic Bone Lesions and Calcium Release: In the context of malignancy, hypercalcemia is often directly caused by lytic bone lesions. These lesions are characterized by:
Destructive bone abnormalities where cancer cells directly invade and destroy normal bone tissue.
Bone destruction in lytic lesions results in the release of calcium from the bone matrix into the bloodstream, significantly contributing to hypercalcemia.
In addition to calcium release from bone, lytic lesions may also impair the normal excretion of urinary calcium, further exacerbating hypercalcemia by reducing calcium elimination from the body.
Signs and Symptoms of Hypercalcemia:
Hypercalcemia can manifest with a wide range of signs and symptoms, affecting multiple organ systems. The severity and specific presentation of symptoms can vary depending on the degree and rate of calcium elevation, as well as individual patient factors. Common signs and symptoms include:
General Malaise: Patients may experience a non-specific sense of feeling unwell, characterized by:
General discomfort and unease.
Vague feelings of being unwell.
Unexplained fatigue and lack of energy.
Nausea and Vomiting: Gastrointestinal disturbances are common, including:
Nausea, with or without food aversion.
Vomiting, which can range from mild to severe and contribute to dehydration.
Anorexia: Loss of appetite or a marked decrease in the desire to eat can occur, contributing to nutritional deficits and weakness.
Constipation: Elevated calcium levels can disrupt normal gastrointestinal motility, leading to:
Constipation, characterized by infrequent bowel movements or difficulty passing stool.
Discomfort and abdominal distention due to decreased bowel function.
Bone Pain: Hypercalcemia can directly cause bone pain, which may be:
Localized to specific areas or generalized throughout the body.
Often described as a deep, aching, or throbbing pain, reflecting the underlying bone abnormalities or metastatic lesions.
Thirst and Polyuria: Renal effects of hypercalcemia include:
Increased thirst (polydipsia), as the body attempts to compensate for fluid loss.
Excessive urination (polyuria), as the kidneys try to excrete excess calcium, leading to increased urine output.
Polydipsia: Polydipsia, or excessive thirst, is a direct consequence of the kidneys’ attempts to excrete excess calcium, leading to dehydration and a compensatory increase in thirst sensation.
Severe Dehydration: Hypercalcemia can significantly contribute to dehydration due to:
Increased fluid loss through excessive urination (polyuria).
Fluid losses from vomiting if nausea and vomiting are present.
Decreased oral fluid intake due to anorexia, nausea, or altered mental status.
Drowsiness: Neurological effects of elevated calcium levels can manifest as:
Drowsiness and lethargy, characterized by excessive sleepiness and reduced alertness.
Confusion and Coma: In severe and untreated hypercalcemia, neurological symptoms can progress to more serious manifestations, including:
Confusion and disorientation, ranging from mild to severe.
Coma, representing a critical and life-threatening state of decreased consciousness.
Cardiac Arrhythmias: Hypercalcemia can disrupt the normal electrical activity of the heart, potentially leading to:
Cardiac arrhythmias, or irregular heart rhythms.
Palpitations (awareness of rapid or irregular heartbeat).
In severe cases, life-threatening arrhythmias or cardiac arrest.
Mental State Changes: Hypercalcemia can affect central nervous system function, resulting in a range of mental status alterations, including:
Difficulty concentrating and impaired attention.
Memory problems and cognitive deficits.
Mood changes, such as depression, anxiety, or irritability.
Generalized changes in mental state and cognitive function.
Hallucinations: In some instances, hypercalcemia can induce perceptual disturbances, leading to:
Hallucinations, which are sensory perceptions in the absence of external stimuli. These may be visual, auditory, or tactile hallucinations.
Jumbled Speech: Neurological effects can also impact speech patterns, causing:
Slurred speech, making it difficult to articulate words clearly.
Jumbled or incoherent speech, reflecting impaired cognitive processing and language formation.
Difficulty finding the right words (aphasia), impairing verbal communication.
Depression and Fatigue: Hypercalcemia can contribute to or exacerbate symptoms of:
Depression, with persistent sadness, loss of interest, and feelings of hopelessness.
Persistent fatigue and unexplained tiredness, further reducing quality of life and functional capacity.
Visual Changes: Some patients with hypercalcemia may report experiencing visual disturbances, such as:
Blurred vision, decreased visual acuity.
Double vision (diplopia).
Photophobia, increased sensitivity to light causing discomfort.
Diagnosis and Investigations for Hypercalcemia:
Diagnosing hypercalcemia involves a combination of clinical assessment and laboratory investigations to confirm elevated calcium levels and determine the underlying cause. Common diagnostic procedures include:
Medical History and Physical Examination: A thorough medical history and physical examination are essential initial steps. These assessments help to:
Identify potential risk factors for hypercalcemia based on the patient’s medical history, including pre-existing conditions, medications, and cancer history.
Assess and document the patient’s presenting symptoms that may be suggestive of hypercalcemia, guiding further diagnostic investigations.
Serum Calcium Level Measurement: Measurement of the serum calcium level in a blood sample is the primary diagnostic test for hypercalcemia. A serum calcium level greater than 2.60 mmol/dL (10.4 mg/dL) is the definitive laboratory indicator of hypercalcemia.
Ionized Calcium Measurement: In certain clinical situations, measuring the ionized calcium level may provide a more accurate and clinically relevant assessment of calcium abnormalities. Ionized calcium represents the physiologically active, unbound form of calcium in the blood.
Parathyroid Hormone (PTH) Level Measurement: Measuring the serum parathyroid hormone (PTH) level is crucial in differentiating between different underlying causes of hypercalcemia. PTH levels can help distinguish between:
Primary hyperparathyroidism: In primary hyperparathyroidism, PTH levels are typically elevated, indicating overactivity of the parathyroid glands as the primary cause of hypercalcemia.
Malignancy-associated hypercalcemia (HCM): In HCM, PTH levels are usually suppressed or low, as the hypercalcemia is driven by factors other than excessive PTH secretion, such as tumor-related calcium release from bone.
Kidney Function Tests: Assessing kidney function is important in the evaluation of hypercalcemia, as hypercalcemia can directly impact renal function and vice versa. Kidney function tests typically include:
Blood Urea Nitrogen (BUN) levels: To assess kidney’s ability to remove waste products from the blood.
Creatinine levels: To measure kidney filtration rate and overall renal function.
These tests help evaluate for potential renal impairment or complications related to hypercalcemia.
Serum Phosphate and Magnesium Levels Measurement: Measuring serum phosphate and magnesium levels in conjunction with calcium can provide additional valuable information to help determine the underlying causes of hypercalcemia. Electrolyte imbalances, including phosphate and magnesium abnormalities, may be associated with certain causes of hypercalcemia.
24-Hour Urine Calcium Measurement: Collecting a 24-hour urine sample for calcium measurement is helpful in evaluating the amount of calcium excreted in the urine over a 24-hour period. This test can assist in:
Determining the rate of urinary calcium excretion.
Aiding in the differential diagnosis of hypercalcemia by distinguishing between causes with high versus low urinary calcium excretion.
Imaging Studies: Various imaging techniques may be utilized to investigate potential underlying causes of hypercalcemia, particularly in cases of suspected malignancy or bone involvement. These imaging studies may include:
X-rays: To evaluate for bone lesions or fractures.
Bone scans: To detect areas of increased bone turnover or metastatic bone disease.
Computed Tomography (CT) scans: To assess for tumors, metastases, or other abnormalities in various organs.
Magnetic Resonance Imaging (MRI): To provide detailed imaging of soft tissues and bone marrow, particularly useful in evaluating multiple myeloma or bone metastases.
Additional Investigations: Depending on the clinical presentation of hypercalcemia, the suspected underlying cause, and initial laboratory findings, further investigations may be warranted. These additional tests can include:
Complete Blood Count (CBC): To assess overall blood cell counts and detect any hematological abnormalities.
Liver Function Tests (LFTs): To evaluate liver function, as liver disease can sometimes be associated with electrolyte imbalances.
Serum Protein Electrophoresis: To investigate for monoclonal proteins suggestive of multiple myeloma, a common cause of HCM.
Vitamin D Levels Assessment: Measuring serum Vitamin D levels to evaluate for Vitamin D-related causes of hypercalcemia, such as Vitamin D intoxication or hypervitaminosis D.
Management of Hypercalcemia
Management of hypercalcemia is guided by the severity of calcium elevation, the underlying cause, and the patient’s overall clinical condition. Treatment strategies typically include:
Hydration Therapy: Intravenous (IV) rehydration with intravenous fluids and close monitoring of fluid balance are fundamental aspects of hypercalcemia treatment. Hydration therapy aims to:
Reverse intravascular volume depletion, which is often a consequence of hypercalcemia-induced polyuria and dehydration.
Dilute serum calcium concentration, reducing the overall calcium level in the bloodstream.
Enhance renal calcium excretion, promoting calcium elimination through increased urine output.
In cases of mild hypercalcemia, aggressive rehydration with normal saline solution administered intravenously at a rate of 100-120 ml/hr may be sufficient as initial therapy to lower calcium levels effectively. Close monitoring of fluid status and electrolytes is essential during rehydration.
Pharmacological Interventions: Medications play a crucial role in lowering serum calcium levels, particularly in moderate to severe hypercalcemia. Bisphosphonates are a class of drugs commonly used as first-line therapy to treat hypercalcemia. Bisphosphonates work by:
Inhibiting osteoclastic bone reabsorption, reducing the breakdown of bone tissue and the release of calcium from bones.
Effectively lowering serum calcium levels, particularly in malignancy-associated hypercalcemia (HCM) where bone metastases are a major contributing factor.
In cases of moderate to severe hypercalcemia, the treatment approach typically involves:Step 1: Rehydration: Initiating intravenous rehydration therapy with normal saline as described above to address volume depletion and promote calcium dilution and excretion.
Step 2: Bisphosphonate Administration: Following rehydration, administering bisphosphonate medications. Pamidronate is a commonly used bisphosphonate for hypercalcemia management.
Intravenous Administration: Bisphosphonates like pamidronate are typically administered intravenously to ensure effective delivery and rapid onset of action.
Pre-hydration Requirement: It is crucial to ensure adequate hydration of the patient before administering bisphosphonates to minimize potential renal side effects and enhance drug efficacy.
Dose Repetition: The bisphosphonate dose may need to be repeated every 3-4 weeks as needed to maintain calcium control, particularly in chronic hypercalcemia associated with malignancy.
Resource Limitations in Developing Countries: It is important to acknowledge that bisphosphonates, while highly effective, may not be readily available in resource-poor countries due to their relatively high cost, limiting access to this essential treatment modality in certain settings.
Corticosteroids: Corticosteroid medications, such as prednisone, may be used in specific types of hypercalcemia, particularly in:
Hematological malignancies: Hypercalcemia associated with certain blood cancers like multiple myeloma or lymphoma that are responsive to steroid therapy.
Less Effective in Solid Tumors: Corticosteroids are generally less effective in lowering calcium levels in hypercalcemia caused by solid tumors compared to hematological malignancies.
Mechanism of Action: Corticosteroids can lower calcium levels through various mechanisms, including:
Decreasing intestinal calcium absorption.
Increasing urinary calcium excretion.
Inhibiting tumor-related factors that promote bone resorption in certain malignancies.
End-of-Life Care Considerations: In cases where:
Bisphosphonates or other calcium-lowering treatments are not available due to resource limitations.
Hypercalcemia is refractory to treatment and indicates that the patient is in the terminal phase of their illness and actively dying.
In these situations, the focus of care appropriately shifts to end-of-life care principles and maximizing patient comfort and dignity. Management strategies prioritize:Comfort Measures: Implementing simple comfort measures to alleviate distressing symptoms and enhance quality of life in the final days or hours.
Regular Mouth Care: Providing frequent and meticulous mouth care to alleviate dry mouth and discomfort, promoting oral hygiene and comfort.
Bowel Care Management: Ensuring effective bowel care to prevent or manage constipation, a common symptom in terminally ill patients, promoting comfort and preventing complications.
Regular Patient Turning and Positioning: Implementing a schedule for regular turning and repositioning of the patient to prevent pressure ulcers, promote skin integrity, and enhance comfort, particularly for immobile or bedridden patients.
Effective Pain and Symptom Control: Prioritizing effective pain management and comprehensive symptom control to alleviate all sources of physical and emotional distress, ensuring a dignified and comfortable end-of-life experience.
Management and Care Specific to Hypercalcemia of Malignancy (HCM):
For Hypercalcemia of Malignancy (HCM), management strategies are tailored to address both the hypercalcemia itself and the underlying cancer:
Treating Underlying Malignancy: A primary approach to managing HCM involves actively treating the underlying malignancy that is driving the hypercalcemia. Cancer-directed therapies may include:
Chemotherapy: To target and reduce tumor burden in chemosensitive cancers.
Radiation therapy: To locally control tumors and reduce bone metastases causing calcium release.
Surgery: In select cases, surgical resection of tumors may be indicated to reduce tumor-related hypercalcemia.
The specific cancer treatment modality chosen depends on the type, stage, and prognosis of the underlying malignancy.
Hydration (Oral): Encourage patients with HCM to maintain adequate hydration by aiming to consume 1 to 2 liters of fluids per day, if they are able to tolerate oral fluids. Oral hydration helps to dilute serum calcium and promote renal calcium excretion.
Fluid Replacement (Intravenous): For patients with moderate to severe HCM (serum calcium levels above 13 mg/dL) or those who are dehydrated or unable to tolerate oral fluids, intravenous fluid replacement is often necessary to:
Restore extracellular fluid volume, which is often depleted due to hypercalcemia-induced polyuria.
Administer 5 to 10 liters of intravenous fluids (typically normal saline) over a period of time to achieve adequate rehydration and calcium dilution.
Saline Administration: In cases of significant dehydration or severe hypercalcemia, the administration of intravenous saline solution is often required. Saline administration helps to:
Restore intravascular volume, improving hydration status.
Correct electrolyte imbalances, including sodium and chloride levels that may be affected by hypercalcemia.
Promote renal calcium excretion, facilitating calcium removal from the body.
Corticosteroid Therapy (Specific Tumors): Patients with HCM that is caused by steroid-responsive tumors may benefit from corticosteroid therapy. Corticosteroids can be particularly effective in lowering calcium levels in HCM associated with:
Certain hematological malignancies, such as multiple myeloma, lymphomas, or leukemias.
Steroid-responsive solid tumors (less common).
Corticosteroids help to reduce calcium levels through mechanisms such as decreasing intestinal calcium absorption and increasing urinary calcium excretion in these specific tumor types.
Symptom Management and Mobility: Management of HCM extends beyond calcium reduction to include comprehensive symptom management and supportive care. This involves:
Symptom Management: Addressing and alleviating symptoms directly caused by hypercalcemia, such as nausea, vomiting, constipation, fatigue, and neurological changes, improving patient comfort and well-being.
Bone Pain Management: Providing effective pain management for bone pain associated with hypercalcemia or bone metastases. This may include medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) for mild to moderate pain, and opioid analgesics for more severe bone pain, ensuring adequate pain relief.
Mobility Promotion: Implementing strategies to promote patient comfort and mobility, encouraging gentle activity and preventing complications of immobility, such as pressure ulcers and muscle weakness.
Constipation Management: Proactively assess patients for constipation, a common and often distressing symptom of hypercalcemia due to its effects on gastrointestinal motility. If constipation is present, implement appropriate measures to alleviate it, such as:
Increasing dietary fiber intake (if oral intake is appropriate).
Administering stool softeners or laxatives as prescribed to promote regular bowel movements and relieve constipation.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

