Eye Conditions
Subtopic:
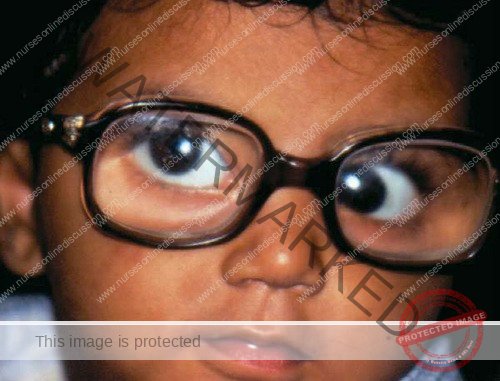
Congenital cataracts
Congenital cataracts are a form of cataract present at birth or developing within the first year of a baby’s life. They are defined by a clouding or opacity that affects the lens of the eye.
The lens itself is a crucial, clear tissue within the eye. Its primary function is to focus light onto the retina, enabling clear vision.
The severity of congenital cataracts can vary considerably. Some lens opacities may be minor and non-progressive, having negligible impact on vision. Conversely, other congenital cataracts can be visually significant, causing substantial visual impairment.
Therefore, congenital cataracts can be further described based on several characteristics:
Visual Significance:
Visually Significant: Impairing vision.
Not Visually Significant: Having little to no effect on sight.
Progression:
Stable: Remaining unchanged over time.
Progressive: Worsening or increasing in opacity.
Onset:
Congenital: Present at birth.
Acquired: Developing after birth.
Laterality:
Unilateral: Affecting only one eye.
Bilateral: Affecting both eyes.
Extent:
Partial: Involving only a portion of the lens.
Complete: Encompassing the entire lens.

Classifications of Congenital Cataracts
Congenital cataracts can be categorized using different criteria, including their morphology, the age at which they appear, and their underlying causes.
Morphology: Based on Physical Appearance
Classification by morphology refers to categorizing congenital cataracts according to their visual characteristics and structure.

Polar Cataract:
Polar cataracts are a type of lens opacity that affects the subcapsular cortex and lens capsule at either the anterior or posterior pole of the lens. These cataracts are characterized by their location at the front (anterior) or back (posterior) “poles” of the lens structure.
Anterior Polar Cataracts: These typically manifest as:
Small size: Often relatively small in diameter.
Bilateral occurrence: Frequently present in both eyes.
Symmetrical presentation: Similar appearance and size in each eye.
Non-progressive nature: Tend not to worsen or enlarge over time.
Visually insignificant: Usually do not cause noticeable vision problems due to their small size and location.
Posterior Polar Cataracts: In contrast to anterior polar cataracts, posterior polar cataracts:
Greater Visual Impact: Generally lead to more significant visual impairment.
Larger Size Tendency: Often tend to be larger in size compared to anterior polar cataracts.
Proximity to Nodal Point: Their location closer to the nodal point of the eye (the optical center of the eye’s focusing system) makes them more disruptive to light transmission and image formation on the retina, hence causing greater visual disturbance.
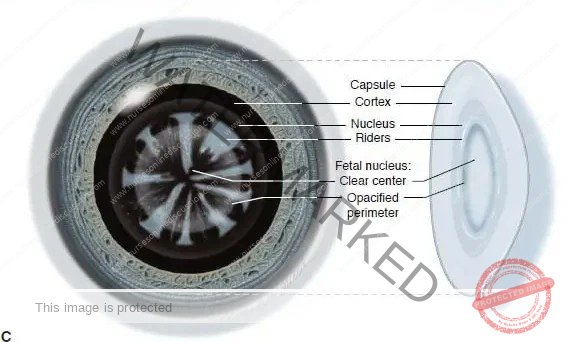
Lamellar Cataract/Zonular Cataract: Lamellar cataracts are the most common type of congenital cataracts.
The cataract is visible as an horseshoe- shaped opacity that surrounds a clearer center and is itself
surrounded by a layer of clear cortex. Lamellar cataracts may be inherited or result from a transient toxic
influence during embryonic lens development.
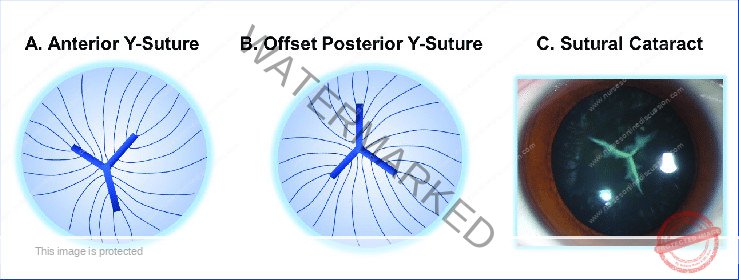
Sutural Cataract: Opacification of the Y-sutures of the fetal nucleus that commonly do not impair vision. They
are usually bilateral, symmetric, and frequently inherited in an autosomal dominant pattern. These opacities
often have branches or knobs projecting from them

Coronary Cataract: Coronary cataracts consist of club-shaped cortical opacities arranged around the equator
of the lens like a crown or corona. They cannot be seen unless the pupil is dilated, and they usually do not
affect visual acuity. They are often inherited in an autosomal dominant pattern.

Cerulean Cataract/Blue-dot Cataract: Cerulean cataracts are small bluish opacities located in the lens cortex.
They are nonprogressive and usually do not cause visual symptoms
Nuclear Cataract: Opacities of either the embryonic nucleus alone or both the embryonic and fetal nuclei. They
are usually bilateral, with a wide spectrum of severity. Eyes with congenital nuclear cataracts tend to be
microphthalmic and have an increased risk of developing aphakic glaucoma.
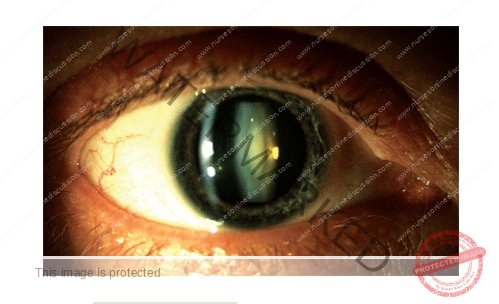
Capsular Cataract: Small opacifications of the lens epithelium and anterior lens capsule that spare the cortex.
They are differentiated from anterior polar cataracts by their protrusion into the anterior chamber, but generally
do not affect vision.

Membranous Cataract: Membranous cataracts occur when lens proteins are resorbed, allowing the anterior
and posterior lens capsules to fuse into a dense white membrane. They cause significant visual disability due
to the resulting opacity and lens distortion.
Age of Onset:
Congenital/Infantile Cataract: Lens opacities present at birth.
Acquired/Juvenile Cataract: Onset occurring after infancy, during childhood.
Etiology (Causes):
Genetic/Hereditary Cataract:
Caused by genetic mutations affecting lens structure or clarity.
Individuals are typically otherwise healthy, without systemic illness.
May be associated with microphthalmos (abnormally small eyes).
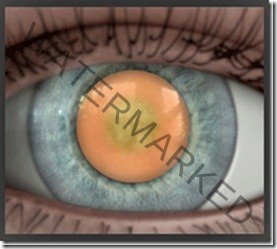
Metabolic Cataract:
Caused by metabolic disorders such as galactosemia, hypoglycemia, hypocalcemia.
Galactosemia-related: Presents with characteristic ‘oil droplet’ cataracts, reversible upon dietary galactose restriction (dairy removal).
Traumatic Cataract:
Caused by external eye injuries.
Trauma is the most frequent cause of unilateral cataract in children.
Typically results from penetrating injury, but blunt trauma can also induce cataract formation.
Secondary Cataracts (Maternal Infection-Related):
Secondary to maternal infections contracted during pregnancy, particularly TORCH infections:
Toxoplasmosis
Others (Syphilis, Hepatitis B)
Rubella
Cytomegalovirus (CMV)
Herpes simplex virus infection
Usually bilateral, dense, and centrally located.
Rubella is the most common maternal infection causing congenital cataracts. Rubella-related cataracts can be present at birth or develop later in infancy.
Iatrogenic Cataract:
Caused by medical treatments.
Examples include Radiation therapy, certain Drugs (e.g., long-term systemic steroids), and Surgical complications.
Commonly seen in older children who have undergone Total Body Irradiation for leukemia, organ transplantation, or long-term systemic steroid therapy. Prognosis after cataract surgery is generally good in these cases.

Causes of Congenital Cataracts
The origins of congenital cataracts are diverse and can involve a combination of factors. These include hereditary predispositions, prenatal infections, physical trauma during pregnancy, metabolic imbalances, and premature birth. In numerous instances, pinpointing the precise cause of congenital cataracts remains undetermined.
Genetic Predisposition: Inherited genetic anomalies are implicated in a significant proportion of congenital cataract cases. It’s estimated that approximately 20% of individuals with congenital cataracts have a family history of the condition, suggesting a familial or hereditary link. These cataracts arise from gene mutations that disrupt the normal development and transparency of the lens.
Prenatal Infections: Certain maternal infections contracted during pregnancy are known to elevate the risk of congenital cataracts in infants. These infections are often categorized under the acronym STORCH (and sometimes TORCH), which includes:
STORCH Complex:
Syphilis
Toxoplasmosis
Rubella
Cytomegalovirus (CMV)
Herpes simplex virus
Other Infections: Additional infections beyond STORCH that have been linked to congenital cataracts include:
Influenza (flu)
Measles
Polio
Rubella (covered in STORCH but listed again for emphasis)
Associated Conditions: Several other conditions can contribute to the development of congenital cataracts:
Hypoparathyroidism (underactive parathyroid glands)
Conradi-Hünermann syndrome (a rare genetic disorder)
Aniridia (absence of the iris)
Anterior segment dysgenesis (abnormal development of the front part of the eye)
Persistent fetal vasculature (PFV) – remnants of fetal blood vessels in the eye
Posterior lenticonus (abnormal bulging of the back surface of the lens)
Maternal corticosteroid use (certain medications taken during pregnancy)
Physical Trauma During Gestation: Physical injury to the mother’s abdomen during pregnancy can, in rare cases, result in trauma to the developing baby’s eyes in utero, potentially leading to congenital cataracts. Such trauma may be caused by events like:
Motor vehicle accidents
Falls
Domestic violence or intimate partner violence
Maternal Hypoglycemia: Episodes of hypoglycemia (low blood sugar) in pregnant women, particularly those with poorly controlled diabetes, have been associated with an increased risk of congenital cataracts in their offspring.
Prematurity: Infants born prematurely, before 37 weeks of gestation, exhibit a higher incidence of congenital cataracts compared to full-term infants.
Metabolic Disorders: Certain inherited metabolic disorders can disrupt lens metabolism and increase the risk of cataract formation from birth, including:
Galactosemia
Hypoglycemia
Syndromes: Congenital cataracts are a recognized feature of several genetic syndromes, including:
Down syndrome (Trisomy 21)
Lowe syndrome (oculo-cerebro-renal syndrome)
Cockayne syndrome
Marfan syndrome
Trisomy 13-15 (Patau syndrome and Edwards syndrome)
Alport syndrome
Myotonic dystrophy
Fabry disease
Incontinentia pigmenti
Diagnosis and Investigations for Congenital Cataracts:
Diagnosis of congenital cataracts requires a thorough ophthalmological evaluation performed by an eye specialist (ophthalmologist).
While extensive testing isn’t always necessary, a detailed patient history is often more informative than numerous investigations in diagnosing congenital cataracts.
Family History and Genetic Evaluation:
Detailed Family History: Obtaining a comprehensive family history is crucial, given the potential for genetic inheritance in congenital cataracts.
Genetic Testing: Genetic testing may be recommended in certain cases to pinpoint specific gene mutations linked to cataract development, particularly when a hereditary cause is suspected.
Comprehensive Eye Examination: A complete eye exam is essential for diagnosis and characterization of congenital cataracts:
Visual Acuity Assessment: Evaluating the infant’s or child’s visual acuity, even if subjective in very young children.
Lens Examination: Careful examination of the lens to directly visualize and characterize the cataract.
Red Reflex Assessment: Evaluation of the red reflex is a critical screening tool, particularly for infants.
Estimating Cataract Size and Location: The red reflex test helps estimate the size and position of the cataract, especially if it obstructs the visual axis.
Darkened Room: The red reflex test is optimally performed in a darkened room to enhance visibility.
Direct Ophthalmoscope Technique: Involves shining a bright light from a direct ophthalmoscope into both eyes simultaneously from a distance of 1-2 feet to observe the red reflex and detect any opacities.
Slit Lamp Examination: A slit lamp biomicroscope is used for detailed anterior segment examination:
Detailed Eye Structure Visualization: A slit lamp provides a magnified, three-dimensional view of the eye’s structures.
Cataract Characterization: Crucial for visualizing the cataract in detail and determining its:
Size
Location within the lens
Morphology (shape and characteristics).
Intraocular Pressure (IOP) Measurement: Tonometry to measure intraocular pressure is performed to:
Assess for glaucoma or other conditions affecting eye pressure.
Rule out other potential ocular issues.
Ultrasound of the Posterior Pole: B-scan ultrasonography is used when lens opacity obscures direct visualization:
Visualization of Posterior Segment: Used when dense cataracts prevent clear visualization of the posterior segment of the eye (retina, optic nerve).
Rule Out Posterior Pole Abnormalities: Helps to assess for any additional abnormalities or structural issues in the back of the eye.
Laboratory Investigations: Laboratory tests may be indicated depending on clinical findings and suspected underlying causes:
TORCH Screening: Blood tests to screen for TORCH infections (Toxoplasmosis, Rubella, Cytomegalovirus, Herpes simplex, and sometimes others like Syphilis).
VDRL Test: Venereal Disease Research Laboratory test to screen for congenital syphilis.
Metabolic Blood Tests: Blood tests to evaluate for metabolic disorders, including:
Serum calcium levels (for hypocalcemia).
Serum phosphorus levels.
Blood glucose levels (for hypoglycemia/hyperglycemia).
Galactokinase levels (enzyme assay for galactosemia).
Urine Tests for Reducing Sugars: Urine tests to screen for reducing sugars, which can indicate galactosemia and other metabolic disorders.
Management of Congenital Cataracts
The treatment and care for congenital cataracts necessitates a comprehensive, multidisciplinary approach, tailored to each child’s unique circumstances and the underlying cause of the cataracts.
Aims of Management
The overarching goals of managing congenital cataracts are:
Lens Opacity Removal & Vision Restoration: To surgically remove the clouded lens and restore clear vision in the affected eye(s), allowing for proper visual input.
Cognitive Development: To facilitate the child’s attainment of typical cognitive development milestones, which can be affected by visual impairment.
Sensory Awareness: To ensure the child recognizes and responds appropriately to their sensory needs, especially visual input.
Injury Prevention: To minimize the risk of accidental injury due to impaired vision and coordination.
Anxiety Reduction: To lessen anxiety and distress in both the child and family related to the condition and its management, providing reassurance and support.
Education for Adaptive Living: To provide thorough education and training to the child and family on strategies to cope with altered visual abilities and maximize functional independence.
Generally, early intervention is crucial, especially for younger children, to mitigate the risk of amblyopia (lazy eye).
For optimal visual development in infants, it is generally recommended that:
Visually significant unilateral congenital cataracts be detected and surgically removed before 6 weeks of age.
Visually significant bilateral congenital cataracts should ideally be removed before 10 weeks of age.
However, some congenital cataracts are too small to impede vision. In such cases:
No immediate surgery or treatment is necessary.
If the cataracts are superficial and minor, an ophthalmologist will monitor them throughout the patient’s life to detect any changes or progression.
Patients with small, non-visually significant congenital cataracts may, in many cases, develop visually significant cataracts later in adulthood, often decades later.
Congenital cataracts are a significant cause of visual impairment in infancy, but also one of the most treatable, with an estimated prevalence of 1 to 6 cases per 10,000 live births.
Nursing Assessment:
Recent Medication Review: Inquire about the patient’s recent medication intake, as anticoagulant therapy may need to be temporarily discontinued before surgery to minimize the risk of bleeding behind the eye (retrobulbar hemorrhage).
Preoperative Testing Review: Check for completion and results of standard preoperative tests, which may be ordered based on the patient’s overall health and medical history. These tests can include:
Complete blood count (CBC)
Electrocardiogram (ECG)
Urinalysis
Vital Signs Monitoring: Confirm stable vital signs (temperature, pulse, respiration, blood pressure) prior to surgery, ensuring the patient is medically fit for the procedure.
Visual Acuity Test Results: Review the results of visual acuity tests, such as Snellen’s chart (for older children), to establish a baseline and understand the extent of visual impairment.
Patient Medical History: Thoroughly assess the patient’s medical history to identify any pre-existing conditions or factors that may influence preoperative testing requirements or surgical planning.
Nursing Diagnoses:
Based on the assessment, relevant nursing diagnoses may include:
Disturbed Visual Sensory Perception: Related to altered sensory reception or changes in sensory organ status, as evidenced by the patient using hands to explore or locate objects in their environment.
Risk for Trauma: Related to compromised vision and reduced hand-eye coordination, increasing the likelihood of accidental injuries.
Anxiety: Related to the potential for permanent vision loss or dependence, as evidenced by patient restlessness and expressed concerns about vision.
Medical Management: Pharmacologic Therapy:
Pupil Dilating Drops: Administered both before and after surgery to:
Dilate the pupil (mydriasis), facilitating surgical access to the lens.
Reduce postoperative inflammation and discomfort.
Antibiotic Medications: Administered prophylactically to:
Prevent postoperative infection, a potential complication of eye surgery.
Minimize inflammation within the eye following surgery.
Intravenous (IV) Sedation: Sedation may be used preoperatively to:
Reduce patient anxiety and apprehension before surgery.
Minimize discomfort associated with preoperative procedures, especially in young children.
Surgical Intervention:
Surgery as Primary Treatment: Surgery is the fundamental and most effective treatment for congenital cataracts that are visually significant.
Pediatric Ophthalmologist Expertise: The surgical procedure is typically performed by pediatric ophthalmologists, who have specialized training and experience in cataract surgery in children.
Cataract Removal Procedure: During surgery:
A small surgical incision is carefully made in the eye.
The cloudy lens (cataract) is meticulously removed from the eye.
Additional Procedures (Possible): In certain cases, depending on the specific needs of the child and the surgical approach, additional procedures may be required, such as:
Intraocular lens (IOL) implantation at the time of cataract removal.
Capsulotomy (creating an opening in the lens capsule) to improve visual axis clarity.
Lens Replacement Options:
Various lens replacement options are available after cataract removal, each with advantages and considerations:
Phacoemulsification: This common technique involves:
Removing a portion of the anterior lens capsule (anterior capsulotomy).
Using ultrasound energy to emulsify and aspirate the lens nucleus and cortex (the cloudy part of the cataract).
Leaving the posterior lens capsule and zonular support structures intact.
Lens replacement options following phacoemulsification include:
Aphakic glasses: Thick eyeglasses to correct vision without a lens.
Contact lenses: Custom-fitted contact lenses for visual correction.
Intraocular lens (IOL) implants: Artificial lenses surgically implanted in the eye to restore focusing power.
Extracapsular Cataract Extraction (ECCE): A surgical technique where:
The anterior lens capsule is removed.
The lens nucleus and cortex are extracted from the eye.
The posterior lens capsule is intentionally left intact, providing support for potential IOL implantation.
Intracapsular Cataract Extraction (ICCE): An older technique, less commonly used now, where:
The entire lens, including its intact capsule, is surgically removed.
Timing of Surgical Intervention:
Individualized Timing: The optimal timing for cataract surgery is determined based on several factors, ensuring the best possible visual outcomes for the child. These factors include:
The child’s age at diagnosis.
The severity of the cataract and its impact on vision.
The presence of any other associated eye conditions or health issues.
Early Surgery Recommendation: Generally, early surgical intervention is recommended for visually significant congenital cataracts to:
Prevent visual deprivation amblyopia (lazy eye), which can develop if vision is impaired early in life.
Promote normal visual development during critical periods of visual pathway maturation in infancy.
Delayed Surgery (Selective Cases): In certain specific situations, surgical intervention may be intentionally delayed, for example:
When there are other underlying medical conditions that need to be stabilized or addressed first before undergoing eye surgery.
Correction of Refractive Errors:
Post-Surgery Refractive Changes: Following cataract surgery, children frequently develop refractive errors, as the eye’s natural lens has been removed. Common refractive errors include:
Nearsightedness (myopia)
Farsightedness (hyperopia)
Corrective Measures: To optimize visual acuity after surgery, corrective measures are necessary, such as:
Prescription eyeglasses, with lenses tailored to correct the refractive error.
Contact lenses, offering a wider field of vision and potentially better visual acuity in some cases, particularly for younger children or unilateral cataracts.
Amblyopia Management:
Amblyopia Risk: Amblyopia, also known as “lazy eye,” is a common and significant complication associated with congenital cataracts.
Mechanism of Amblyopia: Amblyopia develops when the brain favors one eye over the other due to early visual deprivation in the eye with the cataract. The visual pathways for the weaker eye do not develop properly.
Amblyopia Treatment: Treatment strategies are essential to encourage visual development in the weaker eye and may include:
Eye Patching: Patching the stronger, better-seeing eye to force the child to use the weaker, amblyopic eye, stimulating its visual pathway development.
Blurring the Stronger Eye: Using eye drops or special lenses to temporarily blur vision in the stronger eye, achieving the same effect as patching by encouraging use of the weaker eye.
Regular Follow-up and Monitoring:
Long-Term Care is Essential: Children with congenital cataracts require lifelong regular follow-up and ongoing monitoring by a pediatric ophthalmologist to ensure optimal visual outcomes and detect any complications.
Regular Eye Examinations: Scheduled eye examinations are crucial for:
Assessing visual acuity at regular intervals to track visual development.
Monitoring for any potential postoperative complications, such as glaucoma, retinal detachment, or lens reproliferation.
Adjusting treatment plans as needed, including changes in glasses prescriptions, contact lens fitting, or amblyopia therapy adjustments, to optimize vision throughout childhood and adolescence.

Complications of Congenital Cataracts
Although cataract surgery is generally safe and effective, several potential complications can arise following the procedure for congenital cataracts.
Cloudy Vision (Posterior Capsule Opacification – PCO): After cataract surgery, a common occurrence is the development of posterior capsule opacification (PCO).
Lens Capsule Thickening: PCO is characterized by a thickening of a part of the lens capsule that remains in place after the original cloudy lens is removed.
Cloudy Vision Recurrence: This thickening can lead to a clouding of vision, as if the cataract is returning.
Not Cataract Recurrence: It is crucial to understand that PCO is not the cataract itself growing back, but rather the growth and opacification of cells on the lens capsule behind the implanted lens.
Timeline: PCO typically develops within a few months to a year after the initial cataract surgery, often between 4 and 12 months postoperatively.
Correction Required: PCO may necessitate a secondary procedure to restore clear vision, often a laser capsulotomy.
Lazy Eye (Amblyopia): Amblyopia, commonly known as “lazy eye,” is a significant risk following congenital cataract treatment.
Weaker Eye Preference: Amblyopia can occur if vision in one eye is weaker than the other, often due to the visual deprivation caused by the cataract early in life.
Brain Suppression: The brain may begin to favor the stronger eye, effectively ignoring visual signals from the weaker eye.
Improper Visual Development: This can lead to the weaker eye’s visual pathways not developing properly, resulting in reduced visual acuity that is not correctable with glasses alone.
Patching Treatment: Standard treatment for amblyopia involves patching the stronger eye to force the brain to rely on and strengthen the weaker eye’s visual pathways. Blurring the vision in the stronger eye with eye drops is another treatment method.
Glaucoma (Increased Intraocular Pressure): Glaucoma, characterized by elevated pressure inside the eye, is a potential long-term complication.
Vision-Threatening Condition: Glaucoma can damage the optic nerve and lead to progressive vision loss if untreated.
Lifelong Risk: Children who have undergone cataract surgery have an increased lifelong risk of developing glaucoma.
Regular Monitoring Needed: Requires regular eye pressure measurements by an ophthalmologist or optometrist throughout life to detect and manage glaucoma early if it develops.
Squint (Strabismus): Squint, also known as strabismus or crossed eyes, is a misalignment of the eyes.
Eyes Looking in Different Directions: In strabismus, the eyes do not look in the same direction at the same time.
Post-Cataract Surgery Complication: Squint can develop as a complication following cataract surgery, potentially due to changes in vision or eye muscle balance.
Pupil Abnormalities: Changes in pupil shape can occur after surgery.
Oval Pupil Shape: The pupil, normally round, may sometimes become more oval-shaped following cataract surgery.
Usually Minor Visual Impact: These pupil shape abnormalities are usually cosmetic and do not typically significantly affect vision.
Retinal Detachment: Retinal detachment is a serious, though less common, complication.
Retina Separation: This occurs when the retina, the light-sensitive layer at the back of the eye, separates from the underlying inner wall of the eye.
Vision Impairment: Retinal detachment is a sight-threatening condition that can lead to significant and permanent vision loss if not treated promptly.
Post-Cataract Surgery Risk: While rare, retinal detachment is a potential complication that can occur after cataract surgery.
Cystoid Macular Edema (CME): Cystoid Macular Edema (CME) involves fluid accumulation in the retina.
Fluid Buildup in Retina: CME is characterized by the build-up of fluid between the layers of the macula, the central part of the retina responsible for sharp, detailed vision.
Vision Affecting: This fluid accumulation can distort the normal retinal structure and affect central visual acuity.
Infection (Endophthalmitis): Endophthalmitis is a rare but severe intraocular infection.
Intraocular Infection: Endophthalmitis is a serious infection inside the eye, involving the intraocular fluids and tissues.
Rare Post-Surgical Complication: It is a rare complication that can occur after any intraocular surgery, including cataract surgery.
Aggressive Treatment Needed: Requires prompt and aggressive treatment with antibiotics or even further surgery to manage the infection and prevent severe vision loss.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

