Medical Conditions Affecting the Nervous System
Subtopic:
Intersexual Disabilities

“Intersex” serves as a broad term encompassing individuals born with sexual or reproductive anatomy that does not fit typical binary understandings of “male” or “female.”
Historically, people with intersex traits were incorrectly labeled using terms like “hermaphrodites,” “congenital eunuchs,” or “congenitally frigid.” These older terms are now considered inappropriate and stigmatizing. Specifically, “hermaphrodite” is seen as inaccurate and harmful.
The term “intersexuality” was first proposed by Richard Goldschmidt in 1917. Prior to its wider adoption, a suggestion to replace “hermaphrodite” with “intersex” was put forward by Cawadias in the 1940s.
Normal Sexual Development
Typical human sexual development is characterized by two pairs of chromosomes: XX for females and XY for males.
Fertilization: At conception, the sperm cell determines the genetic sex of the embryo by contributing either an X chromosome (leading to female development) or a Y chromosome (leading to male development) to the egg.
Early Development: In the initial stages of pregnancy, both male and female embryos appear “anatomically the same.” The early forms of the reproductive organs, known as primitive gonads, begin to develop around the sixth week of pregnancy. At this point, these gonads have the potential to develop into either testes (male) or ovaries (female).
Gonadal Differentiation: The primitive gonads differentiate to become either testes (in males) or ovaries (in females) based on subsequent biological processes. This specialization begins around the seventh week of gestation.
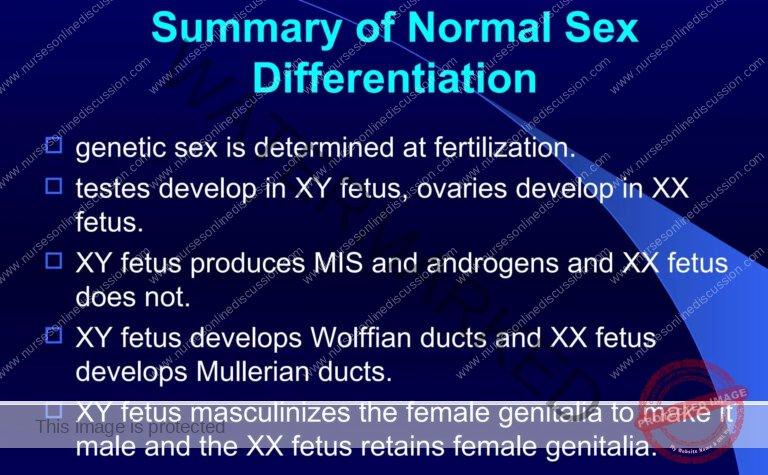
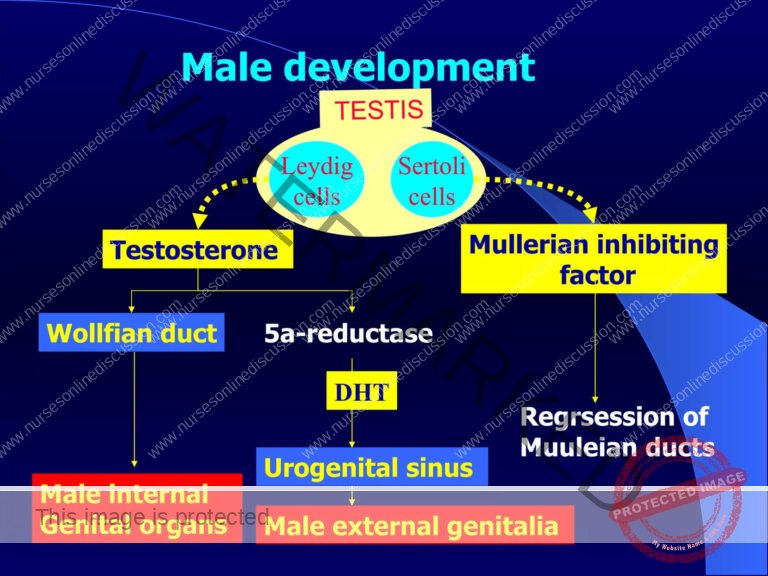
4.Hormonal Influence: Around the eighth week of gestation, in XY embryos, the gonads differentiate into functioning testes. These testes then begin to produce testosterone, a key hormone driving male sexual development. In contrast, in XX embryos, the gonads differentiate into ovaries around the twelfth week of gestation.
5.Duct System Development: Two duct systems are initially present in both sexes: the Müllerian and Wolffian ducts. In females (XX), the Müllerian duct system develops into the female reproductive tract, forming the uterus, Fallopian tubes, and the upper portion of the vagina. Simultaneously, in males (XY), a hormone called Müllerian Inhibiting Substance (MIS) causes the Müllerian ducts to regress or disappear. In males, androgens, particularly testosterone, stimulate the Wolffian duct system to develop into structures of the male reproductive tract.
6. Birth: Typically, by the time of birth, a fetus is fully “sexed,” exhibiting a clear alignment across genetic sex (XX or XY), the development of internal and external reproductive organs (gonads), and the appearance of external genitalia that conform to typical male or female presentations. This results in the newborn being readily identifiable as either male or female.

Causes of Intersex Conditions:
Intersex conditions arise from a variety of biological factors that disrupt typical sexual development. These can broadly be categorized into conditions that lead to a more masculine presentation, a more feminine presentation, and other variations.
Masculinizing Conditions:
XX Congenital Adrenal Hyperplasia (CAH):
This is a frequent cause of intersex traits in individuals with XX chromosomes. It involves the adrenal glands abnormally producing hormones that cause the development of male characteristics, known as virilizing hormones. These hormones promote masculine traits and influence the development of the male reproductive system and outward physical features.
Genetic testing during pregnancy can detect CAH genes in the developing embryo. Prenatal treatment using dexamethasone to try and reduce or prevent genital masculinization is a complex and debated approach.
In XX individuals with CAH, the degree of masculinization can vary, ranging from enlargement of the clitoris to a genital appearance that may closely resemble that of a typical male.
XX Progestin-Induced Virilization:
This condition was observed in the mid-20th century, specifically during the 1950s and 1960s, due to the use of progestin medications prescribed to pregnant women to prevent miscarriages.
Individuals affected by this condition have female internal reproductive anatomy but may develop secondary male characteristics. A notable effect is the development of an enlarged clitoris.
XX Freemartinism:
Freemartinism is predominantly observed in cattle. It occurs in female twin calves that are born alongside a male twin. Due to shared blood circulation in the womb, the female twin can be exposed to male hormones.
The affected female calf typically exhibits a female external appearance but is infertile. Behaviorally, she may also display traits more commonly associated with a castrated male.
Feminizing Conditions:
XY Androgen Insensitivity Syndrome (AIS):
AIS affects individuals with XY chromosomes who possess a genetic inability to properly respond to androgens, which are male sex hormones. This resistance to androgens leads to varying degrees of feminization of the body.
In complete AIS, individuals often present with a typically female external appearance, including a vagina. However, they have testes, which may be undescended or partially descended, rather than ovaries.
XY 5-Alpha-Reductase Deficiency (5-ARD):
This condition affects individuals with a Y chromosome and impairs the body’s ability to convert testosterone into dihydrotestosterone (DHT). DHT is a more potent androgen crucial for typical male external genital development.
At birth, individuals with 5-ARD often have ambiguous genitalia, meaning their genitals do not clearly appear male or female. The spectrum of effects can vary, ranging from predominantly male-appearing genitalia to genitalia that more closely resemble female genitalia but with clitoromegaly (enlarged clitoris).
XY Congenital Adrenal Hyperplasia (CAH):
In XY individuals who have CAH specifically due to a deficiency in the 17 alpha-hydroxylase enzyme, the typical virilization process is diminished in comparison to XX females with CAH or XY individuals with other forms of CAH.
XY Persistent Müllerian Duct Syndrome (PMDS):
PMDS affects XY individuals who possess male chromosomes but paradoxically develop a uterus and fallopian tubes internally. This occurs because of a lack of Müllerian Inhibiting Substance (MIS) during fetal development. MIS normally causes these female reproductive structures to regress in males.
XY Anorchia:
Anorchia is characterized by the loss or absence of testes after approximately 14 weeks of fetal development in XY individuals.
The absence of testes means there is no production of hormones needed for the development of male secondary sexual characteristics. This hormonal deficiency leads to a more feminine physical presentation.
XY Gonadal Dysgenesis:
This is a heterogeneous condition in XY individuals where the gonads do not develop fully or correctly. The failure of proper gonadal development can lead to intersex characteristics.
XY Hypospadias:
Hypospadias, where the opening of the urethra is not located at the tip of the penis, can be caused by a range of factors, including disruptions in testosterone metabolism during development.
The severity of hypospadias can vary significantly, from mild cases where the urethral opening is only slightly displaced to more severe cases where it is located much further down the penis or even in the perineum.
Other Chromosomal Sex Variations:
There are also less typical chromosomal sex variations that can result in intersex traits. These include:
Turner syndrome (XO)
Triple X syndrome (XXX)
Klinefelter syndrome (XXY) and its variants (XXYY, XXXY)
XYY syndrome
de la Chapelle syndrome (XX male)
Swyer syndrome (XY female)
Categories/Types of Intersex:
Intersex conditions can be broadly classified based on chromosomal and hormonal factors. The categories below often overlap with the causes of intersex conditions.
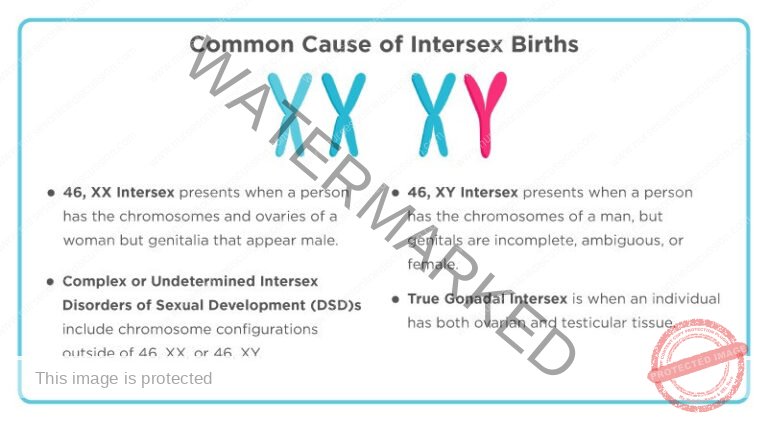
46, XX Intersex:
Chromosomal and Gonadal Sex: Individuals possess a typical female chromosomal makeup (46, XX) and ovaries.
External Genitalia: However, their external genitalia exhibit a more masculine appearance.
Primary Cause: This type is frequently caused by exposure to excessive male hormones (androgens) during fetal development within the uterus.
Specific Conditions: This category includes:
Congenital Adrenal Hyperplasia (CAH): The most prevalent cause.
Prenatal Exposure to Male Hormones: Hormonal medications taken by the pregnant person or other sources.
Maternal Tumors: Hormone-secreting tumors in the mother during pregnancy.
Aromatase Deficiency: Rare condition impacting estrogen production.
Physical Manifestations: This can result in the labia partially or completely fusing, and the clitoris enlarging. Importantly, the uterus and fallopian tubes are typically present and normally developed.
Previous Terminology: Formerly known as female pseudohermaphroditism.
Note on “46”: “46” signifies the standard human chromosome count – 23 pairs totaling 46 chromosomes, with half inherited from each parent.
46, XY Intersex:
Chromosomal Sex: Individuals have a typical male chromosomal composition (46, XY).
External Genitalia Presentation: Despite XY chromosomes, the external genitalia are incompletely formed, present ambiguously (neither clearly male nor female), or may appear predominantly female.
Internal Gonads: Internal testes may be present and can range from normal to malformed or even be absent.
Underlying Causes: These can be attributed to:
Testicular Development Issues: Conditions affecting the development or function of the testes, such as XY pure gonadal dysgenesis.
Testosterone Synthesis Problems: Deficiencies in the body’s ability to produce testosterone.
Androgen Action Impairment: Difficulties in the body’s ability to respond to or utilize testosterone effectively. Examples include:
Androgen Insensitivity Syndrome (AIS): The most frequent cause within this category, characterized by non-functional or poorly functioning androgen receptors.
5-Alpha-Reductase Deficiency (5-ARD): Impaired conversion of testosterone to the more potent dihydrotestosterone (DHT). Babies with 5-ARD often exhibit ambiguous genitalia at birth, but virilization may occur more typically during puberty.
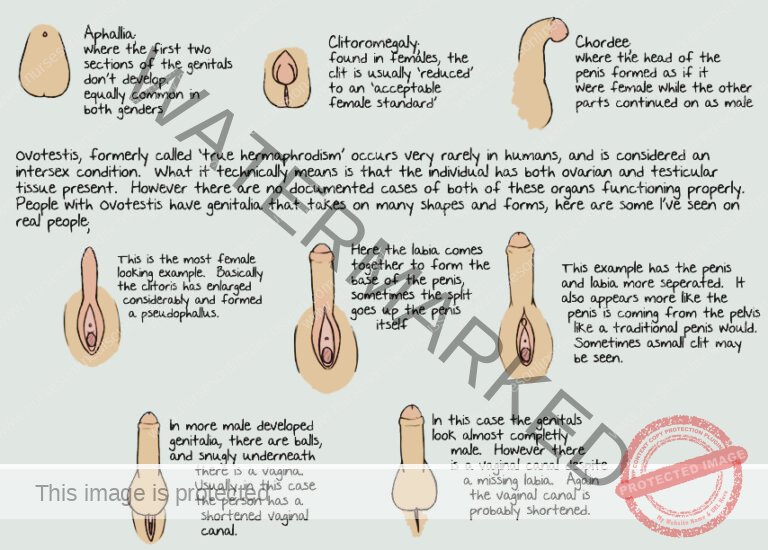
True Gonadal Intersex:
Gonadal Tissue: Individuals possess both ovarian and testicular tissue. This combined tissue can be in the form of an ovotestis (single gonad containing both types) or as a separate ovary and testis.
Chromosomal Variations: Chromosomal makeup can be diverse, including XX, XY, or a mix of both (mosaicism).
Genital Appearance: External genitalia can be ambiguous, female-typical, or male-typical.
Previous Terminology: Formerly known as true hermaphroditism.
Etiology: The precise causes are frequently unknown. Some research in animal models has suggested a possible link to exposure to agricultural pesticides, but further research is needed to confirm environmental links in humans.
Complex or Undetermined Intersex Disorders of Sexual Development:
Chromosomal Complexity: This category includes various chromosomal configurations that deviate from the standard 46, XX or 46, XY patterns.
Examples:
45, XO (Turner Syndrome): Presence of only one X chromosome.
47, XXY (Klinefelter Syndrome): Presence of an extra X chromosome in males.
47, XXX (Triple X Syndrome): Presence of an extra X chromosome in females.
Variants like 47, XXYY or 47, XXXY are also included.
Diverse Effects: These chromosomal disorders may not always result in overt discrepancies between internal and external genitalia. However, they can significantly impact:
Sex hormone levels.
Overall sexual development and function.
The total count and arrangement of sex chromosomes.
SIGNS & SYMPTOMS OF INTERSEX CONDITIONS
The presentation of intersex conditions is diverse, with signs and symptoms varying based on the specific underlying cause.
Ambiguous Genitalia at Birth: At birth, the external sex organs may not conform to typical male or female appearances, making gender assignment unclear.
Micropenis: In individuals assigned male at birth, a penis that is significantly smaller than average can be observed. This may be due to hormonal or genetic factors.
Clitoromegaly (Enlarged Clitoris): In individuals assigned female at birth, the clitoris may be noticeably larger than is typical, often caused by prenatal hormonal influences.
Partial Labial Fusion: Individuals assigned female at birth may present with a partial joining or adhesion of the labia, the skin folds around the vaginal opening.
Apparent Undescended Testes (Potentially Ovaries) in Assigned Males: What appears to be undescended testes in a newborn assigned male, could in fact be ovaries, highlighting a discordance between external presentation and internal anatomy.
Labial or Inguinal Masses (Potentially Testes) in Assigned Females: Lumps or swellings felt in the labial or groin area of a newborn assigned female, may unexpectedly be testes, illustrating complexities in organ development.
Hypospadias: In assigned males, the urethral opening is not located at the tip of the penis. In assigned females, the urethra might open into the vagina rather than in its usual position.
Atypical Genital Appearance at Birth: The overall appearance of the genitals at birth might deviate from typical male or female characteristics, leading to uncertainty in gender assignment.
Electrolyte Imbalances: Disruptions in the balance of essential electrolytes in the body may occur, requiring careful monitoring and medical intervention.
Delayed or Absent Puberty: The onset of puberty may be delayed or fail to occur altogether, impacting the development of expected secondary sexual characteristics.
Unexpected Pubertal Changes: During puberty, individuals might experience developmental changes that are not typical for their assigned sex, causing further complexity in understanding their sexual development.
Underdeveloped Secondary Sexual Characteristics: Development of typical secondary sexual characteristics, such as breast growth in females or facial hair in males, might be incomplete or atypical.
Infertility: Some intersex conditions can result in reduced or absent fertility due to irregularities in the development of reproductive organs or hormonal imbalances affecting the production of sperm or eggs.
Atypical Pubic Hair Patterns: The growth pattern or presence of pubic hair might be unusual or absent, contributing to the diverse presentations of intersex traits.
Urinary or Reproductive System Issues: Complications affecting the urinary or reproductive tracts may be associated with intersex conditions, potentially including structural abnormalities or difficulties with reproduction.
Gender Dysphoria: Individuals might experience distress or discomfort related to the gender they were assigned at birth, potentially leading to concerns about gender identity and a need for psychological support.
Hormonal Irregularities: Variations in hormone levels can manifest in diverse symptoms such as mood changes, fatigue, or irregular menstrual cycles in those who menstruate, depending on the specific intersex variation.
Chromosomal Variations: Some intersex presentations are associated with chromosomal patterns that are not the typical XX or XY configurations, adding to the broad spectrum of intersex experiences.
Psychosocial Challenges: Individuals with intersex conditions may encounter unique psychosocial challenges related to societal misunderstandings, self-perception, social acceptance, and the process of self-discovery, highlighting the importance of supportive and understanding environments.
Skeletal and Muscular Differences: Variations in skeletal and muscular development may be observed, potentially affecting overall body structure and physical capabilities.
Emotional and Mental Well-being: The emotional and mental health of intersex individuals can be significantly influenced by societal attitudes, the process of disclosing their intersex status, and effectively managing their unique life experiences.

Diagnosis and Investigations
To diagnose intersex conditions, a range of investigations may be employed:
Chromosomal Analysis: This test is conducted to analyze an individual’s chromosomes. It determines if the chromosomal arrangement is typical (XX for females, XY for males) or if there are any variations. This analysis is crucial for identifying intersex conditions that are rooted in chromosomal differences.
Hormone Level Assessment (e.g., Testosterone): Measuring the levels of specific hormones, such as testosterone, provides valuable information about the endocrine system. Abnormal hormone levels can indicate imbalances that are influencing sexual development and may point towards an intersex condition.
Hormone Stimulation Testing: These dynamic tests evaluate how the body responds to stimulation with specific hormones. They assess the functional capacity of endocrine glands to produce and regulate hormones that are essential for normal sexual development. The results can help identify hormonal pathways that are not working as expected.
Electrolyte Balance Evaluation: Electrolyte tests are used to check the levels of vital minerals in the body. Imbalances in these electrolytes can be indicative of certain intersex conditions, particularly those affecting adrenal gland function, and need to be identified for appropriate management.
Targeted Molecular Genetic Testing: This advanced testing involves examining the individual’s genetic material at a detailed, molecular level. It is used to pinpoint specific genetic changes or mutations that are known to be associated with various intersex conditions, providing a precise genetic diagnosis.
Endoscopic Examination (Vaginal/Cervical Assessment): An endoscopic exam, using a small camera, may be performed to visually inspect and confirm the presence or absence of internal female reproductive structures like the vagina or cervix. This helps in assessing internal anatomy.
Imaging with Ultrasound or MRI (Internal Organ Evaluation): Medical imaging techniques, such as ultrasound or Magnetic Resonance Imaging (MRI), are utilized to create detailed images of the internal organs, including the uterus and gonads. This allows healthcare providers to assess the presence, absence, or development of internal sex organs and related structures.
Challenges Faced by Intersex People:
I. Social Stigma: Individuals with intersex variations are often subjected to intense stigma. This is fueled by societal misunderstandings and a general lack of awareness regarding diverse sex development. This stigma can significantly harm their mental health and overall well-being.
II. Discrimination from Initial Identification: From the moment an intersex trait is recognized, whether at birth or later in life, individuals may encounter discrimination. This prejudice can manifest in various forms, impacting their sense of self-worth, acceptance, and belonging within their communities.
III. Risk of Infanticide: Tragically, in some cultures and due to severe misinformation, intersex infants are at risk of infanticide. This constitutes a grave threat to the lives of newborns who are born with intersex traits.
IV. Parental Abandonment: The discovery of an intersex condition in a child can be deeply distressing for parents. In extreme and unfortunate cases, parental distress can lead to abandonment, resulting in significant and long-lasting emotional and psychological damage for the child.
V. Family Stigma: The stigma experienced by intersex individuals often extends to their families. Societal ignorance and prejudice can lead to families being judged, isolated, and excluded within their communities simply for having an intersex family member.
VI. Inequitable Treatment: Intersex individuals frequently face unequal treatment in numerous areas of life. This can include discrimination within healthcare systems, educational institutions, and the workplace, leading to reduced opportunities and unfair access to essential services.
VII. Mental Health Concerns: The combined pressures of societal prejudice, discriminatory practices, and potentially intrusive medical interventions can contribute to significant mental health challenges for intersex people. Access to dedicated and sensitive mental health support is crucial for their emotional resilience.
VIII. Lack of Educational Inclusivity: Educational systems often fail to adequately address intersex variations within curricula. This lack of inclusive education can foster misunderstanding, bullying, and a lack of empathy among peers and educators alike.
X. Inadequate Healthcare Access: Many intersex individuals struggle to access healthcare professionals who are knowledgeable, compassionate, and competent in intersex health. This inadequacy in medical care can result in both physical and emotional distress, underscoring the critical need for better-informed healthcare providers.
XI. Limited Public Awareness and Advocacy: Widespread public ignorance about intersex variations is a core contributor to the challenges faced by this population. Amplified public awareness campaigns and dedicated advocacy efforts are essential to cultivate greater understanding, promote tolerance, and ensure equal rights and protections for intersex individuals.
XII. Social Isolation and Loneliness: The compounding effects of societal stigma, misunderstanding, and discrimination can lead to profound feelings of isolation and loneliness among intersex individuals, impacting their social connections and overall quality of life.
Medical Management for Intersex Individuals:
Diagnosis and Comprehensive Assessment:
Chromosomal Analysis: Perform genetic testing to analyze the individual’s chromosome structure (e.g., XX, XY, or variants). This helps to understand the genetic basis of the intersex condition.
Hormone Level Evaluation: Measure key hormone levels, such as testosterone and estrogen, along with other relevant hormones, to assess the endocrine profile. Hormone levels are vital for understanding hormonal influences on development.
Medical Imaging: Employ imaging techniques like ultrasound or MRI to visualize the internal reproductive organs. This allows for detailed assessment of internal anatomy and identification of any structural variations.
Hormone Therapy Interventions:
Gender-Affirming Hormone Administration: Prescribe and administer hormones, either to promote feminization or masculinization. This treatment is guided by the individual’s self-identified gender and aims to develop secondary sexual characteristics that are congruent with their gender identity.
Psychological and Social Support Services:
Mental Health Counseling: Offer access to professional psychological counseling. This is essential to address the emotional challenges that intersex individuals may face, to foster a positive self-concept, and to develop effective coping strategies for navigating life as an intersex person.
Peer Support Networks: Facilitate connections with intersex support groups. These groups provide valuable peer-to-peer support, allowing individuals to share experiences, build community, and reduce feelings of isolation.
Prenatal and Family Counseling Resources:
Genetic Counseling for Families: Provide genetic counseling services specifically for parents and families. This counseling helps families understand the specific intersex condition, discuss potential health considerations, and explore available management and support options in a supportive environment.

Surgical Management for Intersex Individuals:
Genital Reconstructive Surgery:
Feminizing Procedures: For individuals who are assigned female and seeking feminization, surgical options encompass vaginoplasty (creating a vagina), clitoroplasty (reshaping the clitoris to a more typical female appearance), and labiaplasty (altering the labia).
Masculinizing Procedures: For individuals assigned male and pursuing masculinization, surgical interventions may include phalloplasty (constructing a penis) and scrotoplasty (constructing a scrotum).
Gonadectomy (Gonad Removal):
Addressing Health Risks: Removal of the gonads (testes or ovaries) may be considered to mitigate potential risks like gonadal cancer or to manage hormonal imbalances. The optimal timing of a gonadectomy is determined based on a careful evaluation of each individual’s specific health profile and needs.
Corrective Surgical Interventions:
Hypospadias Repair: Surgical correction for hypospadias aims to relocate the urethral opening to the typical position at the tip of the penis.
Vaginal or Penile Reconstruction: Surgeries can be customized to address a range of specific anatomical variations, facilitating the construction or refinement of vaginal or penile structures.
Breast and Chest Gender-Affirming Surgeries:
Supporting Gender Affirmation: To assist individuals in aligning their physical presentation with their gender identity, breast augmentation (for feminization) or chest reconstruction (often referred to as “top surgery” for masculinization) may be offered as part of a broader gender-affirming care plan.
Nursing Care for Intersex Individuals:
Communication and Education Strategies:
Promote Open Dialogue: Nurses should establish and maintain open communication channels to encourage patients and families to express concerns and ask questions, while providing clear and honest information about medical treatments and procedures.
Provide Comprehensive Patient Education: Nurses play a vital role in educating both individuals and their families. This education should cover the specifics of the intersex condition, available treatment options (both surgical and non-surgical), and essential aspects of postoperative care.
Preoperative Nursing Care:
Offer Emotional Support: Prior to any surgical procedure, provide robust emotional support to alleviate anxieties and address any preoperative concerns the individual or family may have.
Ensure Physical Preparation: Nurses are responsible for ensuring patients and families fully understand preoperative instructions, including fasting guidelines, medication adjustments, and hygiene protocols, to facilitate optimal physical preparation for surgery.
Postoperative Nursing Care:
Effective Pain Management: Diligent monitoring and management of postoperative pain are crucial. Nurses should implement strategies to ensure patient comfort throughout the recovery period, utilizing appropriate pain relief methods.
Provide Wound Care Expertise: Administer meticulous wound care for surgical sites. This includes regular assessment for signs of infection, cleaning and dressing changes, and patient education on proper wound care at home, all aimed at preventing complications and promoting optimal healing.
Sustain Emotional Support: Continue to provide consistent psychological support during the postoperative recovery phase. Nurses should be sensitive to body image concerns that may arise post-surgery and actively foster a positive self-perception and body image in the recovering individual.
Long-Term Follow-Up Care:
Hormone Level Monitoring: Regular monitoring of hormone levels is essential for individuals undergoing hormone therapy. Nurses play a role in scheduling and tracking these tests and communicating results to the medical team for appropriate adjustments to hormone regimens as needed.
Ongoing Psychosocial Support: Recognize that psychosocial needs may evolve over time. Ensure continued access to psychosocial support services to address any ongoing or emerging emotional and mental health needs as the individual navigates life with an intersex condition.
Advocacy, Dignity, and Cultural Competence:
Champion Patient Rights: Nurses are key advocates for the rights and inherent dignity of intersex individuals. This includes promoting care environments that are fully inclusive, respectful, and non-discriminatory.
Ensure Cultural Sensitivity: Deliver nursing care that is culturally competent and sensitive, demonstrating respect for the diverse identities, cultural backgrounds, and lived experiences of intersex individuals and their families.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

