Integrated Management of Childhood Illnesses (IMCI)
Subtopic:
Assessing and Classification of a Sick Child

First, determine if this consultation is an initial visit or a follow-up appointment.
For a new (initial) visit, begin by asking: “What brought you and your child here today?” or “What is your child’s main concern?” (To understand the presenting problem).
Once you know the reason for the visit:
Evaluate for General Danger Signs.
A general danger sign indicates a serious health issue requiring immediate referral for specialized care. These signs point towards severe illness.
General Danger Signs Include:
Inability to Drink or Feed: The child cannot suckle or swallow fluids or nourishment.
Persistent Vomiting: The child regurgitates everything, unable to keep down any food or liquid.
Seizures: The child experiences convulsions (fits).
Lethargy or Unconsciousness: The child is unusually drowsy, difficult to rouse, or unresponsive.
Current Convulsions: The child is actively convulsing during the assessment.
After assessing danger signs, inquire about other key symptoms related to the child’s illness.
GENERAL DANGER SIGNS – Critical Indicators
General danger signs in young children (typically from 2 months up to 5 years old) are crucial alerts to potentially life-threatening conditions and must be addressed promptly. The World Health Organization (WHO) emphasizes these core danger signs:
Cannot Drink or Breastfeed: This refers to a child’s inability to effectively suck, drink, or swallow when offered breast milk or other fluids. This is a critical sign of weakness or serious illness.
Vomits Everything: This indicates that the child is rejecting all attempts at oral intake, including food, fluids, and medications, signifying a significant problem with tolerance and potential dehydration.
Convulsions (Fits or Seizures): Convulsions are characterized by involuntary stiffening or jerking movements of the arms and legs due to muscle contractions. The child may also lose awareness or not respond to verbal instructions.
Lethargic or Unconscious State: A lethargic child is excessively sleepy, lacks alertness, and shows no interest in their surroundings. They may not make eye contact or react to stimuli. An unconscious child is unarousable and does not respond to touch, shaking, or verbal commands.
IMMEDIATE ACTION REQUIRED: Any child exhibiting any General Danger Sign requires URGENT attention. Conduct a complete assessment, administer any necessary preliminary treatment immediately, and proceed with referral without delay.
Clarification of Danger Signs:
1. Not able to Drink or Breastfeed:
“Not able to drink or breastfeed” implies the child’s incapacity to suck or swallow when given fluids or breast milk.
Note: If there’s uncertainty about the mother’s response, directly offer the child clean water or breast milk to observe their ability to drink/feed.
2. Vomiting Everything:
“Vomiting everything” signifies:
The child cannot retain anything taken orally.
Everything ingested is immediately brought back up (regurgitated).
Note: If unsure about the mother’s answer, offer the child clean water or breast milk and observe if vomiting occurs.
3. Convulsions (Fits):
A convulsion is defined as any involuntary and uncontrolled movement of any part of the body.
This danger sign is present if there is a reported history of convulsions related to the current illness or if the child is convulsing during the examination.
A past history of convulsions is only relevant as a danger sign if the seizures occurred within the current episode of illness.
Use locally understood terms for convulsions, like “fits” or “spasms,” when communicating with caregivers.
4. Lethargic or Unconscious:
“Lethargic or unconscious” means:
The child is not fully awake and alert as expected for their age.
The child is excessively drowsy and disinterested in their environment.
The child might stare blankly, appearing unaware of their surroundings. or
An unconscious child cannot be awakened at all and shows no response to touch, shaking, or speech.
ASSESSMENT FOR GENERAL DANGER SIGNS – Practical Approach
| ASK | LOOK |
| – Is the child able to drink or breastfeed? | – Observe if the child appears lethargic or is unconscious. |
| – Does the child vomit everything? | – Is the child convulsing currently? If yes, initiate immediate management. |
| – Has the child experienced convulsions during this current illness? |
A child presenting with any general danger sign requires IMMEDIATE and focused attention. Complete the full assessment swiftly and provide any necessary pre-referral treatments without delay to ensure prompt referral and further management.
SIGNS, CLASSIFICATION, AND TREATMENT PROTOCOL
General Danger Signs: VERY SEVERE DISEASE
If any general danger sign is present, immediately classify the illness as a VERY SEVERE DISEASE requiring urgent intervention.
Emergency Pre-Referral Actions:
If Actively Convulsing: Administer diazepam immediately to manage seizures.
Expedited Assessment: Quickly finalize the complete child assessment.
Immediate Pre-Referral Treatment: Administer any necessary pre-referral treatments without delay.
Prevent Hypoglycemia: Take steps to prevent low blood sugar (hypoglycemia).
Maintain Body Temperature: Ensure the child is kept warm.
URGENT Referral: Refer the child to a higher level of care as a critical emergency.
Additional Screening: Consider screening for potential Tuberculosis (TB) and check for HIV risk factors.
NOTE: Actions in BOLD represent critical, urgent pre-referral treatments that must be initiated immediately.
Proceed to Main Symptom Assessment:
After addressing general danger signs, inquire about the Four Main Symptoms.
Four Key Symptom Areas:
The healthcare provider evaluating a sick child MUST systematically inquire about each of the following four main symptom areas:
Respiratory Issues: Cough or Difficult Breathing
Gastrointestinal Issues: Diarrhea
Elevated Temperature: Fever
Auditory Issues: Ear Problem
If any of these symptoms are reported as present, proceed with a more detailed assessment specific to that symptom area.

Cough or Difficult Breathing
Pneumonia is a major cause of mortality in children under the age of five globally. While most children presenting with a cough or breathing difficulties will have common, self-limiting conditions like a cold, it is crucial to identify the subset who may have pneumonia, a more serious respiratory infection.
ASSESSMENT OF COUGH AND BREATHING DIFFICULTY – ENSURE CHILD IS CALM DURING EXAMINATION
Inquire: “Does your child have a cough or is he/she having difficulty breathing?”
If YES, proceed with the following assessment: ASK, OBSERVE, LISTEN, FEEL
If Cough or Difficult Breathing is Present, ASK:
“How long has the cough or breathing difficulty been present?” (Duration of symptoms).
Observe, Listen, and Feel:
Respiratory Rate: Count the number of breaths per minute. Utilize respiratory rate timers if available to aid accuracy.
Chest Indrawing: Observe for chest in-drawing*.
Stridor: Listen for stridor** (a harsh, high-pitched sound).
Wheeze: Listen for wheezing*** (a musical, whistling sound).
Central Cyanosis: Check for bluish discoloration around the lips and face (central cyanosis).
Oxygen Saturation: Measure oxygen saturation using a pulse oximeter, if available.
AVPU Score: Assess level of consciousness using the AVPU scale****.
Wheezing Assessment (with Chest Indrawing or Fast Breathing): If wheezing is present alongside chest in-drawing or rapid breathing, evaluate for possible Asthma.
Wheezing Assessment (General): Assess for possible Tuberculosis (TB) disease if wheezing is noted.
Current Convulsions: Inquire “Is the child convulsing right now?” If yes, manage convulsions immediately.
Define Fast Breathing based on Age:
Children aged 2 months up to 12 months: Fast breathing is defined as 50 breaths per minute or higher.
Children aged 12 months up to 5 years: Fast breathing is defined as 40 breaths per minute or higher.
SIGNS, CLASSIFICATION, AND TREATMENT GUIDELINES
| SIGNS | CLASSIFICATION | TREATMENT |
| Any General Danger Sign OR any of the following: | VERY SEVERE DISEASE | • Administer diazepam immediately if the child is actively convulsing. • Conduct a rapid and thorough assessment. • Provide any essential pre-referral treatments without delay. • Manage to prevent low blood sugar. • Ensure the child is kept warm. • Administer the first oral dose of cotrimoxazole suspension. • Administer Vitamin A supplement. • Refer URGENTLY to a higher level healthcare facility. • Screen for potential TB and assess HIV risk factors. |
• Chest Indrawing in a calm child OR • Fast breathing AND • Absence of Very Severe Disease Signs | PNEUMONIA | • Prescribe Amoxicillin Dispersible Tablets. • Administer Vitamin A supplement. • Manage wheezing if present. If wheezing is present, schedule a follow-up within 2 days. • Recommend a safe and appropriate remedy to soothe the throat and alleviate cough symptoms. • Screen for potential TB and assess HIV risk factors. • If wheezing is noted (or resolves after a bronchodilator), administer an inhaled bronchodilator for 5 days. • If cough persists for over 14 days or recurrent wheezing is reported, refer for TB and/or asthma evaluation. • Re-assess in 2 days. If a 2-day review is not feasible, admit or refer children exhibiting chest in-drawing • Counsel the caregiver on when to seek immediate return to care. |
| Absence of Pneumonia or Very Severe Disease indicators. | NO PNEUMONIA: COUGH OR COLD | • Manage wheezing if present. If wheezing is present, schedule a follow-up within 2 days. • Recommend a safe and appropriate remedy to soothe the throat and alleviate cough symptoms. • Schedule a follow-up in 5 days if symptoms do not improve. • Screen for potential TB and assess HIV risk factors. • Counsel the caregiver on when to seek immediate return to care. |
Note: Treatments listed in BOLD represent critical, urgent pre-referral interventions.
Definitions of Clinical Signs:
Chest In-drawing: This occurs when the lower portion of the chest wall retracts or moves inwards during inhalation.
Stridor: A harsh, noisy, high-pitched sound that is audible primarily during inspiration (breathing in).
Wheeze: A musical, whistling sound usually heard during expiration (breathing out).
AVPU: A scale used to assess the level of consciousness: Alert, Responds to Voice, Responds to Pain, Unresponsive.

Diarrhea
Diarrhea is characterized by the excretion of three or more loose or watery stools within a 24-hour period. This condition is very common in children, particularly those between 6 months and 2 years old, representing a vulnerable age group.
It stands as the second most significant cause of death in children under five years of age globally. Dehydration resulting from diarrhea is the primary driver of mortality in these cases.
An episode of diarrhea is classified as acute if it lasts for less than 14 days. If diarrhea persists for 14 days or longer, it is considered persistent diarrhea.
The term dysentery is used when diarrhea is accompanied by blood in the stool, which may or may not include mucus.
It is important to distinguish true diarrhea from simply an increase in the frequency of normal, formed stools.
Initial Assessment for Diarrhea:
Inquire: “Does your child have diarrhea?”
If YES, proceed with ASK, OBSERVE, LISTEN, FEEL approach:
If Diarrhea is Present, ASK:
“How long has the diarrhea been going on?” (Duration of the diarrhea)
“Is there any blood in the stools?” (Assess for dysentery)
Clinical Examination:
General Condition Assessment:
Palpate Pulse: Check for a weak or absent pulse, which can indicate poor perfusion.
Assess Alertness: Evaluate the child’s level of consciousness using AVPU scale*, specifically checking if Alert (A) status is maintained.
Temperature and Peripheral Circulation: Assess for cold hands along with a temperature gradient (core body warmer than extremities), indicating poor circulation.
Capillary Refill Time: Test capillary refill time, noting if it is prolonged (greater than 3 seconds), suggesting dehydration and poor peripheral blood flow.
Dehydration Signs:
Level of Consciousness: Is the child lethargic or unconscious? (Severe Dehydration) Or Restless and irritable? (Moderate Dehydration)
Eyes: Observe for sunken eyes, a key indicator of fluid loss.
Fluid Intake Assessment: Offer the child fluids and observe:
Is the child unable to drink or drinking poorly? (Severe Dehydration)
Is the child drinking eagerly and appearing very thirsty? (Moderate Dehydration)
Skin Turgor: Pinch the skin on the abdomen to assess skin turgor (elasticity). Observe how quickly the skin fold returns to normal:
Very slowly (longer than 2 seconds)? (Severe Dehydration)
Slowly? (Moderate Dehydration)
Immediately? (No Dehydration)
Crucially, remember to systematically classify every child presenting with diarrhea specifically for the presence and severity of dehydration.
Classification and Treatment based on Dehydration Status
For DEHYDRATION
| SIGNS | CLASSIFICATION | TREATMENT |
All Four of the Following: • Weak or absent pulse • AVPU* score less than Alert (A) • Cold hands with temperature gradient • Capillary refill time greater than 3 seconds PLUS • Sunken eyes and very slow or slow skin pinch. | HYPOVOLEMIC SHOCK FROM DIARRHEA/DEHYDRATION | • INITIATE SHOCK MANAGEMENT. Administer Ringer’s Lactate solution at 20ml/kg intravenously as a bolus A second bolus may be necessary depending on the child’s response before proceeding to step 2 of PLAN C for dehydration management. • Treat and prevent hypoglycemia (low blood sugar). • Assess for severe acute malnutrition • Evaluate for severe anemia. Note: If Hemoglobin (Hb) is below 5g/dL, administer urgent blood transfusion. Admit to hospital or refer URGENTLY. • Screen for possible Tuberculosis (TB) and assess for HIV risk factors. • For children 2 years and older in areas with cholera outbreaks, administer oral cotrimoxazole for cholera prophylaxis and treatment. |
Two or More of the Following Signs: • Restless and irritable • Sunken eyes • Drinks eagerly, appears thirsty • Skin pinch returns slowly. | SOME DEHYDRATION | If the child ALSO has a severe classification (unrelated to dehydration): – Admit or refer URGENTLY to hospital, instructing the mother to give frequent small sips of Oral Rehydration Solution (ORS) during transport and to continue breastfeeding. OR If the child has NO other severe classifications: – Implement fluid and food therapy for some dehydration (following Plan B guidelines). – Provide Vitamin A supplementation.<br> – Administer ORS and Zinc Sulfate supplements. • Schedule a follow-up in 2 days if there’s no improvement. -Screen for potential TB and assess HIV risk factors. • Advise the mother on when to return immediately for worsening symptoms. |
| Not enough signs to classify as some or severe dehydration. | NO DEHYDRATION | If the child ALSO has a severe classification (unrelated to dehydration): – Admit or refer URGENTLY to hospital, instructing the mother to give frequent small sips of ORS during transport and to continue breastfeeding. OR If the child has NO other severe classifications: – Provide fluid and food therapy to manage diarrhea at home (following Plan A guidelines). – Provide Vitamin A supplementation. – Administer ORS and Zinc Sulfate supplements. • Schedule a follow-up in 5 days if there is no improvement. • Screen for potential TB and assess HIV risk factors. • Advise the mother on when to return immediately if symptoms worsen. |
Persistent Diarrhea Management (Diarrhea lasting 14 days or more)
| Condition | CLASSIFICATION | TREATMENT |
Dehydration Present (Hypovolemic shock, severe dehydration, or some dehydration). | SEVERE PERSISTENT DIARRHEA | • Manage hypovolemic shock and any form of dehydration before referral, unless the child has another co-existing severe classification that necessitates immediate referral for other reasons. • Provide Vitamin A supplementation. • Administer ORS and Zinc Sulfate supplements. • Prescribe Multivitamin and Mineral supplements.< • Admit to hospital or refer URGENTLY, instructing the mother to give frequent sips of ORS during transport and continue breastfeeding. • Screen for possible TB and assess HIV risk factors. |
| No Dehydration | PERSISTENT DIARRHEA | • Counsel the mother on appropriate feeding strategies for a child with persistent diarrhea. • Provide Vitamin A supplementation. • Administer ORS and Zinc Sulfate supplements. • Prescribe Multivitamin and Mineral supplements. • Check for HIV infection.<br> • Schedule a follow-up appointment in 5 days. • Screen for possible TB and assess HIV risk factors. |
Dysentery Management (Blood in Stool)
| Condition | CLASSIFICATION | TREATMENT |
| Blood in the stool. | DYSENTERY | • Treat with Ciprofloxacin.<br> • Provide Vitamin A supplementation. • Administer ORS and Zinc Sulfate supplements. • Schedule a follow-up appointment in 2 days. • Screen for possible TB and assess HIV risk factors. |

Fever
Fever is considered present if any of the following conditions are met:
Reported history of fever from the parent or caregiver.
The child feels unusually hot to the touch.
The child’s measured temperature is 37.5°C (99.5°F) or higher.
Fever in children can be an indicator of various illnesses, including malaria, measles, or other serious infections. Globally, malaria remains a significant cause of mortality in children under five. However, fever can also arise from common and less severe conditions such as colds, coughs, or other viral infections.
Effective classification and management of fever require understanding the local malaria risk level.
High Malaria Risk Areas: Regions where malaria accounts for more than 5% of fever cases in children.
Low Malaria Risk Areas: Regions where malaria accounts for 5% or less of fever cases in children.
Assessment Process for Fever:
Inquire: “Does your child have a fever? (Based on history, feeling hot, or temperature ≥ 37.5°C)”
IF YES:
“Has the child travelled in the past month to an area with high malaria risk (malaria-endemic zones, seasonal transmission areas, or epidemic-prone regions)?”
Determine the local Malaria Risk level: High or Low.
Utilize ASK, LOOK & FEEL approach:
THEN ASK:
“For how long has the fever been present?” (Duration of fever)
“If longer than 7 days, has the fever been present every day?” (Pattern of fever)
“Has the child shown any signs of measles in the last three months?” (Recent measles history)
LOOK AND FEEL:
Assess for nuchal rigidity: Look for or feel for a stiff neck.
Observe for nasal discharge: Look for a runny nose.
Evaluate for Measles Signs: Look for signs suggestive of MEASLES:
Generalized rash AND at least one of the following: cough, runny nose, or conjunctivitis (red eyes).
Investigate other potential fever causes: Consider and look for any other apparent reasons for the fever…
Malaria Testing Strategy based on Risk Level:
| Malaria Risk Level | Malaria Testing Recommendation | Areas Included |
| High Malaria Risk | Perform a malaria test for all febrile children. | • Endemic malaria zones • Seasonal malaria transmission zones • Epidemic-prone malaria areas |
| Low Malaria Risk | Perform a malaria test if there is no clear alternative explanation for the fever. Consider testing even if another cause seems likely to rule out malaria, especially in vulnerable populations or specific clinical contexts. | • Areas with low malaria prevalence • Regions where malaria transmission is infrequent or sporadic • Areas with effective malaria control programs that have significantly reduced local transmission |
Test Results Interpretation:
| Test Result | Interpretation |
| TEST POSITIVE | • Plasmodium falciparum PRESENT • Plasmodium vivax PRESENT |
| TEST NEGATIVE | • Plasmodium falciparum or Plasmodium vivax ABSENT |
NOTE: If malaria testing is unavailable, do not delay essential treatment. Clinical judgment should guide immediate management decisions.
SIGNS, CLASSIFICATION, AND TREATMENT GUIDELINES for Fever
| SIGNS | CLASSIFICATION | TREATMENT |
• Any general danger sign OR • Stiff neck AND • Confirmed malaria positive test. | VERY SEVERE FEBRILE DISEASE OR SEVERE MALARIA | • Administer the first dose of artesunate or quinine for severe malaria. • Give the first dose of a suitable antibiotic (e.g., Ceftriaxone first dose). • Manage to prevent hypoglycemia (low blood sugar). • Administer a single dose of paracetamol in the clinic for high fever (≥38.5 °C/ 101.3°F). • Admit to hospital or Refer URGENTLY. • Screen for possible TB disease and assess HIV risk factors. |
| • Malaria test POSITIVE** | UNCOMPLICATED MALARIA | • Administer the recommended first-line oral antimalarial medication. • Administer Artemether + Lumefantrine (AL) as first line. • Administer a single dose of paracetamol in the clinic for high fever (≥38.5 °C/ 101.3°F). • Provide appropriate antibiotic treatment if a bacterial cause for the fever is identified. • Give Vitamin A supplement.<br> • Schedule a follow-up appointment in 3 days if fever persists. • If fever has been present daily for more than 7 days, conduct further assessment or refer. • Screen for possible TB disease and assess HIV risk factors.<br> • Advise caregiver on when to return immediately. |
| • Malaria test NEGATIVE | FEVER: NO MALARIA | • Administer a single dose of paracetamol in the clinic for high fever (≥38.5 °C/ 101.3°F). • Evaluate for other potential causes of the fever. • Schedule a follow-up appointment in 3 days if fever persists. • If fever has been daily for more than 7 days, perform further assessment or refer. • Screen for possible TB disease and assess HIV risk factors.<br> • Advise caregiver on when to return immediately. |
CHECK FOR MEASLES COMPLICATIONS
If the child currently exhibits signs of measles or has had measles within the last 3 months:
Oral Ulcers: Look for mouth ulcers; assess if they are deep or extensive.
Ocular Discharge: Look for pus draining from the eye(s).
Corneal Clouding: Look for clouding of the cornea (the clear front part of the eye).
SIGNS, CLASSIFICATION, AND TREATMENT for Measles Complications
| SIGNS | CLASSIFICATION | TREATMENT |
| Generalized rash characteristic of measles <br> AND <br> • At least one of: cough, runny nose, or red eyes | SUSPECTED MEASLES | • Give Vitamin A supplement (refer to protocol on page 14 for dosage).<br> • Report the case and obtain a blood sample for measles confirmation.<br> • Screen for possible TB disease and assess HIV risk factors.<br> • Advise caregiver on when to return immediately if the child’s condition worsens. |
| Any general danger sign <br> OR <br> • Corneal clouding <br> OR <br> • Deep or extensive mouth ulcers. | SEVERE COMPLICATIONS OF MEASLES | • Give Vitamin A supplement.<br> • Administer the first dose of Ceftriaxone antibiotic.<br> • If corneal clouding or pus draining from the eye is present, apply tetracycline eye ointment.<br> • Report the case and obtain a blood sample for confirmation OR refer immediately.<br> • Admit to hospital or Refer URGENTLY.<br> • Screen for possible TB disease and assess HIV risk factors. |
| • Pus draining from the eye <br> OR <br> • Mouth ulcers (not deep or extensive). | EYE OR MOUTH COMPLICATIONS OF MEASLES | • Give Vitamin A supplement.<br> • If pus is draining from the eye, treat eye infection with tetracycline eye ointment.<br> • If mouth ulcers are present, treat with nystatin (antifungal medication).<br> • Schedule a follow-up appointment in 2 days.<br> • If the child does not require referral, report the case and collect a blood sample for measles confirmation.<br> • Screen for possible TB disease and assess HIV risk factors. |
| • No pus draining from the eye <br> OR <br> No mouth ulcers. | NO EYE OR MOUTH COMPLICATIONS OF MEASLES | • Give Vitamin A supplement if not received in the past month.<br> • If the child does not require referral, collect blood sample for measles confirmation.<br> • Screen for possible TB disease immediately following the measles infection and assess HIV risk factors. |

Ear problem
Ear problems in children frequently involve ear infections.
An ear infection can lead to pus accumulation in the space behind the eardrum. This buildup of pressure often causes pain and may be accompanied by fever.
If left untreated, the eardrum can rupture, resulting in pus discharge and a temporary reduction in pain. However, even after eardrum rupture, there is a risk of long-term consequences such as impaired hearing or, in severe cases, permanent deafness. Untreated ear infections can also spread, potentially leading to serious complications like mastoiditis (infection of the mastoid bone behind the ear) or meningitis (infection of the membranes surrounding the brain and spinal cord).
Assessment of Ear Problems:
Inquire: “Does your child have an ear problem?”
If YES, proceed with ASK, LOOK, and FEEL examination:
If an Ear Problem is Reported, ASK:
“Is your child experiencing ear pain?” (Presence of otalgia)
“Is there any discharge coming from the ear?” (Presence of otorrhea). If yes, “For how long has the discharge been present?” (Duration of discharge)
LOOK and FEEL:
Examine for Ear Discharge: Visually inspect the ear for any pus draining from the ear canal.
Palpate for Mastoid Tenderness: Gently feel the area behind the ear to check for tender swelling, which could indicate mastoiditis.
Classification and Treatment of EAR PROBLEMS
| SIGNS | CLASSIFICATION | TREATMENT |
| • Tender swelling behind the ear. | MASTOIDITIS | • Administer the first dose of Ceftriaxone Antibiotic. • Give the first dose of paracetamol for pain relief. • Refer URGENTLY to hospital or admit for inpatient care. • Assess for HIV risk factors. |
• Pus observed draining from the ear OR • Ear discharge reported for less than 14 days, OR • Ear pain (otalgia). | ACUTE EAR INFECTION | • Prescribe Amoxicillin dispersible tablets for a 5-day course. • Administer paracetamol for pain management. • Dry the ear canal using a wicking technique • Assess for HIV risk factors. • Schedule a follow-up appointment in 5 days. |
• Pus observed draining from the ear OR • Ear discharge reported for 14 days or more (chronic discharge). | CHRONIC EAR INFECTION | • Dry the ear canal using a wicking technique. • Assess for HIV risk factors. • Schedule a follow-up appointment in 5 days. |
• No ear pain AND • No pus seen or reported draining from the ear. | NO EAR INFECTION | No specific treatment indicated. |
ASSESS FOR MALNUTRITION
ASK
Inquire about prior Tuberculosis (TB) exposure history.
LOOK AND FEEL
Examine for swelling in both feet (pedal edema).
Evaluate the child’s weight in relation to their height/length (WFH/L) and plot it on growth charts to determine the Z-score.
Analyze the child’s growth pattern for flattening or decline over at least two consecutive months.
Measure Mid-Upper Arm Circumference (MUAC) in millimeters for children 6 months or older.
If WFH/L is below -3 Z-score or MUAC is less than 115mm, proceed with further assessment.
Determine if any medical complexities are present:
Note any general danger indicators.
Identify any severe classification.
Observe for chest indrawing indicative of pneumonia.
If no medical complications are identified:
Perform an appetite test.
If the child is 6 months or older, offer Ready-to-Use Therapeutic Food (RUTF).
Assess if the child is able to finish the RUTF portion.
If the child can finish RUTF, assess breastfeeding practices.
For children under 6 months, evaluate breastfeeding challenges.
If the child has acute Malnutrition and is currently receiving RUTF, avoid administering additional iron supplements as RUTF already contains sufficient iron.
Classify Malnutrition
| SIGNS SEVERE ACUTE MALNUTRITION WITH COMPLICATIONS FOR CHILDREN
SIGNS:
Presence of edema in both feet.
OR Weight-for-Height/Length Z-score is less than -3.
OR MUAC measurement is less than 11.5 cm and ANY of the following are present:
Medical complication requiring treatment.
Inability to finish a standard portion of RUTF.
Breastfeeding challenges (for infants under 6 months).
TREATMENT:
Address potential hypoglycemia immediately.
Ensure the child is kept warm.
Administer the initial dose of Benzylpenicillin and Gentamicin.
Provide Vitamin A supplementation.
URGENTLY refer to a hospital.
Hospital admission is necessary if the child has any other complications (e.g., danger signs like diarrhea, pneumonia, fever, lack of appetite).
Immunize according to the recommended schedule.
Screen for possible TB infection and HIV.
SEVERE ACUTE MALNUTRITION
SIGNS:
Visible severe wasting.
OR Presence of edema in both feet.
OR Z-score of less than -3 (Weight-for-age or Weight-for-height/Length). For children aged 6-59 months.
OR MUAC measurement less than 11.5 cm.
AND Child is able to finish RUTF.
TREATMENT:
Administer oral Amoxicillin DT for 5 days.
Provide Ready-to-Use Therapeutic Food (RUTF) specifically formulated for children aged six months and older.
Screen for TB and HIV.
Schedule a follow-up appointment in 7 days.
Evaluate the child’s feeding practices and provide counseling to the mother on feeding recommendations.
Immunize based on the schedule.
Advise the mother about when to return immediately if needed.
MODERATE ACUTE MALNUTRITION
SIGNS:
Static weight or weight loss observed.
Z-score between -3 and less than -2.
For children aged 6 months up to 59 months, MUAC ranges from 11.5 to 12.5 cm.
TREATMENT:
If growth faltering is noted for two consecutive months, administer Vitamin A supplementation and consider further assessment or referral to a hospital.
Evaluate the child’s feeding practices and provide counseling to the mother on feeding recommendations.
Administer Albendazole if the child is 1 year or older and has not received a dose within the last 6 months.
For feeding problems, schedule a follow-up in 14 days.
Screen for TB and HIV.
Immunize as per schedule.
Advise the mother about when to return immediately.
AT RISK OF ACUTE MALNUTRITION
SIGNS:
Static weight or weight loss observed.
Z-score between -2 and less than -1.
For children aged 6 months up to 59 months, MUAC ranges from 12.5 to 13.5 cm.
TREATMENT:
If the child is under 2 years old and experiencing growth faltering, assess feeding practices and counsel the mother on feeding recommendations according to guidelines.
Administer Albendazole if the child is 1 year or older and hasn’t had a dose in the previous 6 months.
Schedule a follow-up in 14 days.
If feeding problems persist, follow up in 5 days.
Screen for TB and HIV.
Immunize as per schedule.
Advise the mother about when to return immediately.
NO ACUTE MALNUTRITION
SIGNS:
Weight-for-Height/Length Z-scores between -1 and +2.
OR MUAC measurement is greater than 13.5 cm.
TREATMENT:
If the child is under 2 years old, assess feeding practices and counsel the mother on feeding recommendations.
For feeding problems, schedule a follow-up in 5 days.
Administer Albendazole if the child is 12 months or older and hasn’t had a dose in the previous 6 months.
Immunize as per schedule.
Screen for TB and HIV.
THEN CHECK FOR ACUTE MALNUTRITION
Optimal nutrition arises from sufficient consumption of macronutrients, micronutrients, and water. These are crucial for supporting the body’s metabolic activities, encompassing both building up (anabolism) and breaking down (catabolism) processes.
Components of Nutrition:
Macronutrients: These are the major nutrients required in large amounts, such as carbohydrates, proteins, and fats, providing energy and building blocks for the body.
Micronutrients: These are essential nutrients needed in smaller quantities, including vitamins and minerals, vital for various bodily functions and overall health.
What is Malnutrition?
Malnutrition is a condition that develops when the body does not receive the correct proportion of nutrients. This includes both undernutrition, where there is a deficiency of necessary nutrients, and overnutrition, where there is an excessive intake of nutrients.
Deficiencies in either macro or micronutrients can impede proper development, result in inadequate physical growth, or cause body wasting.
The effects of malnutrition are often evaluated through anthropometric measurements, which include assessments like weight-for-age, height-for-age, and weight-for-height to determine physical status.
Undernutrition represents the more prevalent form of malnutrition, particularly observed within developing countries.
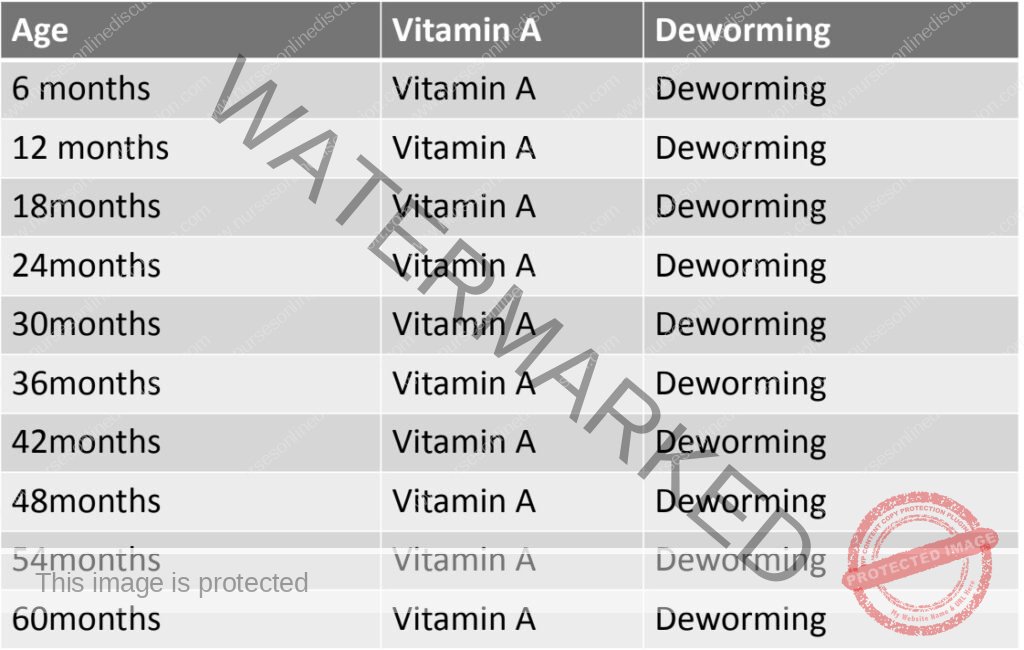
CHECK THE CHILD’S IMMUNIZATION, VITAMIN A & DEWORMING STATUS
Immunization Status:
Highly Effective Intervention: Vaccination is a very efficient and cost-effective public health measure for controlling and preventing infectious diseases, especially in young children.
Target Population: Vaccination programs primarily focus on children under 5 years of age, as they are most vulnerable to vaccine-preventable illnesses.
Resource Intensive: Successful immunization programs require significant resources, planning, and dedicated effort for effective implementation and outreach.
Strategies for Enhancing Immunization Coverage:
Routine Immunization Services: Consistent and readily available vaccination services provided at regular health facilities.
Supplementary Immunization Activities (SIAs): Periodic campaigns to reach wider populations, often used to boost coverage or introduce new vaccines.
Disease Surveillance: Systematic monitoring of targeted diseases to track trends and identify areas with low immunization rates.
“Mopping Up” Campaigns: Focused efforts in high-risk or under-immunized areas to ensure no child is missed, particularly after outbreaks or in areas with persistently low coverage.
Vitamin A Status:
Essential for Child Health: Vitamin A is crucial for numerous bodily functions in children, playing a vital role in:
Growth and Development: Supporting normal physical growth and maturation.
Infection Protection: Strengthening the body’s defense mechanisms against infections and enhancing overall immunity.
Causes of Vitamin A Deficiency: Vitamin A deficiency can arise due to:
Inadequate Dietary Intake: Insufficient consumption of foods naturally rich in Vitamin A, like liver, eggs, and orange/yellow fruits and vegetables.
Impaired Absorption: Conditions affecting nutrient absorption in the gut can reduce Vitamin A uptake from food.
Increased Utilization During Illness: The body’s Vitamin A stores can be rapidly depleted during infections and illnesses, increasing the risk of deficiency.
Consequences of Vitamin A Deficiency: Lack of sufficient Vitamin A can lead to several adverse health outcomes:
Increased Susceptibility to Illness: Weakened immunity results in a higher chance of getting sick more frequently.
Delayed Recovery: The body’s ability to fight off infections is compromised, leading to longer illness durations and slower recovery.
Eye Problems and Blindness: Severe Vitamin A deficiency is a leading cause of preventable childhood blindness, starting with night blindness and potentially progressing to irreversible damage.
Elevated Mortality Risk: Vitamin A deficiency significantly increases the risk of death from common childhood illnesses, making supplementation a life-saving intervention.
Benefits of Vitamin A Supplementation: Providing Vitamin A supplements has proven to significantly reduce childhood morbidity and mortality:
Measles Mortality Reduction: Can decrease deaths from measles by approximately 50%.
Diarrheal Disease Mortality Reduction: Reduces mortality associated with diarrhea by roughly 33%.
Overall Mortality Reduction: Leads to a significant decrease in death from all causes in children by about 23%.
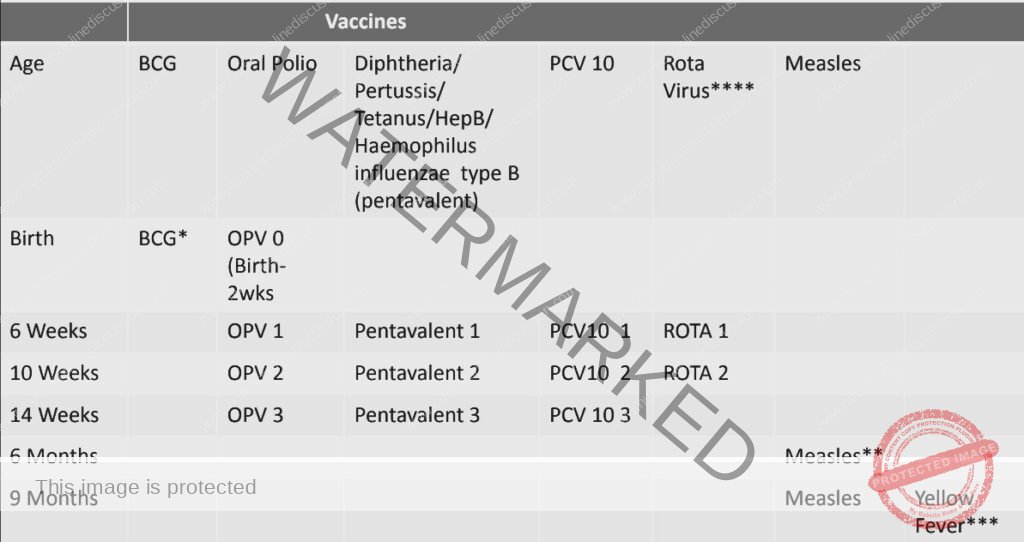
BCG Vaccine: If the Bacillus Calmette-Guérin (BCG) vaccine, which protects against tuberculosis, is not administered at birth, it is contraindicated for children who are displaying symptoms of HIV/AIDS.
Measles Vaccination at 6 Months: A measles vaccine dose at 6 months of age is specifically recommended for infants who are either HIV-exposed or HIV-infected. This is an early dose in addition to the standard schedule to provide earlier protection in vulnerable children.
Yellow Fever Vaccine: The Yellow Fever vaccine is contraindicated for children exhibiting symptoms of HIV/AIDS due to the risk of adverse events in immunocompromised individuals.
Rotavirus Vaccine Age Limit: The Rotavirus vaccine series, used to prevent severe diarrheal disease, should not be initiated in children who are 15 months of age or older. The first dose should ideally be given before 15 weeks of age, and the series completed by 8
ASSESS OTHER POTENTIAL HEALTH CONCERNS
It is important to recognize that the IMCI (Integrated Management of Childhood Illness) case management approach, while comprehensive, has inherent limitations:
Scope is not Exhaustive: The IMCI guidelines, as reviewed here, do not encompass every possible symptom or pediatric condition a child might present with.
Not a Complete Pediatric Textbook: This process is a focused guide for managing common childhood illnesses and is not intended to be a comprehensive overview of all pediatric medical knowledge.
Address Caregiver Concerns and Observed Issues:
It’s crucial to actively listen to and address any additional concerns raised by the child’s caregiver. For example, if the caregiver mentions that the child has persistent itchy skin, this needs attention beyond the core IMCI symptoms. Similarly, be observant during the examination for any problems the caregiver may not have explicitly mentioned, such as visible jiggers or other skin conditions.
Management and Referral of Additional Problems:
Treat Based on Competence: Manage any other identified health issues according to your professional training, clinical expertise, and established clinic protocols and guidelines.
Referral for Complex Issues: If you encounter any problem that falls outside your scope of practice or the clinic’s capabilities, ensure appropriate referral to a higher level of care or a specialist for further evaluation and management.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

