Integrated Management of Childhood Illnesses (IMCI)
Subtopic:
Integrated Management of Childhood Illnesses
Integrated Management of Childhood Illnesses represents a holistic approach to managing sick children, ensuring that their care and treatment are considered comprehensively.
Definition and Origin:
IMCI Acronym: IMCI stands for Integrated Management of Childhood Illnesses.
Development: This approach was collaboratively developed by the United Nations Children’s Fund (UNICEF) and the World Health Organization (WHO).
Purpose: IMCI is designed as a strategy to significantly improve the overall health and well-being of children under the age of five years on a global scale.
Core Focus of IMCI:
Holistic Child Health: IMCI is centered on an integrated view of child health, prioritizing the comprehensive well-being of the child rather than addressing illnesses in isolation.
Primary Objectives: IMCI is fundamentally aimed at:
Mortality Reduction: Decreasing the incidence of death in children.
Morbidity Reduction: Lowering the rates of illness and sickness.
Disability Reduction: Minimizing long-term disabilities arising from childhood illnesses.
Promotion of Growth and Development: Fostering improved growth and optimal developmental milestones in children under five.
Preventive and Promotive Approach: IMCI is designed not only to treat sickness but also to proactively reduce preventable deaths, lessen the burden of disease and disability, and actively support healthy growth and development in young children.
Practical Application of IMCI Guidelines:
Enhanced Clinical Practice: IMCI guidelines are structured to assist healthcare providers in:
Accurate Caretaker Interviewing: Improving skills in effectively communicating with caregivers to gather precise information about the child’s illness.
Clinical Sign Recognition: Sharpening the ability to correctly identify and interpret key clinical signs and symptoms.
Appropriate Treatment Selection: Guiding the choice of suitable and effective treatments based on accurate diagnosis and classification.
Counseling Provision: Facilitating the delivery of essential counseling to caregivers on home care and follow-up.
Preventive Care Measures: Integrating preventive strategies into routine child healthcare visits for children up to 5 years of age.
Key Goals of IMCI Implementation:
Identify Major Mortality Causes: To pinpoint the principal diseases and conditions that contribute to childhood deaths.
Explain Integrated Case Management: To elucidate the meaning and rationale behind a unified approach to managing childhood illnesses.
Describe IMCI Strategy Steps: To outline the essential steps and components that constitute the IMCI strategy framework.
Introduce IMCI Tools Utilization: To familiarize healthcare providers with the use of practical IMCI tools, which include:
Chart Booklets
Wall Posters
Case Management Sheets
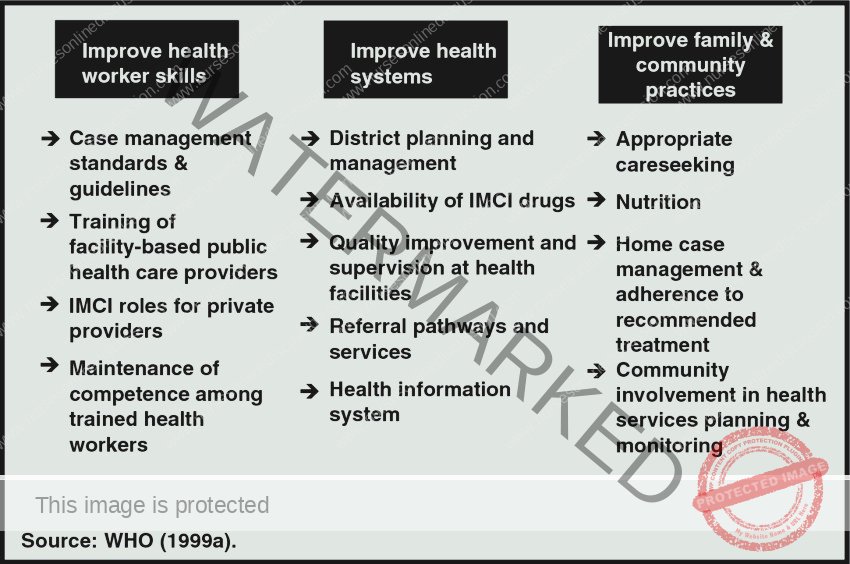
Key Components of IMCI
IMCI is structured around three essential areas within healthcare:
Boosting healthcare provider skills in case management.
Strengthening health systems for quality care delivery.
Improving family and community health practices to promote health, growth, and development.
CHILD HEALTH AND MORTALITY
In 2015, global child mortality reached approximately 5.9 million deaths in children under five. This equates to about 16,000 deaths daily. The primary causes are infections, newborn-related conditions, and nutritional deficiencies. A significant concern is that a large percentage of these deaths are preventable.
Uganda is noted to have a high rate of child mortality. The World Health Organization (WHO) ranks Uganda 168th out of 188 countries for infant mortality rates. World Bank data from 2016 reported Uganda’s under-five mortality rate as 53 deaths per 1,000 live births.

Seventy-five percent (75%) of the common causes of child mortality in developing countries include:
Roughly three-quarters of childhood deaths in developing nations stem from the following factors:
Infectious Diseases: Major contributors include acute respiratory infections, diarrheal illnesses, malaria, and measles. These diseases are particularly dangerous for young children, potentially leading to severe illness and death, especially where healthcare access and preventative measures are limited.
Malnutrition: A significant factor in child deaths, malnutrition weakens children’s immune systems. This makes them more vulnerable to infections and reduces their ability to recover from sickness.
It’s important to recognize that these factors often occur together, with children potentially suffering from multiple conditions simultaneously. The similar symptoms of these illnesses can also complicate accurate diagnosis and effective treatment.
WHY IMNCI? (Need for IMCI)
IMCI is crucial for addressing the complexities of childhood illness due to several reasons:
Multiple Co-occurring Conditions: Children frequently suffer from several life-threatening conditions at the same time. IMCI employs a comprehensive strategy, addressing all potential health issues to minimize preventable death and support healthy development. By enabling integrated assessment and combined treatments, IMCI prioritizes effective case management and disease prevention, promoting healthy growth.
Limited Diagnostic Resources: Many healthcare settings lack advanced diagnostic tools like lab tests or X-rays. IMCI acknowledges this limitation and uses clinical guidelines based on patient history, signs, and symptoms for diagnosis. IMCI training equips healthcare workers to effectively manage childhood illnesses even when resources are scarce.
Importance of Patient History: IMCI highlights the critical role of patient history in diagnosing and managing childhood diseases. Healthcare providers are trained to collect detailed information about a child’s symptoms, past illnesses, and other relevant factors. This information, alongside IMCI clinical guidelines, aids in accurate diagnosis and appropriate treatment decisions.
Necessity of Referrals: When a child has a severe illness needing specialized care, IMCI stresses the importance of timely referrals to higher-level facilities. By identifying serious cases and facilitating prompt referrals, IMCI helps ensure children get necessary specialist treatment and support.
IMCI PROCESS
The Integrated Management of Childhood Illness (IMCI) process is a detailed method for identifying and treating childhood illnesses in outpatient settings. It aims to improve the quality of healthcare for children under five using standardized guidelines and treatments.
IMCI Process:
Condition Checklist: IMCI involves systematically checking for a range of conditions in infants and children to ensure a thorough assessment and treatment plan.
Comprehensive Assessment and Treatment: Children are evaluated and treated for all identified conditions using standardized guidelines to direct management decisions.
Referral Decision-Making: IMCI guidelines provide clear instructions on when it’s necessary to refer a child to more advanced levels of care for further management.
Interventions Included in the IMCI Guidelines:
The IMCI guidelines include both treatments for existing illnesses and preventative measures for various childhood conditions.
Curative Interventions:
Acute Respiratory Infections (ARI) including pneumonia
Anaemia
Diarrhoea (dehydration, persistent, dysentery)
Ear infections
HIV/AIDS
Local bacterial infections
Meningitis and sepsis
Malnutrition
Wheeze
Malaria
Measles
Neonatal jaundice
Preventive Interventions:
Breastfeeding support
Immunization
Nutrition counseling
Periodic deworming
Vitamin A supplementation
Zinc supplementation
Who Can Use IMCI:
IMCI is designed for use by all doctors, nurses, and other healthcare professionals who provide care to infants and children under five years of age. It is primarily intended for use in primary healthcare settings like clinics, health centers, and hospital outpatient departments.
The Case Management Process
IMCI categorizes children into two groups for management purposes:
Sick Young Infants (1 week to 2 months): IMCI primarily focuses on infants in this age range. Newborns under one week old are typically excluded as their illnesses are often related to factors during pregnancy, labor, and delivery, which require different management approaches.
Sick Children (2 months to 5 years): This category encompasses children from two months up to their fifth birthday.
IMCI is specifically designed for use by healthcare providers (including doctors and nurses) who are working in primary healthcare settings such as clinics, health centers, or outpatient departments of hospitals, to manage sick children and infants.
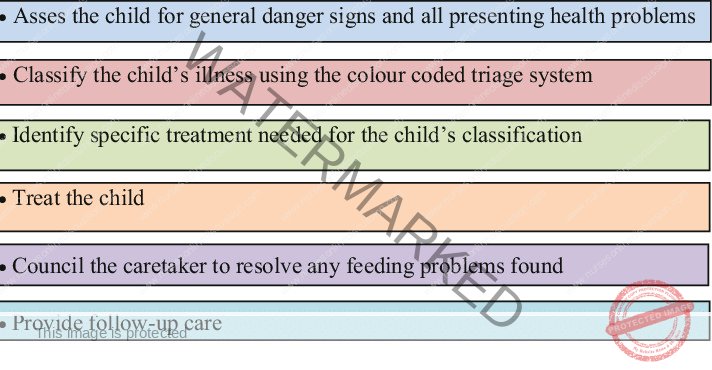
The IMCI case management process involves a series of key steps:
Assessment of the Child/Young Infant: This involves gathering the child’s medical history and conducting a physical examination to understand their condition.
Illness Classification: Based on the assessment, the healthcare provider determines the severity of the illness and assigns it to a specific category of classification. This classification reflects the urgency and type of care needed.
Treatment Identification: Once the illness is classified, the appropriate treatment strategy is identified based on IMCI guidelines.
Treatment Administration: The identified treatment is then provided to the child or young infant.
Maternal Counseling: Crucially, the mother or caregiver receives counseling on how to care for the child, administer any home treatments, and recognize danger signs.
Follow-up Care Planning: Arrangements for follow-up care are made to monitor the child’s progress and address any ongoing issues.
Assessing the child involves history taking and physical examination to get a complete picture of the child’s health status.
Classifying the illness is about determining the seriousness of the condition. It’s a decision-making process where the healthcare provider selects a classification category that reflects the disease’s severity. It is important to note that these classifications are not specific diagnoses. Instead, they guide treatment decisions. For example, “severe febrile disease” is a classification that could encompass conditions like cerebral malaria, meningitis, or septicemia. The recommended treatment for this classification is designed to address all potential underlying causes.
Steps in Integrated Case Management according to IMCI guidelines:
STEP 1: ASSESS
The ‘Assess’ section within the IMCI chart booklet guides healthcare workers on how to effectively take a patient’s history and conduct a physical examination.
Establish effective communication with the child’s mother or caregiver to gather accurate information.
Initially, screen for general danger signs. These are indicators of potentially life-threatening conditions that require immediate attention.
Ask specific questions focusing on common childhood illnesses such as diarrhea, pneumonia, and fever.
If any danger signs or positive responses to specific questions are identified, prioritize a focused physical examination to detect life-threatening illnesses.
Evaluate the child’s nutritional and immunization status to identify any related needs.
The assessment should be comprehensive, including checks for other health problems beyond the primary complaint.
STEP 2: CLASSIFY
The ‘Classify’ section (often labeled ‘signs and classify’) in the IMCI chart provides a list of clinical signs of various illnesses alongside their corresponding classifications. “Classify” here means the health worker needs to decide on the severity of the illness based on observed signs and symptoms.
Based on the assessment findings, classify each of the child’s illnesses using a specially designed color-coded triage system.
Because children frequently present with multiple health issues, each identified condition is classified to indicate the required level of care:
COLOUR CLASSIFICATION
PINK: Indicates a severe classification. Requires urgent admission to hospital or pre-referral treatment followed by immediate referral to a higher-level facility.
YELLOW: Indicates a classification that requires specific medical treatment at the health facility and advice to the caregiver on home care.
GREEN: Indicates a non-serious classification. In most cases, medications are not needed. Focus is on providing simple advice on home management to the caregiver.
STEP 3: IDENTIFY TREATMENT
The ‘Identify Treatment’ section assists healthcare providers in quickly and accurately determining the appropriate treatments for each identified classification.
If a child or young infant has multiple classifications, it’s essential to consult multiple treatment tables within the IMCI guidelines to ensure all conditions are addressed appropriately.
COLOUR CLASSIFICATION
PINK: For children requiring urgent referral, determine and administer essential pre-referral treatment to stabilize the child’s condition before transfer.
YELLOW: For children needing specific treatment at the facility, develop a treatment plan, identify necessary medications for clinic administration, and determine the essential advice to provide to the mother or caregiver for ongoing care.
GREEN: If no serious conditions are classified (green), concentrate on delivering appropriate advice to the mother or caregiver regarding actions needed for the child’s care at home.
STEP 4: TREAT
The ‘Treat’ section details how to implement the treatments identified for each classification. ‘Treat’ encompasses administering treatments within the healthcare facility, prescribing medications or other treatments for home use, and importantly, educating the mother/caregiver on how to correctly administer home treatments.
COLOUR CLASSIFICATION
PINK: When a child or young infant needs hospital admission or referral, it is crucial to administer essential treatment before the admission or referral process to improve their condition en route.
YELLOW: If specific treatment is required, create a treatment plan, administer the necessary medications at the facility, advise on treatment to be given at home, and provide thorough counseling to the mother/caregiver.
GREEN: When the classification is green and no serious conditions are present, the primary action is to advise the mother/caregiver on appropriate home care practices for the child.
STEP 5: COUNSEL
If follow-up care is necessary, clearly instruct the mother/caregiver on when to return to the clinic for a follow-up appointment. Also, thoroughly educate them on danger signs – indications that necessitate immediately bringing the child or young infant back to the facility.
Conduct an assessment of the child’s feeding practices, with a focus on breastfeeding, and provide counseling to address any identified feeding problems. This step also includes offering counseling to the mother about her own health and well-being.
STEP 6: FOLLOW-UP
Certain children or young infants may require more than one visit for the same illness. Identify these individuals and ensure they are brought back for appropriate follow-up care as indicated in the IMCI guidelines. During follow-up visits, re-assess the child or young infant for any new health concerns that may have arisen.
The IMCI guidelines are also designed to empower healthcare workers to:
Recognize children who need additional follow-up visits to monitor their recovery.
Deliver appropriate follow-up care based on specific guidance within the IMCI protocols.
Provide effective counseling to mothers regarding their own health needs and well-being.
Offer counseling on preventative and treatment measures to promote ongoing child health.
When necessary, re-evaluate the child for any new health issues that may have emerged since the initial consultation.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

