Integrated Management of Childhood Illnesses (IMCI)
Subtopic:
Manage HIV/AIDS using IMCI approach

CHECK FOR HIV EXPOSURE AND INFECTION
It is recommended that all children presenting with specific conditions like pneumonia, ongoing diarrhea, ear drainage, or significant underweight (for their age), and who do not immediately require specialist referral, should be evaluated for possible HIV infection showing symptoms.
Children can contract HIV from their mothers through mother-to-child transmission, which can occur during pregnancy (while in the womb), at the time of birth, or through breastfeeding. Without preventive measures, it is estimated that approximately 30 to 40 percent of infants born to mothers with HIV will also become infected.
Regrettably, for many children who are born with HIV and do not receive treatment, the disease progresses rapidly. The majority of these children will not live to see their fifth birthday, and for many, survival is limited to only a couple of years.
Effective treatments are available that can significantly change the course of HIV infection in children, leading to improved health outcomes and a better quality of life for both the child and their family. Identifying HIV in a child can sometimes be the first indication that a parent may also be living with HIV, highlighting the importance of family-centered care and testing.
ASSESS FOR HIV EXPOSURE AND INFECTION
| Topic | Details |
| ASK | |
| Inquire about the mother’s HIV status to determine the child’s HIV exposure risk. (Positive, Negative, or Unknown); Ask about any history of Tuberculosis (TB) contact | |
| LOOK, FEEL AND DIAGNOSE | |
| Child under 18 months: | |
| If the mother has a confirmed HIV-positive status, perform a DNA PCR test on the infant at 6 weeks of age or upon initial contact; If the mother’s HIV status is uncertain, conduct a rapid antibody test on the mother to evaluate potential HIV exposure; Consider a presumptive diagnosis of HIV infection in children <18 months presenting with: Pneumonia, Oral Candidiasis (thrush), Severe sepsis, Other conditions indicative of AIDS | |
| Child 18 months and older: If the mother’s antibody test result is POSITIVE, the child is considered exposed. Perform an antibody test directly on the child. | |
| Child whose mother is NOT available: Child < 18 months Perform an antibody test on the child. If the antibody test is positive, follow up with a DNA PCR test for confirmation. Child ≥ 18 months Conduct an antibody test to determine the child’s HIV status |
CLASSIFY HIV STATUS
| SIGNS | CLASSIFY AS | TREATMENT |
| Child < 18 months with a POSITIVE DNA PCR test | ||
| Child ≥ 18 months with a POSITIVE Antibody test | CONFIRMED HIV INFECTION | Start Anti-Retroviral Therapy (ART), address existing infections; Start or continue Cotrimoxazole prophylaxis to prevent opportunistic infections; Evaluate the child’s feeding practices and offer appropriate counseling to the mother or caregiver; Provide routine follow-up appointments for growth, nutritional status, developmental milestones, and HIV-related services; Educate caregivers about the importance of treatment adherence; Screen for Tuberculosis (TB) at each visit; For children without TB, start Isoniazid Prophylactic Therapy (IPT) to prevent TB. Monitor for TB development throughout IPT; Administer measles vaccination at 6 and 9 months and provide a booster at 18 months; Conduct monthly follow-up in accordance with national ART guidelines, offering comprehensive HIV management. Refer to national guidelines for HIV care |
| Child<18 months, and: Mother tested positive, AND child’s DNA PCR is negative. OR Mother unavailable; child’s antibody test is positive AND DNA PCR is negative. | HIV EXPOSED | Treat existing infections, counsel the caregiver; Start or continue Cotrimoxazole prophylaxis; Administer Zidovudine and Nevirapine prophylaxis according to national PMTCT guidelines; Evaluate child’s feeding, counsel mother/caregiver; Offer routine follow-up for growth, nutrition, and development; Repeat DNA PCR at 6 months, again at 12 months if negative. If both are negative, repeat antibody test at 18 months; Continue routine care in under-5 clinics; Screen for Tuberculosis (TB) at every visit; Administer measles vaccine at 6 and 9 months, and booster at 18 months; Follow up monthly per national ART guidelines, offering comprehensive HIV management. |
| No test results available for child or mother. AND exhibiting two or more of: Severe pneumonia Oral candidiasis (thrush) Severe Sepsis OR An AIDS-defining condition | SUSPECTED SYMPTOMATIC HIV INFECTION | Treat existing infections, counsel the caregiver; Administer Cotrimoxazole prophylaxis; Administer Vitamin A supplements every 6 months starting at 6 months old; Assess the child’s feeding and provide appropriate counseling to the mother; Test to confirm HIV infection; Refer for further assessment including HIV care/ART; Follow up in 14 days, then monthly for 3 months, then every 3 months, or according to the immunization schedule. |
| Mother’s HIV status is NEGATIVE. OR Mother’s HIV status is POSITIVE, and child is ≥ 18 months with a negative antibody test 6 weeks post-breastfeeding cessation. | HIV NEGATIVE | Address presenting conditions based on IMNCI and national guidelines; Counsel the mother on feeding practices and her own health. |
THEN CHECK FOR TB
| Topic | Details |
| ASK | |
| For symptoms suggestive of TB | Has the child been coughing for 14 days or longer?; Has the child had persistent fever for 14 days or longer?; Has the child had poor weight gain in the last month? |
| History of contact | Has the child had contact with a person with Pulmonary Tuberculosis or chronic cough? |
| LOOK AND FEEL | |
| Physical signs of TB | Swellings in the neck or armpit; Swelling on the back; Stiff neck; Persistent wheeze not responding to bronchodilators. |
| Sample Collection | Collect sample for GeneXpert or smear microscopy. |
| Further testing(If available for further investigations) | Send the child for laboratory tests (GeneXpert or smear microscopy) and/ or Chest X-Ray. |
CLASSIFY
| SIGNS | CLASSIFY AS | TREATMENT |
| Two or more of the following in HIV Negative child AND one or more of the following in HIV Positive child: | ||
| At least two symptoms suggestive of TB; Positive history of contact with a TB case; Any physical signs suggestive of TB; OR A positive GeneXpert or smear microscopy test | TB | Initiate TB treatment; Treat, counsel, and follow up any co-infections; Inquire about the caregiver’s health and treat as necessary; Link the child to the nearest TB clinic for further assessment and ongoing follow-up; If GeneXpert or smear microscopy test is unavailable or negative, refer for further assessment. |
| Positive history of contact with a TB case and NO other TB symptoms or signs listed above | TB EXPOSURE | Start Isoniazid at 10mg/kg for 6 months; Treat, counsel, and follow up existing infections; Inquire about the caregiver’s health and treat as necessary; Link child to the nearest TB clinic. |
| NO TB symptoms or signs | NO TB | Treat, counsel, and follow up existing infections; Start Isoniazid in HIV positive child above 1 year at 10mg/kg for 6 months. |
THEN CHECK THE CHILD’S IMMUNIZATION AND VITAMIN A STATUS
Immunization Schedule
Refer to National Guidelines in the Child Health Card/Mother Baby Passport
| Age | Vaccine |
| Birth | BCG* , OPV-0 |
| 6 weeks | DPT+HepB+HiB, OPV-1, RTV1, PCV1 |
| 10 weeks | DPT+HepB+HiB, OPV-2, RTV2, PCV2 |
| 14 weeks | DPT+HepB+HiB, OPV-3, IPV, RTV3, PCV3 |
| 9 months | Measles |
BCG: Bacillus Calmette-Guérin (given at birth)
OPV: Oral Polio Vaccine
DPT: Diphtheria, Pertussis, Tetanus
HepB: Hepatitis B
HiB: Haemophilus influenzae type b
RTV: Rotavirus Vaccine
PCV: Pneumococcal Conjugate Vaccine
IPV: Inactivated Polio Vaccine
VITAMIN A SUPPLEMENTATION
Give every child a dose of Vitamin A every six months from the age of 6 months. Record the dose on the child’s chart.
ROUTINE DEWORMING TREATMENT
Give every child mebendazole every six months from the age of 1 year. Record the dose on the child’s chart.
Managing HIV/AIDS with the IMCI Approach
It is recommended that all children under the age of 5 who are diagnosed with HIV infection should commence Antiretroviral Therapy (ART), regardless of their CD4 count or clinical stage of the disease.
Critical Note: If a child presents with any general danger signs or is classified as having a severe condition based on IMCI assessments, URGENT REFERRAL is the priority. ART initiation is not an emergency intervention and should be initiated only after the child’s condition is stabilized.
Steps for Initiating ART in Children:
STEP 1: Confirming HIV Infection in the Child
Child Under 18 Months Old:
HIV infection is definitively confirmed through a positive virological test, specifically a Polymerase Chain Reaction (PCR) test. This test directly detects the virus’s genetic material.
Child Over 18 Months Old:
Confirmation requires two positive results from distinct serological tests. Serological tests detect antibodies to HIV in the blood.
Further Confirmatory Testing:
Submit any additional tests that are required to definitively confirm the HIV diagnosis according to national guidelines.
Discordant Results:
If test results are conflicting or unclear, refer the child to a specialist or higher-level facility for expert evaluation.
Proceed to Step 2:
If HIV infection is confirmed and the child is currently in a stable medical condition, proceed to STEP 2.
STEP 2: Assessing Caregiver Capacity to Administer ART
Caregiver Readiness Assessment:
Evaluate the caregiver’s willingness and ability to consistently administer ART medication to the child. This is crucial for treatment success.
Support Network:
Ideally, ensure the caregiver has disclosed the child’s HIV status to another responsible adult who can provide support with ART administration, or that the caregiver is connected with a peer support group. Support systems are vital for long-term adherence.
Caregiver Able to Administer ART: Proceed to STEP 3
Caregiver Unable to Administer ART:
Classify the child as CONFIRMED HIV INFECTION, but NOT CURRENTLY ON ART.
Provide thorough counseling and support to the caregiver to address barriers and build capacity for ART administration.
Establish a plan for regular follow-up to monitor the situation and provide ongoing support.
Transition to STEP 3 once the caregiver indicates willingness and demonstrates the ability to initiate ART.
STEP 3: Determining Facility Readiness for ART Initiation
Referral Criteria:
If the child’s weight is less than 3 kg, refer for ART initiation to a facility equipped to manage very low-weight infants on ART.
If the child has active Tuberculosis (TB), refer for ART initiation to ensure integrated management of both conditions, which may require specialized services.
Facility-Based Initiation:
If the child weighs 3 kg or more and does not have TB, proceed to STEP 4 for ART initiation at your current facility.
STEP 4: Recording Baseline Information on the Child’s HIV Treatment Card
Document Baseline Data: Thoroughly record the following baseline information on the child’s dedicated HIV treatment card:
Weight and Height: Record precise measurements to track growth and nutritional status.
Pallor: Note the presence or absence of pallor (pale skin), as it can indicate anemia.
Feeding Problems: Document any reported or observed feeding difficulties.
Laboratory Results (if available): Record any existing laboratory results, including:
Hemoglobin (Hb): To assess for anemia.
Viral Load: To measure the amount of HIV virus in the blood (if available).
CD4 Count and Percentage: To assess the child’s immune system status (if available).
Required Laboratory Tests: Send requests for any essential laboratory tests that are still needed according to national guidelines.
Do Not Delay: Do not postpone ART initiation while waiting for laboratory results. Proceed to STEP 5.
STEP 5: Initiating ART, Cotrimoxazole Prophylaxis, and Routine Treatments
Initiate ART Regimen:
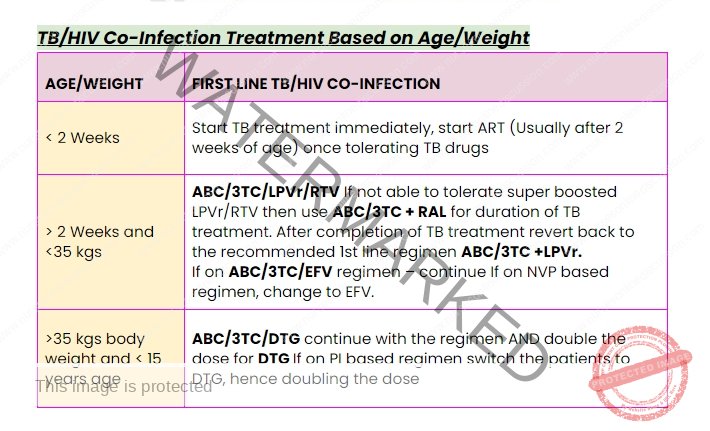
Children up to 3 Years Old: Commence ART with a recommended first-line regimen, typically including: Abacavir (ABC) or Zidovudine (AZT) + Lamivudine (3TC) + Lopinavir/ritonavir (LPV/r) or another nationally recommended first-line regimen for this age group.
Children 3 Years or Older: Commence ART with a recommended first-line regimen, typically including: Abacavir (ABC) + Lamivudine (3TC) + Efavirenz (EFV) or another nationally recommended first-line regimen for this age group.
Administer Cotrimoxazole Prophylaxis: Start daily cotrimoxazole preventive therapy to protect against opportunistic infections, particularly Pneumocystis jirovecii pneumonia.
Provide Other Routine Treatments: Ensure the child receives other essential routine treatments, including:
Vitamin A Supplementation: Administer Vitamin A according to national guidelines.
Immunizations: Ensure the child is up-to-date with all recommended immunizations as per the national immunization schedule.
Regular Follow-Up: Establish a schedule for regular follow-up appointments based on national guidelines to monitor treatment effectiveness, adherence, and the child’s overall health and development.
Recommended First-Line ARV Regimens
| Patient Category | Indication | ARV Regimen |
|---|---|---|
| Adults and Adolescents (aged 10 and above) | Initiating ART | TDF + 3TC + EFV |
| Alternative Regimens | TDF + 3TC + DTG (Contraindications for EFV) | |
| ABC + 3TC + DTG (Contraindications for TDF) | ||
| Pregnant or Breastfeeding Women | Initiating ART | TDF + 3TC + EFV |
| Alternative Regimen | ABC + 3TC + ATV/r (Contraindications for TDF or EFV) | |
| Children (3 to <10 years) | Initiating ART | ABC + 3TC + EFV |
| Alternative Regimen | ABC + 3TC + NVP (Contraindications for EFV) | |
| Children Under 3 Years | Initiating ART | ABC + 3TC + LPV/r |
| Alternative Regimen | AZT + 3TC + LPV/r (Hypersensitivity reaction to ABC) |
Second- and Third-Line ART Regimens
| Population | Patients Failing First-Line Regimens | Second-Line Regimens | Third-Line Regimens |
|---|---|---|---|
| Adults, Pregnant and Breastfeeding Women, Adolescents | TDF + 3TC + EFV | AZT + 3TC + ATV/r (recommended) or AZT + 3TC + LPV/r (alternative) | All 3rd line regimens guided by resistance testing |
| TDF + 3TC + DTG | TDF + 3TC + ATV/r (recommended) or TDF + 3TC + LPV/r | If not exposed to INSTIs: DRV/r + DTG ± 1-2 NRTIs | |
| ABC + 3TC + DTG | ABC + 3TC + EFV | If exposed to INSTIs: DRV/r + ETV ± 1-2 NRTIs | |
| ABC/3TC/NVP | TDF/3TC/NVP | ||
| AZT/3TC/NVP | AZT/3TC/EFV | ||
| Children (3–<10 years) | ABC + 3TC + EFV | AZT + 3TC + LPV/r | For children above 6 years, and prior exposure to INSTIs, DRV/r ± 1-2 NRTIs |
| ABC + 3TC + NVP | AZT + 3TC + NVP | ||
| ABC + 3TC + LPV/r | AZT + 3TC + LPV/r | DRV/r + RAL + 2 NRTIs | |
| Children Under 3 Years | ABC + 3TC + LPV/r pellets | AZT + 3TC + RAL | Optimize regimen using genotype profile |
| AZT + 3TC + LPV/r pellets | ABC + 3TC + RAL | ||
| AZT + 3TC + NVP | ABC + 3TC + LPV/r |
Principles for Selecting Antiretroviral (ARV) Regimens:
When choosing an ARV regimen, several key factors guide the selection process to ensure optimal treatment outcomes and patient well-being:
Minimized Toxicity Profile: Prioritize regimens known to have fewer adverse effects to enhance patient comfort and long-term adherence to therapy.
Improved Acceptability and Reduced Dosage Burden: Select medications that are easier for patients to take, considering factors like taste (palatability) and the number of pills required daily (pill burden), to promote consistent adherence.
Enhanced Treatment Durability and Effectiveness: Favor regimens demonstrated to maintain viral suppression over time (durability) and achieve high rates of viral suppression (efficacy) to prevent disease progression and drug resistance.
Strategic Sequencing for Future Treatment Options: Choose initial regimens with consideration for preserving other drug classes and formulations for use in second-line regimens should treatment adjustments become necessary later.
Consistency Across Diverse Populations: Aim for treatment strategies that can be effectively and safely used across different age groups and patient demographics to simplify treatment guidelines and implementation.
Cost-Effectiveness: Consider the financial implications of different regimens to ensure treatment is affordable and accessible, supporting wider program sustainability.
Simplified Regimen Recommendation: Strive to identify regimens that can be recommended for the majority of individuals living with HIV (PLHIV), streamlining treatment algorithms and clinical decision-making.
Reasons for Considering Alternative ARV Regimens:
Specific clinical situations may necessitate the use of alternative ARV regimens to address contraindications or limitations associated with standard first-line options. Examples include:
Tenofovir Disoproxil Fumarate + Lamivudine + Dolutegravir (TDF+3TC+DTG): Used when Efavirenz (EFV) is contraindicated. This combination provides an effective alternative when EFV cannot be used due to factors like potential neuropsychiatric side effects or pregnancy considerations.
Abacavir + Lamivudine + Dolutegravir (ABC+3TC+DTG): Chosen when Tenofovir Disoproxil Fumarate (TDF) is contraindicated. This regimen is suitable when TDF is not appropriate, such as in patients with kidney issues or bone density concerns.
Abacavir + Lamivudine + Atazanavir/Ritonavir (ABC+3TC+ATV/r): Considered when there are contraindications to both TDF and EFV. This offers an option when neither TDF nor EFV can be used, utilizing a protease inhibitor-based approach.
Abacavir + Lamivudine + Nevirapine (ABC+3TC+NVP): May be used when Efavirenz (EFV) is contraindicated in children aged 3 to under 10 years. Nevirapine serves as an alternative NNRTI in younger children where EFV may not be preferred or appropriate.
Zidovudine + Lamivudine + Lopinavir/ritonavir (AZT+3TC+LPV/r): Considered in cases of a rare hypersensitivity reaction to Abacavir (ABC). This regimen substitutes AZT for ABC when ABC cannot be tolerated due to an allergic reaction.
Important Considerations:
Dolutegravir (DTG) Advantages: DTG is increasingly favored due to its beneficial characteristics, including:
Low Drug Interaction Potential: Reduces the risk of interactions with other medications.
Rapid Viral Suppression: Leads to quicker control of HIV viral load.
High Resistance Barrier: Less prone to the development of drug resistance.
Long Half-Life: Allows for once-daily dosing, improving convenience.
Lower Cost: Often more affordable compared to some other ARV options, enhancing accessibility.
Abacavir + Lamivudine + Efavirenz (ABC+3TC+EFV) as a Once-Daily Regimen: This combination is frequently used for its convenience of once-daily dosing, which can significantly improve patient adherence to treatment.
Lopinavir/ritonavir (LPV/r)-Based Regimens for Young Children: Regimens based on LPV/r are often preferred for children under 3 years old due to their favorable safety profile in this age group and their robust barrier to resistance, which is especially important in early treatment.
Key to Abbreviations:
ABC: Abacavir
AZT: Zidovudine
3TC: Lamivudine
LPV/r: Lopinavir/Ritonavir
RTV: Ritonavir
NVP: Nevirapine
EFV: Efavirenz
DTG: Dolutegravir
TDF: Tenofovir Disoproxil Fumarate
RAL: Raltegravir
ATV/r: Atazanavir/Ritonavir
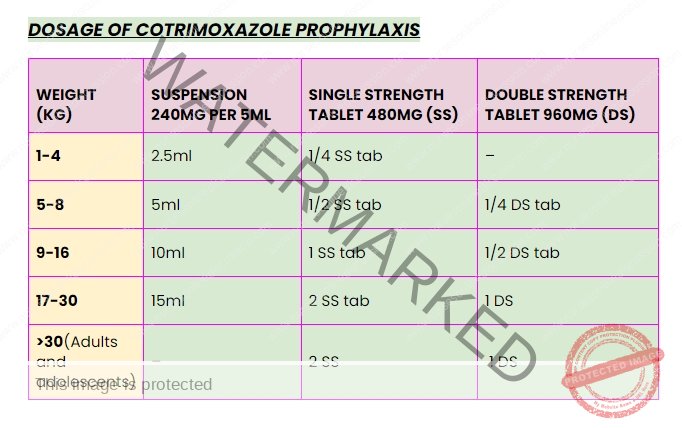
Trimethoprim-sulfamethaxazole dose: 24-30 mg/kg once daily
Oral thrush: Miconazole gel
Cotrimoxazole is still recommended.
Infants/children take time before recovery
Children on LPV/r: continue ritonavir
RAL: consider if unable to tolerate boosted LPV/r
Paediatric ARVs Dosages
| WEIGHT RANGE (KG) | ABACAVIR + LAMIVUDINE (120 mg ABC + 60 mg 3TC) | ZIDOVUDINE + LAMIVUDINE (60 mg ZDV + 30 mg 3TC) | EFAVIRENCE (EFV) (Once Daily 200mg tabs) | LAMIVUDINE + ZIDOVUDINE (Twice Daily 200mg tabs) |
| 3 – 5.9 | 0.5 tab | 1 tab | – | – |
| 6 – 9.9 | 1 tab | 1.5 tabs | – | – |
| 10 – 13.9 | 1 tab | 2 tabs | 1 tab | 1.5 tabs |
| 14 – 19.9 | 1.5 tabs | 2.5 tabs | 1.5 tabs | + 1 tab in AM & 0.5 tab in PM |
| 20 – 24.9 | 2 tabs | 3 tabs | 1.5 tabs | 1 tab in AM & 0.5 tab in PM |
| 25 – 34.9 | 300 mg ABC + 150 mg 3TC | 300 mg ZDV + 150 mg 3TC | 2 tabs | 1 tab in AM & 0.5 tab in PM |
Manage Side Effects of ARV Drugs
| SIGNS OR SYMPTOMS | APPROPRIATE CARE RESPONSE |
| Yellow eyes (jaundice) or abdominal pain | Stop drugs and REFER urgently |
| Rash | If on abacavir, assess carefully. Call for advice. If severe, generalized, or associated with fever or vomiting: stop drugs and REFER urgently |
| Nausea | Advise drug administration with food. If it persists for more than 2 weeks or worsens, call for advice or refer. |
| Vomiting | If medication is seen in vomitus, repeat the dose. If vomiting persists, bring the child to the clinic. REFER urgently if vomiting everything or associated with severe symptoms. |
| Diarrhoea | Assess, classify, and treat using diarrhoea charts. Reassure that it may improve in a few weeks. Follow up as per chart booklet. Call for advice or refer if not improved after two weeks. |
| Fever | Assess, classify, and treat using fever chart. |
| Headache | Give paracetamol. If on efavirenz, reassure that it is common and usually self-limiting. Call for advice or refer if it persists for more than 2 weeks or worsens. |
| Sleep disturbances, nightmares, anxiety | Due to efavirenz, Administer at night on an empty stomach with low-fat foods. Call for advice or refer if it persists for more than 2 weeks or worsens. |
| Tingling, numb, or painful feet or legs | If new or worse on treatment, call for advice or refer. |
| Changes in fat distribution | Consider switching from stavudine to abacavir, consider viral load. Refer if needed. |
GIVE FOLLOW – UP CARE FOR ACUTE CONDITIONS
Utilize the follow-up guidance corresponding to the child’s initial classifications during return visits.
For any new complaints, conduct a complete assessment, classify, and manage them following the “ASSESS AND CLASSIFY” chart.
PNEUMONIA
After 2 Days:
Re-evaluate for Danger Signs: Assess for general danger signs.
Reassess Respiratory Status: Examine the child for cough or breathing difficulty.
Inquire about Improvement:
Is the breathing rate becoming slower?
Is the fever reducing?
Is the child’s appetite improving?
Treatment:
Danger Signs Present: If any general danger sign is identified, immediately administer a dose of a second-line antibiotic, and then URGENTLY ADMIT or REFER to hospital.
No Improvement in Key Symptoms: If chest in-drawing, rapid breathing rate, fever, or poor eating persist, transition to a second-line antibiotic and ADMIT or REFER. (Referral is especially important if the child has a history of measles in the last 3 months or has confirmed/suspected HIV infection).
Positive Signs of Recovery: If breathing is slower, fever is reduced, and appetite is better, continue the initial antibiotic course to complete the full 5-day treatment duration.
WHEEZING
After 2 Days:
Check for Complications: Assess for general danger signs or chest in-drawing.
Reassess Respiratory Condition: Evaluate the child’s cough and breathing difficulty.
Inquire about Symptom Changes:
Is the breathing rate becoming slower?
Is wheezing still present?
Is the child’s appetite improving?
For Children Under 1 Year:
Wheezing Plus Complicating Signs: If wheezing is accompanied by any general danger sign, stridor in a calm state, chest in-drawing, rapid breathing, or poor feeding:
Administer an intravascular or intramuscular antibiotic dose.
Then URGENTLY ADMIT or REFER to the hospital.
Improved Condition: If wheezing is absent, breathing is slower, and appetite is better:
Continue the prescribed treatment regimen for a total of 5 days.
For Children Over 1 Year:
Wheezing Plus Complicating Signs: If wheezing is present alongside any general danger sign, stridor in a calm state, chest in-drawing, rapid breathing, or poor feeding:
Administer an intravascular or intramuscular antibiotic dose.
Then URGENTLY ADMIT or REFER to the hospital.
No Improvement in Breathing/Eating: If breathing rate and appetite show no improvement:
Change to a second-line antibiotic and URGENTLY ADMIT or REFER to the hospital.
Persistent Wheezing: If wheezing continues:
Maintain the oral bronchodilator therapy.
Positive Signs of Recovery: If breathing is slower, wheezing is absent, and appetite is better:
Continue the treatment plan for the full 5-day course.
Unilateral Wheezing and Poor Bronchodilator Response: If wheezing is localized to one side and not responding to bronchodilators, consider Tuberculosis (TB) as a potential cause and investigate further.
PERSISTENT DIARRHEA
After 5 Days:
Inquire about Diarrhea Status:
Has the diarrhea resolved?
How many loose stools is the child experiencing daily?
Treatment:
Ongoing Diarrhea: If diarrhea persists (still 3 or more loose stools daily):
Perform a complete reassessment of the child’s condition.
Provide any necessary treatments based on the reassessment findings.
Then REFER to the hospital for further management.
Diarrhea Resolution: If diarrhea has ceased (fewer than 3 loose stools per day):
Advise the caregiver to follow standard age-appropriate feeding recommendations.
Instruct them to provide one extra meal per day for a month to aid recovery.
Continue Zinc sulfate supplementation for a total of 10 days.
Note: Dietary management is crucial in managing persistent diarrhea.
DYSENTERY
After 2 Days:
Reassess Diarrhea: Evaluate the child’s diarrhea status, as per the “ASSESS & CLASSIFY” chart.
Inquire about Symptom Changes:
Are there fewer stools being passed?
Is there less blood present in the stool?
Is the fever decreasing?
Is abdominal pain reducing?
Is the child’s appetite improving?
Treatment:
Dehydration Present: If the child is dehydrated, manage dehydration based on its classification.
Worsening Symptoms: If stool frequency, blood in stools, fever, abdominal pain, or eating is worsening:
ADMIT or REFER to the hospital.
Condition Unchanged: If the condition remains the same:
Add Metronidazole to the current treatment regimen for a 5-day course.
Advise the caregiver to continue Ciprofloxacin and Zinc and return for review in 2 days.
Exceptions requiring immediate ADMISSION or REFERRAL:
Children younger than 12 months.
Children who were dehydrated at the initial visit.
Children with recent measles (within the last 3 months).
Improving Condition: If there are fewer stools, less blood, reduced fever and abdominal pain, and improved appetite:
Continue Ciprofloxacin and Zinc sulfate treatment until the course is completed.
UNCOMPLICATED MALARIA
If Fever Persists After 3 Days or Returns Within 14 Days:
Full Reassessment Needed: Perform a complete reassessment of the child, referring to the “ASSESS & CLASSIFY” chart.
Evaluate for Other Fever Causes: Investigate for alternative reasons for the persistent or recurrent fever.
Treatment:
Danger Signs or Stiff Neck Present: If any general danger sign or stiff neck is found, manage as VERY SEVERE FEBRILE DISEASE.
Fever Due to Other Cause: If the fever is attributed to a condition other than malaria, provide appropriate treatment for that condition.
Malaria Confirmed and Apparent Cause: If malaria is confirmed by testing and is the apparent cause of ongoing fever:
Administer oral DIHYDROARTEMISININ-PIPERAQUINE (DHA-PPQ).
Give Paracetamol for fever management.
For children under 5 kg who receive DHA-PPQ, conduct further assessment.
Advise caregiver to return again in 3 days if fever continues.
If fever has been present every day for 7 days, refer for expert evaluation.
FEVER – NO MALARIA
If Fever Persists After 3 Days:
Complete Reassessment Required: Conduct a thorough reassessment of the child, using the “ASSESS & CLASSIFY” chart.
Assess for Other Fever Origins: Determine if there are alternative causes for the ongoing fever.
Treatment:
Danger Signs or Stiff Neck Present: If any general danger sign or stiff neck is identified, manage as VERY SEVERE FEBRILE DISEASE.
Fever Caused by Another Condition: If the fever is due to a condition other than malaria, administer suitable treatment for that condition.
Malaria as Apparent Cause: If malaria is deemed the most likely cause of fever:
Treat with the recommended first-line oral antimalarial medication.
Administer Paracetamol for fever control.
Advise the caregiver to return in 3 days if the fever continues.
If fever has been present daily for 7 days, refer for further assessment.
Persistent Fever, Cough, and Reduced Playfulness: If fever, cough, and decreased activity persist despite other treatments, evaluate for potential TB.
EYE OR MOUTH COMPLICATIONS OF MEASLES
After 2 Days:
Examine Eyes and Mouth:
Check for redness and pus discharge from the eyes.
Evaluate the condition of mouth ulcers.
Assess breath odor for foul smell.
Treatment for Eye Infection:
Pus Discharge Present: If pus is still draining from the eye, inquire about the caregiver’s treatment methods.
If treatment was appropriate, REFER to the hospital.
If treatment was incorrect, educate the caregiver on the correct method.
Pus Resolved, Redness Remains: If pus has cleared but eye redness persists, continue the current treatment.
No Pus or Redness: If both pus and redness are absent, discontinue eye infection treatment.
Treatment for Mouth Ulcers:
Worsening Ulcers or Foul Odor: If mouth ulcers are worsening, or there is a very bad odor from the mouth, REFER to the hospital.
Ulcers Stable or Improving: If mouth ulcers are the same or improving, continue using half-strength Gentian Violet or Nystatin for a total of 5 days.
Treatment for Thrush:
Thrush Worsening: If thrush is getting worse, confirm that the treatment is being administered correctly.
Swallowing Difficulty: If the child has trouble swallowing, REFER to the hospital.
Thrush Stable or Improving and Good Feeding: If thrush is neither worse nor better and the child is feeding well, continue Nystatin for a full 7-day course.
Persistent or Worsening Thrush: If thrush does not improve or worsens, consider the possibility of symptomatic HIV infection.
EAR INFECTION
After 5 Days:
Reassess Ear Problem: Re-evaluate the ear condition, referring to the “ASSESS & CLASSIFY” chart.
Measure Temperature: Check the child’s body temperature.
Treatment:
Mastoiditis Signs or High Fever: If there is tender swelling behind the ear or a high temperature (38.5°C or higher), URGENTLY ADMIT or REFER to the hospital.
Acute Ear Infection: If ear pain or discharge continues:
Extend the same antibiotic treatment for another 5 days.
Continue ear drying by wicking.
Schedule a follow-up in 5 days.
Chronic Ear Infection: Confirm the caregiver is correctly performing ear wicking.
Encourage continued wicking.
Review again in 2 weeks.
If ear discharge persists beyond 2 months: ADMIT or REFER to the hospital.
No Pain or Discharge: If there’s no ear pain or discharge, commend the caregiver for effective treatment. If the 5-day antibiotic course is not yet completed, advise them to finish the treatment.
FEEDING PROBLEM
After 5 Days:
Reassess Feeding Practices: Re-evaluate feeding, referencing the questions in the “COUNSEL THE MOTHER” section. Inquire about feeding issues identified during the initial visit.
Counsel on Feeding: Counsel the caregiver on any new or ongoing feeding challenges. If significant feeding changes are recommended, schedule a follow-up visit in 5 days.
Very Low Weight for Age: For children with significantly low weight for age, schedule a follow-up 14 days after the initial visit to monitor weight gain.
PALLOR
After 14 Days:
Iron and Folate Supplementation: Provide iron and folate supplements.
Continued Supplementation: Advise the caregiver to return in 14 days for more iron and folate.
Extended Treatment: Continue daily iron and folate supplementation for a total of 2 months.
Persistent Pallor: If palmar pallor remains after 2 months of supplementation, refer for further assessment.
MALNUTRITION
After 14 Days:
Weight Gain Assessment: If the child is gaining weight, encourage the caregiver to continue current feeding practices.
Feeding Counseling: Counsel the caregiver on any identified feeding problems.
SEVERE MALNUTRITION WITHOUT COMPLICATIONS
After 7 Days or During Regular Follow-Up:
Comprehensive Reassessment: Perform a full assessment using the “ASSESS AND CLASSIFY” chart.
Repeat Anthropometric Measurements: Re-measure Weight-for-Height/Length (WFH/L) and Mid-Upper Arm Circumference (MUAC) as done at the initial visit.
Check for Edema: Examine for bilateral pitting edema in both feet.
Appetite Test: Assess appetite in children 6 months and older by offering Ready-to-Use Therapeutic Food (RUTF).
Treatment:
Progression to SEVERE MALNUTRITION WITH COMPLICATIONS: If the child now meets criteria for complicated severe acute malnutrition (WFH/L less than -3 z-scores, MUAC less than 11.5mm, or bilateral edema AND presence of a medical complication, edema worsening, or failed appetite test), URGENTLY REFER to the hospital.
SEVERE MALNUTRITION WITHOUT COMPLICATIONS Persisting: If the child still has uncomplicated severe acute malnutrition (WFH/L less than -3 z-scores, MUAC less than 11.5 mm, or edema but NO medical complication and passed appetite test), continue counseling the caregiver and encourage consistent RUTF feeding. Schedule a follow-up in 7 days.
MODERATE ACUTE MALNUTRITION: If the child has moderate acute malnutrition (WFH/L between -3 and -2 z-scores or MUAC between 11.5 and 12.5 mm), advise the caregiver to continue RUTF, and provide ongoing counseling.
MODERATE ACUTE MALNUTRITION
After 14 Days:
Re-evaluate Nutritional Status: Assess the child using the same anthropometric measurement (WFH/L or MUAC) as at the initial visit.
For WFH/L, weigh, measure height/length, and calculate WFH/L z-score.
For MUAC, measure with a MUAC tape.
Check for Edema: Examine for bilateral pitting edema.
Reassess Feeding: Review feeding practices, using questions from the “COUNSEL THE MOTHER” chart.
Treatment:
No Longer Moderate Acute Malnutrition: If the child no longer meets the criteria for moderate acute malnutrition, praise the caregiver and encourage continued healthy practices.
Still MODERATE ACUTE MALNUTRITION: If the child still has moderate acute malnutrition, counsel the caregiver on any feeding problems identified. Schedule another follow-up in 14 days. Continue bi-weekly follow-ups until the child is feeding well and consistently gaining weight, or their WFH/L is -2 z-scores or greater, or MUAC is 12.5 cm or more.
Evaluate for TB: Assess all children with failure to thrive or growth faltering for possible Tuberculosis.
Referral Consideration: If you anticipate feeding will not improve, or if the child has lost weight or MUAC has decreased, refer the child for specialized care.
HIV EXPOSED & INFECTED CHILDREN
HIV INFECTED CHILD
After 1 Month:
Assess General Condition: Evaluate the child’s overall health status. Perform a complete reassessment.
Treat Any Conditions: Manage any new health conditions found.
Feeding Assessment: Inquire about feeding problems, counsel on any new or ongoing feeding issues.
Caregiver Education: Advise the caregiver to bring the child back if any new illness occurs or if they have concerns.
Counseling and Support: Counsel the caregiver on any other identified problems and ensure access to community support resources. Refer for further psychosocial support/counseling if needed.
Routine Follow-Up: Continue regular follow-up for growth, development, nutrition, immunization, Vitamin A, and deworming.
ART and Cotrimoxazole Adherence: Assess adherence to ART and Cotrimoxazole prophylaxis and provide adherence counseling as needed. Offer or refer the child for comprehensive HIV management and care (including ART) according to national ART guidelines.
Defaulter Tracking: Implement a system for tracking and identifying children who miss appointments or discontinue treatment.
Monthly Follow-Up: Schedule monthly follow-up visits.
HIV EXPOSED CHILD (<18 months): For children tested DNA PCR Negative
After 1 Month:
Assess General Condition: Evaluate the child’s overall health. Perform a complete reassessment.
Feeding and Appetite Assessment: Inquire about feeding problems or poor appetite, counsel the caregiver on any new or persistent feeding issues.
Treat Any Conditions: Manage any health conditions identified.
Cotrimoxazole Prophylaxis: Continue Cotrimoxazole prophylaxis started at 6 weeks and emphasize the importance of adherence.
ARV Prophylaxis: Continue or initiate ARV prophylaxis for a total duration of 12 weeks.
TB Screening: Screen for possible Tuberculosis Disease.
Routine Follow-Up: Continue regular follow-up for growth, development, nutrition, immunization, Vitamin A, and deworming.
Monthly Follow-Up: Schedule monthly follow-up visits up to 24 months of age for HIV-exposed infants.
EID Algorithm: Refer to the Early Infant Diagnosis (EID) algorithm for HIV status confirmation.
HIV Exposed Infant Follow-up Card: Utilize and refer to the HIV exposed infant follow-up card and register for detailed follow-up instructions.
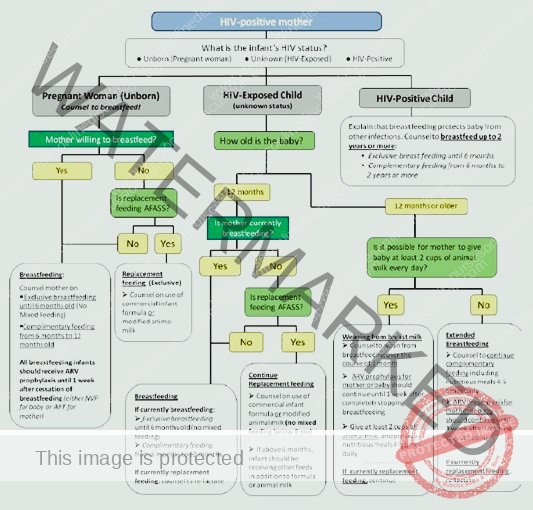
Feeding Counseling: Guidance for Mothers and Caregivers of Infants Under 18 Months
Primary Objectives:
Address Continued HIV Transmission Risk via Breastfeeding: Explain the ongoing possibility of HIV transmission through breast milk and how this can impact the interpretation of infant HIV test results, particularly antibody tests.
Support Informed Feeding Decisions: Provide comprehensive support to mothers as they navigate and decide on the most appropriate feeding method for their infants, respecting their individual circumstances and choices.
Clarify Infant HIV Testing Procedures (Under 18 Months): Ensure mothers fully understand the recommended HIV testing process for infants younger than 18 months, including the timing and types of tests.
Immediate ART for HIV-Positive Infants: If an infant’s HIV test is positive, clearly communicate the critical need to begin Antiretroviral Therapy (ART) without delay.
Initial Postpartum Counseling Topics for Mothers:
Immediately following childbirth, counseling for mothers should include the following key discussions:
Maternal HIV Testing: If HIV testing was not performed during antenatal care, strongly recommend and facilitate HIV testing for the mother soon after delivery to ascertain her HIV status for her health and the baby’s care.
Infant Feeding Practices Education: Provide detailed education on recommended infant feeding practices, specifically tailored to the context of potential HIV exposure.
Infant HIV Testing Schedule: Inform mothers about the recommended timing for infant HIV testing, emphasizing that testing is typically initiated at 6 weeks of age.
Overview of Feeding Recommendations for HIV-Exposed Infants:
Exclusive Breastfeeding for the First 6 Months (HIV-Positive Mothers): Mothers living with HIV are advised to exclusively breastfeed their infants for the first six months of life. Exclusive breastfeeding means giving the infant breast milk only, with no other liquids or solids, except for oral rehydration solution, drops, or syrups of vitamins, minerals, or medicines.
Introduction of Complementary Foods at 6 Months: Starting at 6 months, nutritionally appropriate and safe complementary foods should be introduced to meet the infant’s growing nutritional needs, alongside continued breastfeeding.
Sustained Breastfeeding up to 12 Months: Breastfeeding should be continued for a total duration of 12 months, in combination with complementary foods from 6 months onwards.
Infant Nevirapine (NVP) Prophylaxis During Breastfeeding: Throughout the breastfeeding period, the infant should receive daily Nevirapine (NVP) prophylaxis to reduce the risk of HIV acquisition via breast milk. This daily NVP should continue until one week after breastfeeding is completely stopped.
Safe Breastfeeding Cessation: Breastfeeding should only be discontinued when it is possible to provide a nutritionally adequate, safe, and sustainable diet for the infant without breast milk. When a mother living with HIV decides to stop breastfeeding at any point, the process should be gradual, ideally over a period of approximately one month, to allow the infant to adjust to the dietary change and minimize potential risks.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

