Integumentary Disorders of the Skin
Subtopic:
Eczema

Eczema, also known as atopic dermatitis or atopic eczema, is a skin condition characterized by areas of skin that become:
Inflamed
Itchy
Red
Cracked
Rough
Small fluid-filled sacs called blisters may sometimes develop.
Eczema is frequently observed in children. It is a recurring skin condition that presents with intense itching, along with swelling, redness, and dryness of the skin. Due to persistent scratching, the skin may exhibit flaking, cracking, oozing, blisters, or bleeding.
Several elements have been linked to eczema, including genetic changes and a family history of the condition. While there is currently no cure for eczema, it is not contagious. It is often associated with allergies.
Causes of Eczema
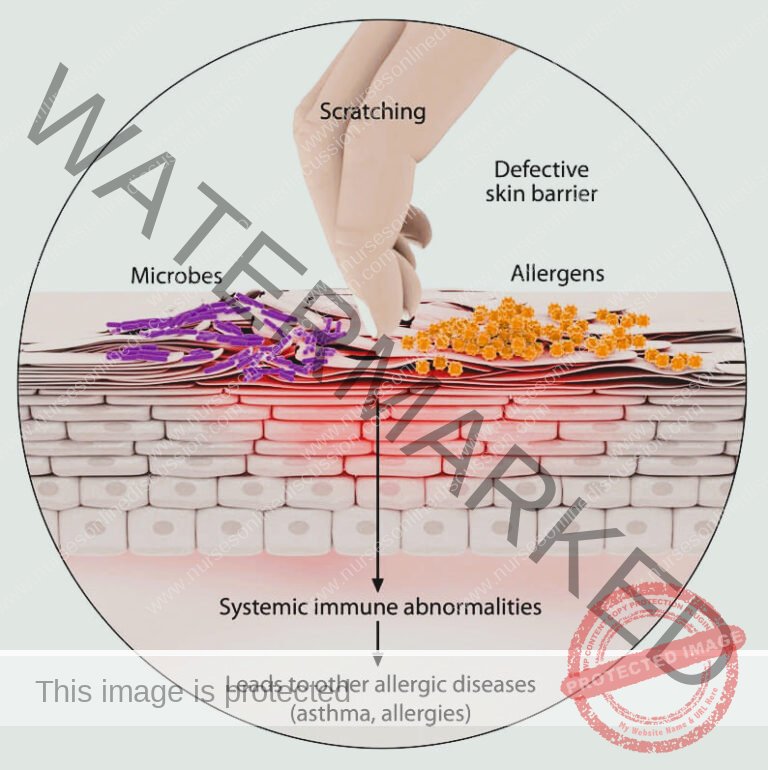
The precise origins of eczema remain elusive; however, current understanding suggests it arises from a complex interplay between genetic predispositions and environmental influences.
Genetic Factors:
Family History: Individuals with a family history of eczema or related atopic conditions—such as asthma or allergic rhinitis (hay fever)—are at an elevated risk of developing eczema. This suggests a hereditary component to the disorder.
Inherited Genetic Variations: Genetic mutations can compromise the skin’s natural barrier function. This weakened barrier makes the skin more susceptible to penetration by irritants and allergens from the external environment, contributing to eczema development.
Environmental Factors:
Irritants: Exposure to various substances that irritate the skin can trigger eczema flare-ups. These irritants include:
Harsh cleansing agents: Strong soaps, laundry detergents, dishwashing liquids, and certain shampoos can strip the skin of its natural oils and protective barrier.
Disinfectants: Chemical disinfectants used in cleaning can be harsh on sensitive skin.
Plant-based irritants: Even natural substances like juices from fresh fruits, raw meats, or vegetables can contain compounds that irritate the skin in susceptible individuals.
Certain Fabrics: Specific materials, such as wool or synthetic fabrics, can be abrasive or occlusive, leading to skin irritation and eczema symptoms.
Allergens: Exposure to common allergens in the environment can exacerbate eczema in sensitive individuals. These allergens may include:
House dust mites: Microscopic creatures found in house dust.
Pet dander: Skin flakes and proteins shed by animals.
Pollen: Airborne particles released by trees, grasses, and weeds.
Mold spores: Microscopic fungi that thrive in damp environments.
Dander: General term for skin scales, often referring to human dandruff.
Microbes: The presence and activity of certain microorganisms on the skin can play a role in eczema. These microbes can include:
Bacteria: Specifically, Staphylococcus aureus bacteria are commonly found on eczema-affected skin and can worsen inflammation.
Viruses
Fungi
Environmental Conditions: External environmental factors can significantly impact eczema symptoms:
Extreme Temperatures: Both very hot and very cold temperatures can be detrimental to eczema-prone skin.
Humidity Fluctuations: Changes in humidity, both excessively dry and excessively humid conditions, can trigger or worsen eczema flare-ups.
Dietary Factors:
Common Food Triggers: Certain food items have been identified as potential triggers for eczema symptoms in some individuals. These commonly implicated foods can include:
Dairy products (milk, cheese, yogurt)
Eggs
Nuts
Seeds
Soy products
Wheat
Other Influencing Factors:
Stress: Psychological stress is known to be a significant trigger that can worsen existing eczema symptoms and lead to flare-ups.
Hormonal Changes: Fluctuations in hormone levels within the body can influence eczema. These hormonal shifts may occur during:
Pregnancy
Menstrual cycle
Age: Eczema is notably more prevalent in infants and children, although it can affect individuals across the entire lifespan, from childhood through adulthood.
Skin Dryness: Pre-existing dry skin is a major contributing factor that can significantly worsen eczema symptoms. Maintaining adequate skin hydration is therefore crucial
Classification of Eczema
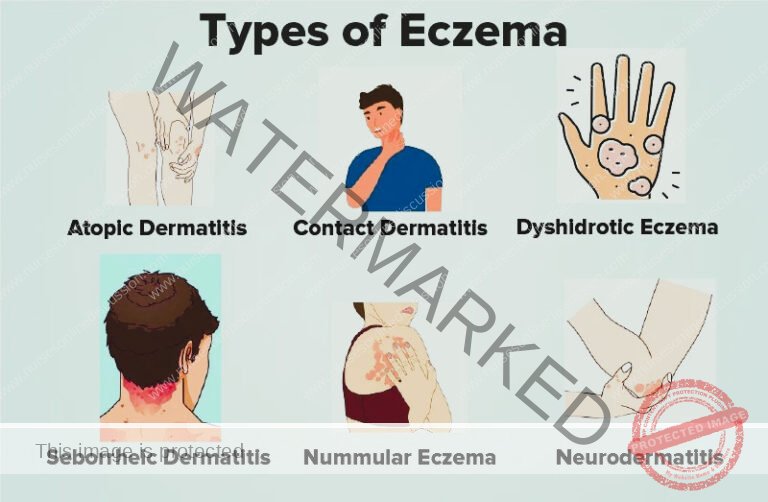
The National Eczema Association categorizes eczema into several distinct types, reflecting the diverse ways this skin condition can manifest.
Table 1. Common Types of Eczema
| Classification | Description |
| Atopic Dermatitis | Characterized by xerosis (excessively dry skin) and intense pruritus (itching). This is the most prevalent form of eczema, often starting in childhood. |
| Contact Dermatitis | Skin reactions and lesions that arise due to contact with specific allergens or irritants. This type is triggered by external substances coming into direct contact with the skin, causing inflammation. |
| Seborrheic Dermatitis | A papulosquamous (characterized by papules and scales) skin condition identified by greasy scales, typically appearing on the scalp. It can also affect other areas rich in oil glands, such as the face and chest. |
Table 2. Less Common Types of Eczema
| Classification | Description |
Dyshidrosis (Dyshidrotic Eczema/ Housewife’s Eczema) | Manifests as intensely pruritic vesicles (small, fluid-filled blisters) along with thickening and cracks in the skin. These symptoms typically appear on the palms, soles, and lateral borders of fingers and toes, often triggered by stress, allergies, or irritants. |
Nummular Dermatitis (Discoid Eczema) | Characterized by well-defined, coin-shaped lesions that are often oozing. These distinctive round lesions commonly appear on the lower extremities. The exact cause of nummular dermatitis remains unknown. |
Stasis Dermatitis (Varicose eczema/Venous eczema) | Frequently observed on the ankles of older individuals (typically aged 50 and above) who have underlying blood circulation problems, particularly venous insufficiency. If left unmanaged, stasis dermatitis can progress and potentially lead to the development of leg ulcers. |
| Dermatitis Herpetiformis | Strongly linked to celiac disease (gluten sensitivity). Presents as a symmetrical, intensely itchy rash. The rash typically appears on specific body areas including the arms, knees, back, and thighs. |
Neurodermatitis (Lichen Simplex Chronicus) | Defined by a localized, thickened, hyperpigmented (darkened skin), and intensely pruritic patch. This type of eczema often results from a cycle of repeated scratching and rubbing of a specific area of skin, leading to lichenification (thickening of the skin). |
Autoeczematization (Autosensitization) | Represents a skin reaction to microorganisms, such as bacteria, fungi, or viruses, that occurs at a site distant from the primary infection. This “auto-sensitization” is a secondary eczema that develops as a response to an infection elsewhere in the body, rather than at the site of infection itself. |
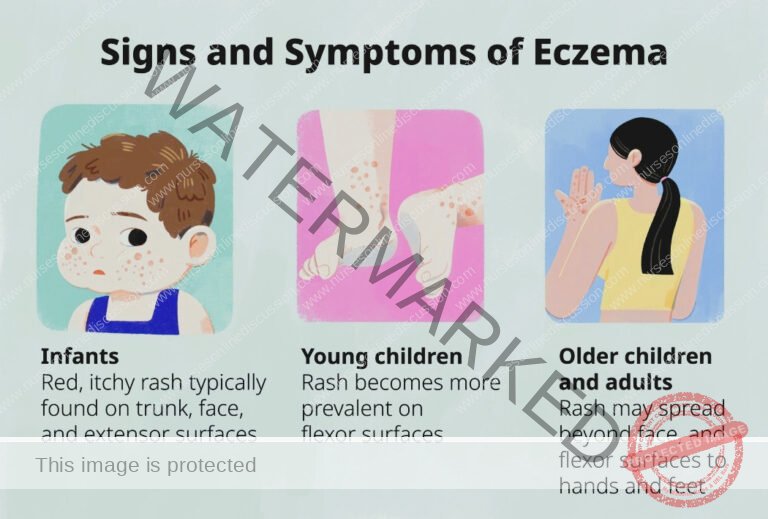
Symptoms of Atopic Eczema by Age Group
The symptoms of atopic eczema can differ depending on the age of the individual.
Infants (Under 2 Years Old):
Rash Location: Rashes commonly manifest on the scalp and cheeks.
Rash Appearance: Typically, rashes initially appear as small bumps that evolve into fluid-filled blisters before weeping or leaking fluid.
Intense Itch: Extreme itchiness (pruritus) is a hallmark symptom and can significantly disrupt sleep patterns.
Skin Infections: Persistent rubbing and scratching due to intense itching can break the skin and increase the risk of secondary skin infections.
Children (2 Years Until Puberty):
Rash Location: Rashes frequently develop in the flexural areas of the body, specifically:
Behind the creases of the elbows and knees.
Neck.
Wrists.
Ankles.
Buttock-leg creases.
Chronic Rash Changes: Over time, eczema rashes in children may undergo characteristic changes:
Become bumpy and raised.
Change in skin color (hyperpigmentation or hypopigmentation).
Thicken (lichenification) due to chronic scratching and rubbing.
Develop small, firm knots (papules).
Lead to persistent, chronic itching.

Adults:
Rash Location: Commonly, rashes appear in the flexural areas such as:
Creases of the elbows and knees.
Nape of the neck (back of the neck).
May also cover broader areas of the body.
Facial and Periocular Rashes: Noticeable rashes may develop on the:
Neck.
Face.
Skin around the eyes.
Skin Characteristics:
Skin can become extremely dry and prone to irritation.
Rashes may be persistently itchy (chronic pruritus).
Rash Appearance: Adult eczema rashes often present as:
More scaly in texture compared to those in children.
Secondary Infections: Scratching can lead to breaks in the skin, increasing susceptibility to skin infections.
Long-Term Effects: Adults with a childhood history of atopic dermatitis may continue to experience:
Dry or easily irritated skin even if childhood eczema has subsided.
Hand eczema (eczema specifically affecting the hands).
Eye problems related to chronic eczema around the eyes.
Diagnosis of Eczema
Assessment:
Eczema diagnosis primarily relies on clinical assessment, with itching being the defining symptom. Skin appearance varies based on the stage of eczema:
Acute Eczema: Represents the initial, active phase, characterized by:
Crusted skin patches.
Oozing lesions.
Eroded vesicles (small blisters that have broken open).
Erythematous plaques (raised, red patches of skin).
Papules (small, solid, raised bumps).
Subacute Eczema: Follows the acute phase, with skin exhibiting:
Erythematous scaly plaques (red areas with flaky skin).
Erythematous scaly papules.
Chronic Eczema: Represents the long-term stage, developing after repeated acute and subacute phases, showing:
Slightly pigmented (discolored patches of skin).
Lichenified plaques (thickened, leathery, and hardened skin due to chronic scratching).
Excoriations (areas of skin that have been scraped or scratched, often showing linear marks).
Skin Allergy Tests:
Skin allergy testing is valuable in identifying specific triggers that may worsen eczema:
Skin Prick Testing: A method to identify immediate allergic reactions.
Small quantities of suspected allergens are introduced into the skin, typically on the forearm or back, through tiny pricks.
Reactions, such as redness and swelling, are observed within about 15-20 minutes to identify immediate allergic triggers.
Patch Testing: Used to detect delayed-type hypersensitivity reactions, often associated with contact dermatitis.
Small patches containing potential contact allergens are applied to the skin, usually on the back, and remain in place for 48 hours.
The skin is examined after patch removal at 48 and 72 hours to assess for delayed allergic reactions, such as redness, vesicles, or itching, indicating contact allergens.
Food Allergy Testing: May be performed to identify food allergies that may be contributing to eczema symptoms, especially in children. Different methods may be used, including:
Blood tests: To measure IgE antibodies to specific foods.
Skin prick tests: For immediate food allergy reactions.
Elimination diets: Under medical supervision, to systematically remove and reintroduce suspected foods to observe symptom changes.
Skin Biopsy:
A skin biopsy is sometimes recommended to confirm the diagnosis and exclude other skin conditions:
A small skin sample is collected from an affected area, usually using a punch biopsy or shave biopsy technique.
The skin sample is then sent to a laboratory for microscopic examination by a dermatopathologist.
Skin biopsy helps to confirm the clinical diagnosis of eczema by examining cellular patterns and inflammatory markers.
It also aids in ruling out other skin disorders that may mimic eczema, such as psoriasis, cutaneous lymphoma, or infections.
Blood Tests – IgE Level:
Measuring Immunoglobulin E (IgE) levels in the blood can provide supportive diagnostic information:
IgE Level Measurement: A blood test is performed to measure the level of IgE antibodies in the patient’s serum.
Elevated IgE Association: Elevated IgE levels are frequently observed in individuals with atopic eczema, suggesting an allergic component to their condition and atopic predisposition.
Not Definitive Diagnosis: While elevated IgE levels can support the diagnosis of atopic eczema, it is not a definitive diagnostic test on its own, as IgE levels can be elevated in other allergic conditions as well. Clinical correlation and other diagnostic criteria are necessary.

Treatment and Management of Eczema
Eczema is a chronic condition without a definitive cure. The goals of eczema treatment are to:
Heal Affected Skin: Resolve current skin lesions and inflammation.
Prevent Flare-Ups: Minimize the frequency and severity of future symptom exacerbations.
Treatment approaches are personalized and tailored to each individual, taking into account:
Age
Specific symptoms
Overall health status
Severity of eczema
While eczema may resolve spontaneously in some individuals, for many, it is a long-term, lifelong condition requiring ongoing management.
Home Care Strategies
Essential self-care practices at home form the foundation of eczema management:
Lukewarm Baths: Bathe in lukewarm water, avoiding hot water, which can further dry out the skin and worsen eczema.
Moisturization: Crucially, apply a moisturizer generously within 3 minutes of bathing. This “locks in” moisture, hydrating the skin. Daily moisturization, especially after bathing, is paramount for eczema management.
Clothing Choices: Opt for loose-fitting clothing made from soft, breathable fabrics like cotton. Avoid:
Rough or scratchy fibers (e.g., wool).
Synthetic materials that can irritate the skin.
Tight-fitting garments that can rub and exacerbate eczema.
Gentle Cleansing: When washing, use mild soaps or non-soap cleansers. Avoid harsh soaps that can strip the skin of its natural protective oils.
Skin Drying Technique: After bathing or washing, air dry the skin when possible or gently pat the skin dry with a soft towel. Vigorously rubbing the skin should be avoided as it can irritate eczema patches.
Temperature Regulation: Maintain a comfortable skin temperature by:
Avoiding rapid temperature changes.
Limiting activities that induce excessive sweating, as sweat can irritate eczema.
Trigger Avoidance: Actively identify and diligently avoid personal eczema triggers. Common triggers vary but can include allergens, irritants, stress, or specific foods.
Humidifier Use: Utilize a humidifier, particularly during dry or cold weather, to add moisture to the air and help prevent skin dryness.
Nail Care: Keep fingernails short and trimmed to minimize skin damage from scratching and reduce the risk of infection.
Medications
Pharmacological treatments play a key role in managing eczema symptoms and flare-ups:
Topical Corticosteroids: These are the mainstay of eczema treatment.
Anti-inflammatory creams or ointments are applied directly to the affected skin.
They effectively reduce inflammation and itching, the core symptoms of eczema.
Systemic Corticosteroids: Used for severe eczema flare-ups that are not controlled by topical treatments.
Administered via injection or oral route.
Powerful anti-inflammatory effect but used for short periods only due to potential side effects with long-term use.
Antibiotics: Prescribed when eczema is complicated by a secondary bacterial skin infection. Antibiotics target and treat the bacterial infection, which can worsen eczema symptoms.
Antiviral and Antifungal Medications: Used to treat eczema when fungal or viral infections are also present and contributing to the skin condition.
Antihistamines: Primarily used to alleviate nighttime scratching and improve sleep quality.
Certain antihistamines have sedating properties, inducing drowsiness, which can help reduce nighttime scratching that often occurs unconsciously.
Topical Calcineurin Inhibitors: Non-steroidal, immunomodulating medications.
Applied topically to suppress immune system activity in the skin.
Reduce inflammation and help prevent eczema flare-ups by modulating the immune response.
Calcineurin inhibition: These drugs act by inhibiting calcineurin, an enzyme crucial in the activation of T-cells, thereby reducing the release of inflammatory cytokines.
Barrier Repair Moisturizers: Specialized moisturizers designed to:
Reduce transepidermal water loss from the skin, improving hydration.
Repair and restore the skin’s natural barrier function, strengthening its protective capabilities against irritants and allergens.
Other Therapeutic Modalities
Phototherapy: Utilizes controlled exposure to ultraviolet (UV) light as a treatment option for moderate to severe eczema.
Typically administered under medical supervision in a clinic or dermatology office.
Skin is closely monitored during phototherapy treatments to minimize risks and optimize effectiveness.
Ongoing Care and Maintenance
Long-term management is essential, even when eczema symptoms are under control:
Continued Skin Care Routine: Even after eczema lesions have healed, it is crucial to persist with a consistent skin care routine to maintain skin health and prevent future flare-ups.
Regular Moisturizing: Regular and diligent moisturizing remains a cornerstone of long-term eczema management.
Trigger Avoidance: Continued vigilance and avoidance of identified eczema triggers is vital to minimizing symptom recurrence and maintaining remission.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

