Endocrine Disorders Affecting the Children
Subtopic:
Precocious Puberty
Precocious puberty is defined as the emergence of physical changes related to sex hormones earlier than typically expected. This early development, regardless of the cause, is considered clinically significant and may require medical evaluation.
In simpler terms, precocious puberty is when puberty starts at an unusually young age. For girls, this is generally defined as before the age of 8, and for boys, before the age of 9. It is a condition where the body begins to show signs of sexual maturation earlier than the commonly accepted age range.
The appearance of pubic hair, breast development, or genital changes at a young age can be due to normal, albeit early, maturation. However, it can also be indicative of various underlying medical conditions that require investigation.
Precocious puberty can lead to the capacity for reproduction at a very young age. A notable example of this is Lina Medina, who holds the record as the youngest documented mother, giving birth as early as 5 years and 7 months in some accounts, and 6 years and 5 months in others.
CASE STUDY ANALYSIS
Patient Presentation:
A 3-year-old girl presented with a concerning one-year history of notable breast tissue development and the presence of vaginal discharge. Prior to this, she was reported to be in good health and had reached developmental milestones appropriately. Her medical history was unremarkable for birth trauma, head injuries, encephalitis, headaches, or seizures.
Observed Clinical Findings:
Vaginal Discharge: A white-colored discharge was noted during examination of the vagina.
Breast Examination: Bilateral breast enlargement was evident, described as firm to the touch. The nipples and areolae (the darker skin around the nipples) were also developed in appearance.
Hair Development: Sparse presence of both axillary (underarm) and pubic hair was observed.
Diagnostic Investigations:
Hormone Levels: Laboratory tests revealed elevated levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These hormones play key roles in sexual development and reproduction.
Abdominal Ultrasound: An abdominal ultrasound imaging study showed that both the uterus and ovaries were enlarged, reaching sizes typically seen in adults.
Diagnosis:
Based on the presented clinical picture, the case is indicative of precocious puberty in this young girl. The constellation of symptoms, including premature development of secondary sexual characteristics and hormonal findings, points towards this diagnosis. Further comprehensive evaluation and a tailored management plan are necessary to determine the underlying cause of the hormonal imbalance and to manage its implications for the child’s health and development.
PUBERTY: A Developmental Overview
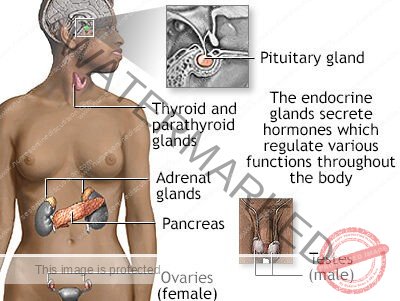
Puberty is the complex biological transition from childhood to young adulthood. It is fundamentally characterized by:
Maturation of Gametogenesis: The development of the ability to produce gametes (sperm in males, eggs in females), marking the onset of reproductive capability.
Gonadal Hormone Secretion: Increased production and release of sex hormones from the gonads (ovaries in females, testes in males). These hormones are critical drivers of pubertal changes.
Secondary Sexual Characteristics Development: The appearance of physical traits that distinguish adult males and females, such as breast development, changes in body hair, and voice deepening.
Reproductive Function Establishment: The maturation of the reproductive system to a functional state, enabling sexual reproduction.
Tanner Staging System for Puberty Assessment
The Tanner staging system, developed by Dr. James Tanner, is a widely accepted and clinically used tool for tracking the progression of puberty. It relies on the observable physical changes that occur during this developmental phase.
Key Terms in Puberty:
Thelarche: Refers to the initiation of breast development in females. This is primarily driven by the effects of estrogen.
Pubarche: Indicates the start of the growth of sexual hair (pubic and axillary hair). This is mainly influenced by androgens (male sex hormones), though present in both sexes.
Menarche: Signifies the onset of menstruation (first menstrual period) in females.
Spermarche: In males, this term denotes the first appearance of spermatozoa (mature sperm cells) in seminal fluid, indicating the start of sperm production.
Gonadarche: Describes the earliest changes in the gonads (ovaries or testes) that mark the beginning of puberty at the hormonal level.
Tanner Stages of Breast Development in Females (Thelarche)
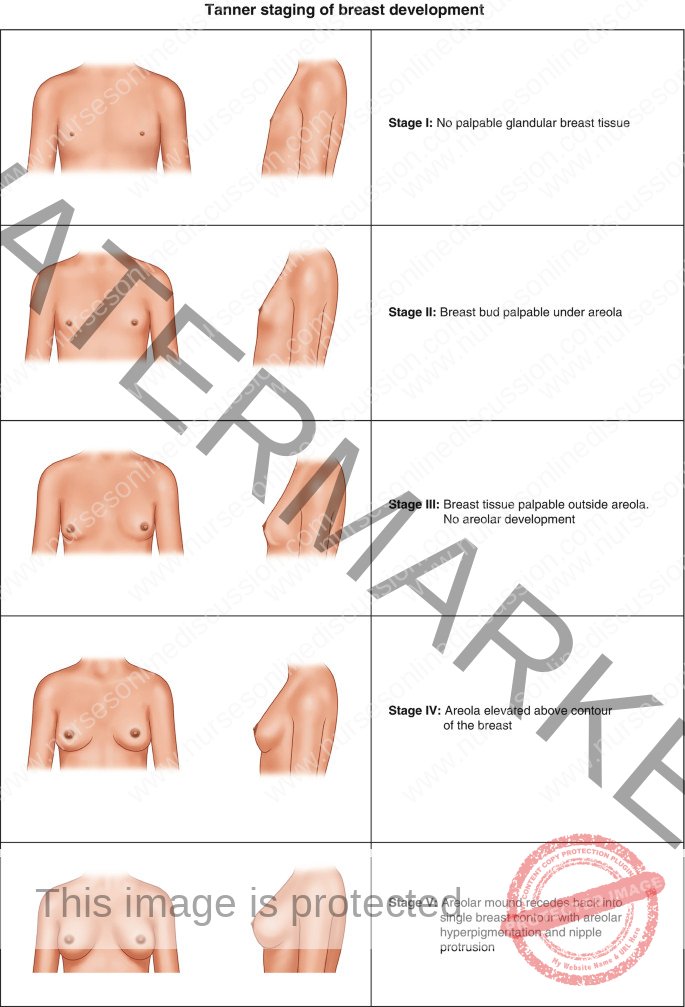
The Tanner scale for female breast development outlines five stages, from pre-pubertal to mature adult form:
Stage 1 (Preadolescent): There is no noticeable glandular breast tissue development. Only the papilla (nipple) is elevated above the chest wall.
Stage 2: The stage of “breast buds.” Small, palpable breast buds start to form under the areola (the pigmented area around the nipple). There is a slight elevation of the breast and nipple area as a small mound. The areola widens slightly.
Stage 3: Further enlargement of breast tissue occurs. The breast mound becomes more elevated and extends beyond the areola. The areola itself also enlarges but remains in the same contour as the breast mound.
Stage 4: Continued breast enlargement. A distinctive feature of this stage is the areola and papilla forming a secondary mound that projects above the overall contour of the developing breast.
Stage 5 (Adult): Represents the mature, adult breast. The breast is fully developed in size and shape. The areola returns to the general contour of the breast, no longer forming a separate mound. The nipple projects outward.

Pubic Hair Development in Females (Pubarche)
The Tanner scale also describes the stages of pubic hair development in females, concurrent with breast development but driven by different hormones:
Stage 1 (Preadolescent): There is no pubic hair present. The genital area is essentially hairless, similar to childhood.
Stage 2: The appearance of sparse, lightly pigmented, downy hair is observed. This initial hair growth is predominantly along the labia majora (outer lips of the vulva). The hair is typically long and fine.
Stage 3: Pubic hair becomes darker, coarser, and begins to curl. The hair spreads more densely over the mons pubis (the fleshy area above the pubic bone) and becomes easier to see.
Stage 4: The pubic hair now more closely resembles adult pubic hair in terms of texture and curl, but the distribution is still less extensive than in the adult stage. It covers a smaller area than in Stage 5 and does not yet extend onto the inner thighs.
Stage 5 (Adult): This stage represents the full adult pattern of pubic hair distribution. The hair is thick, coarse, and curly, forming an inverse triangle that extends to the inner thighs and sometimes up towards the linea alba (midline of the abdomen).
Tanner Stages in Males:

The Tanner staging system for males assesses pubertal progression in terms of both genital and pubic hair development, reflecting the influence of hormones.
Genital Development (Gonadarche) in Males
The stages of genital development in males, primarily focusing on the testes, scrotum, and penis, are as follows:
Stage 1 (Preadolescent): The testes, scrotum, and penis are at their childhood size. There is no noticeable enlargement or change from the prepubertal state.
Stage 2: The testes and scrotum begin to enlarge. There is an initial increase in the size of the testes and scrotum. The skin of the scrotum may start to redden and change in texture.
Stage 3: The penis begins to lengthen. There is continued growth of the testes and scrotum, which become further enlarged compared to Stage 2.
Stage 4: There is a notable increase in the size of the penis, particularly in width and circumference as well as length. The scrotum becomes darker in color and further enlarged. The glans penis (head of the penis) also becomes more pronounced.
Stage 5 (Adult): The genitalia reach their mature, adult size and shape. There is no further significant growth in the penis, testes, or scrotum. Adult size and proportions are achieved.

Classification of Precocious Puberty
Precocious puberty is broadly categorized into two main types, based on the underlying hormonal mechanisms:
Gonadotropin-Releasing Hormone (GnRH)-Dependent Precocious Puberty (Central Precocious Puberty):
Description: This is the more common form of precocious puberty overall, and it is significantly more frequent in girls than in boys (occurring 5 to 10 times more often in girls).
Mechanism: In GnRH-dependent precocious puberty, the hypothalamic-pituitary-gonadal (HPG) axis is activated prematurely. This axis is a critical regulatory system in the brain and endocrine system that controls sexual development. The early activation leads to:
Enlargement and maturation of the gonads (ovaries or testes).
Development of secondary sexual characteristics (e.g., breast development, pubic hair, genital enlargement).
Initiation of oogenesis (egg production) in girls or spermatogenesis (sperm production) in boys.
Cause: The primary cause is the early, but otherwise normal, activation of the hypothalamic-pituitary-gonadal axis. It is as if puberty is starting early, but the hormonal pathway is the same as in normal puberty.
Clinical Characteristics: This type of precocious puberty is characterized by a coordinated and complete pubertal development. In girls, this typically involves both breast development (thelarche) and pubic hair growth (pubarche), reflecting estrogen and androgen effects respectively. In boys, it is characterized by pubic hair development (pubarche) and testicular enlargement.
GnRH-Independent Precocious Puberty (Peripheral Precocious Puberty or Sex Hormone-Independent Precocious Puberty):
Description: This type is much less common than GnRH-dependent precocious puberty.
Mechanism: In GnRH-independent precocious puberty, secondary sexual characteristics develop due to high levels of circulating sex hormones (estrogens or androgens) from sources outside of the normal hypothalamic-pituitary activation. Crucially, the hypothalamic-pituitary axis is not activated in the usual pubertal manner.
Cause: The underlying cause is usually excessive secretion of sex hormones from:
The gonads (ovaries or testes) themselves, due to conditions like tumors or cysts.
The adrenal glands, which can also produce sex hormones, again often due to conditions like adrenal tumors or congenital adrenal hyperplasia.
Subtypes based on Sex Hormone Effects: GnRH-independent precocious puberty can be further classified based on the type of secondary sexual characteristics that develop, which in turn reflects the dominant sex hormone involved:
Isosexual Precocious Puberty: The secondary sexual characteristics that develop are consistent with the child’s genetic sex. This means:
Feminizing signs in girls: Such as breast development and menstruation. Driven by excess estrogens.
Masculinization in boys: Such as testicular enlargement, penile growth, and muscle development. Driven by excess androgens.
Heterosexual Precocious Puberty: The secondary sexual characteristics that develop are inconsistent with the child’s genetic sex. This is less common and indicates a more complex hormonal imbalance:
Masculine characteristics in girls: Girls may develop signs typically associated with males, such as deepening voice, increased muscle mass, and male-pattern hair growth. Often due to excess androgens.
Feminization in boys: Boys may develop signs typically associated with females, such as breast development (gynecomastia). Often due to excess estrogens.
Conditions Causing Precocious Puberty
Precocious puberty, categorized as either Central or Peripheral, arises from diverse underlying conditions affecting hormonal regulation.
Central Precocious Puberty (GnRH-Dependent): This type, also termed complete or true precocious puberty, stems from early activation of the hypothalamic–pituitary–gonadal (HPG) axis. Potential causes related to hypothalamic or pituitary dysfunction include:
Hypothalamic Haematoma: Blood clot formation in the hypothalamus can disrupt its normal inhibitory control over the HPG axis, leading to premature GnRH release and puberty onset.
Langerhans Cell Histiocytosis: This rare condition, characterized by Langerhans cell proliferation, can disrupt hypothalamic regulatory mechanisms, leading to early HPG axis activation and precocious puberty.
McCune–Albright Syndrome: Genetic mutations in McCune–Albright syndrome can cause abnormal hypothalamic function, disrupting the normal timing of puberty onset and causing prematurity.
Intracranial Neoplasm (Brain Tumors): Tumors within the brain can interfere with hypothalamic signaling pathways, leading to early GnRH release and subsequent central precocious puberty.
Infection: Central nervous system infections, particularly tuberculosis, can cause hypothalamic-pituitary axis inflammation. This inflammatory process can disrupt normal control and trigger premature puberty.
Trauma: Brain trauma, such as head injuries, can damage the hypothalamus and pituitary gland, causing malfunction of regulatory centers and contributing to early puberty activation.
Hydrocephalus: Cerebrospinal fluid accumulation in hydrocephalus can exert pressure on the hypothalamus. This pressure can damage hypothalamic tissue, disrupting HPG axis control and leading to central precocious puberty.
Angelman Syndrome: This genetic disorder can affect neurological functions, including hypothalamic regulation. Altered neural function can contribute to premature HPG axis activation and central precocious puberty.
Idiopathic or Constitutional: In many cases, no specific underlying cause is identifiable, and it is termed idiopathic or constitutional central precocious puberty.
Peripheral Precocious Puberty (GnRH-Independent): This type, also known as precocious pseudopuberty, is driven by sex steroids from abnormal sources, bypassing normal HPG axis activation. Causes vary by sex and the dominant hormone effect:
Isosexual (Feminizing) Conditions in Females:
McCune-Albright Syndrome: Genetic mutations can cause overactive endocrine glands, particularly ovaries, leading to excessive estrogen secretion and premature feminizing features.
Ovarian Tumors: Autonomous estrogen production by ovarian tumors can induce early development of female secondary sexual characteristics.
Heterosexual (Masculinizing) Conditions in Females:
Congenital Adrenal Hyperplasia (CAH): This genetic disorder causes adrenal glands to overproduce androgens, leading to masculinizing features in females due to androgen excess.
Adrenal Tumors: Androgen-producing adrenal tumors can cause masculinization in females due to excessive androgen influence.
Ovarian Tumors: In some cases, ovarian tumors can produce androgens, resulting in masculinization in females due to androgen excess.
Isosexual (Masculinizing) Conditions in Boys:
Congenital Adrenal Hyperplasia (CAH): Adrenal androgen overproduction in CAH leads to premature development of male secondary sexual characteristics due to excess androgens.
Leydig Cell Tumors: Testicular tumors of Leydig cells produce excess androgens, causing premature male secondary sexual characteristic development.
hCG-Secreting Tumors: Tumors that secrete human chorionic gonadotropin (hCG) stimulate androgen production, leading to the development of male secondary sexual characteristics.
Heterosexual (Feminizing) Conditions in Boys:
Feminizing Adrenocortical Tumor: Estrogen-producing tumors in the adrenal cortex can induce feminization in boys due to elevated estrogen levels.
Exogenous Hormones: External sources of hormones, often from medications, can alter hormonal balance and influence early development of secondary sexual characteristics.
Isosexual and Heterosexual Precocity – Rare Syndromes:
Aromatase Excess Syndrome: This rare genetic condition causes exceptionally high estrogen levels, leading to hyperfeminization in both males and females, representing an example of both isosexual and heterosexual precocity depending on the sex.
Risk Factors for Precocious Puberty:
Diet and Lifestyle: High-fat diets, lack of physical activity, and obesity in girls may be associated with earlier maturation.
Environmental Endocrine Disruptors: Exposure to xenoestrogens, such as Bisphenol A (BPA) in plastics, is a potential risk factor.
Pineal Tumors: Pineal gland tumors secreting chorionic gonadotropin (beta-hCG) can trigger precocious puberty.
Elevated Melatonin Levels: Although counterintuitive as melatonin is often associated with sleep, some research links elevated melatonin levels to precocious puberty.
Familial History: A family history of idiopathic central precocious puberty (ICPP) increases risk.
Genetic Mutations: Mutations in genes like LIN2, LEP, and LEPR, related to leptin and leptin receptor function, are implicated.
Diagnosis and Investigations in Precocious Puberty
Diagnosis relies on clinical assessment and investigations to identify precocious puberty and its underlying cause.
Clinical Manifestations:
Premature Secondary Sex Characteristics: Diagnosis is initially suspected based on the early appearance of secondary sexual characteristics, before typical age ranges.
Boys: Pubic hair or genital enlargement (gonadarche) before 9.5 years.
Girls: Pubic hair (pubarche) before 8 years, breast development (thelarche) before 7 years, or menstruation (menarche) before 10 years.
Blood Tests:
Hormone Assessment: Blood tests are used to measure hormone levels. In some conditions causing peripheral precocious puberty, blood tests may reveal elevated androgen levels with low cortisol levels, particularly in certain types of congenital adrenal hyperplasia (CAH).
Evaluation – Medical History: A thorough medical history includes:
Age at Onset: When the first signs of puberty were noticed.
Sex: Patient’s biological sex.
Pubertal Progression: How rapidly puberty is progressing.
Hypothyroidism Symptoms: Assessing for symptoms that might suggest hypothyroidism as a related or differential diagnosis.
CNS History: History of past CNS infections, headaches, visual disturbances, and seizures, which might indicate central nervous system involvement.
Physical Examination: A detailed physical examination involves:
Growth Measurements: Height, weight, and height velocity are measured to assess growth patterns.
Pubertal Staging: Pubertal stage is assessed using Tanner staging to document physical development.
Androgen and Estrogen Effects: Evaluate for clinical signs of androgen and estrogen effects, such as acne, body odor, breast development, or genital changes.
Skin Inspection: Inspection of the skin for café au lait macules, which are associated with McCune-Albright Syndrome.
Hypothyroidism Signs: Examination for signs of hypothyroidism, as it can sometimes be related to pubertal abnormalities.
Basic Radiology:
Bone Age Assessment: X-ray of the left wrist and hand to determine bone age, which indicates skeletal maturity and helps assess the advancement of puberty.
Pelvic and Abdominal Sonography (Ultrasound): Ultrasound imaging of the pelvis and abdomen to identify any ovarian cysts, adrenal masses, or structural abnormalities in reproductive organs that may be contributing to precocious puberty.
Hormone Evaluation – Stimulation Tests:
GnRH Stimulation Test (or Leuprolide Stimulation Test): Intravenous administration of gonadotropin-releasing hormone (GnRH) or a GnRH agonist like leuprolide is used to assess pituitary response. This test is particularly helpful in diagnosing central precocious puberty, especially in boys.
Girls – Estradiol Levels Post-Stimulation: In girls, central precocious puberty can be confirmed by measuring pubertal levels of estradiol (>50 pg/mL) in blood samples collected 20-24 hours after stimulation with leuprolide. This elevated estradiol level post-stimulation indicates central, GnRH-dependent puberty.

Challenges Faced by Children with Precocious Puberty
Children experiencing precocious puberty encounter a unique set of challenges due to the early onset of sexual development, impacting both physical and psychosocial well-being.
In Girls:
Compromised Adult Height: Accelerated bone maturation due to early puberty can lead to premature closure of growth plates, potentially resulting in a shorter adult height than genetically predicted.
Underlying Serious Conditions: Precocious puberty can be an indicator of underlying medical issues, such as tumors or other endocrine disorders, requiring further investigation and management.
Increased Risk of Sexual Exploitation: The early development of adult-like physical characteristics can unfortunately increase the risk of becoming targets for adult sexual exploitation, a serious safety concern.
Heightened Vulnerability to Sexual Abuse: Physically appearing more mature may make these young girls more vulnerable to sexual abuse due to misperceptions of their age and maturity.
Social Stigma and Peer Issues: Developing physically ahead of their peers can lead to teasing and bullying from classmates who may not understand the condition, causing social isolation and emotional distress.
Mental Health Concerns: Precocious puberty is associated with an increased risk of developing mental health disorders, such as anxiety and depression, possibly due to the emotional and social challenges they face.
Adult Short Stature: Due to advanced bone age, the growth spurt ends prematurely, often leading to a final adult height that is shorter than what would have been achieved without early puberty.
In Boys:
Increased Aggression: Hormonal surges characteristic of puberty, occurring early, can contribute to increased aggressiveness and irritability in boys, potentially impacting behavior and relationships.
Social Expectations and Pressure: Early physical maturation may lead to unrealistic social expectations, with others expecting these young boys to behave and act like older adolescents or even adults, placing undue pressure on them.
Developmental Disparity: While physically maturing faster, their cognitive, emotional, and social development may still lag behind their advanced physical appearance. This mismatch can create internal and external conflicts.
Increased Risky Behaviors: Studies indicate that early maturing boys are more likely to engage in sexual activity at a younger age and are also at a higher risk for participating in other risky behaviors, potentially due to hormonal influences and social dynamics.
Treatment of Precocious Puberty
Treatment strategies for precocious puberty aim to halt or reverse early sexual development, address underlying causes, and mitigate the physical and psychosocial challenges associated with the condition.
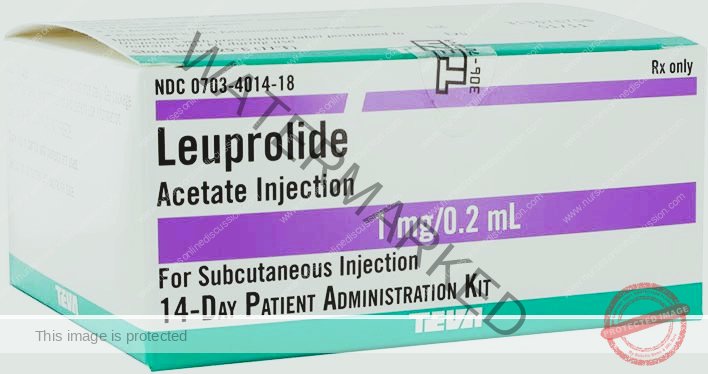
Pharmacological Treatment:
Anastrozole: Anastrozole, an aromatase inhibitor, is mentioned as a potential treatment. Aromatase inhibitors reduce estrogen production, which can be relevant in certain types of precocious puberty, particularly in girls.
GnRH Agonists: Gonadotropin-Releasing Hormone (GnRH) agonists are a primary treatment modality for central precocious puberty. Examples include:
Histrelin Acetate (Supprelin LA): A long-acting GnRH agonist implant.
Triptorelin: Another GnRH agonist available in injectable forms.
Leuprolide: A commonly used GnRH agonist, often administered via injection. A typical dosage mentioned is Inj. Leuprolide (0.5-0.3 mg/kg/dose) monthly.
Mechanism of GnRH Agonists:
Paradoxical Effect: Interestingly, non-continuous use of GnRH agonists can stimulate the pituitary gland, leading to increased release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
Continuous Use – Downregulation: However, regular, continuous use of GnRH agonists leads to the opposite effect. It downregulates the pituitary gland’s GnRH receptors, effectively decreasing the release of both FSH and LH. This suppression of gonadotropins is the therapeutic mechanism in central precocious puberty.
Long-Term Use Consideration: Prolonged use of GnRH agonists carries a potential risk of osteoporosis due to hormonal suppression.
Reversibility: Upon discontinuation of GnRH agonist treatment, pubertal changes are expected to resume within 3 to 12 months. Therefore, regular monitoring is crucial throughout the treatment period and after cessation.
Surgical Treatment:
Surgery may be indicated when precocious puberty is caused by certain types of tumors:
Tumor Removal: Surgical removal is the primary treatment for tumors of the ovary, testis, and adrenal glands that are causing peripheral precocious puberty by excessive hormone production.
Hypothalamic Hamartomas: While hypothalamic hamartomas (benign tumors in the hypothalamus) can cause central precocious puberty, surgical removal is generally not recommended. These hamartomas are considered low-risk for growth or malignancy, and surgery in this area is hazardous due to the hypothalamus’s critical functions.
Radiotherapy: Radiotherapy may be used to treat:
Germ Cell Tumors: Certain germ cell tumors can cause precocious puberty.
Pineal Tumors: Tumors in the pineal gland.
hCG-Producing Suprasellar Tumors: Suprasellar tumors that secrete human chorionic gonadotropin (hCG), which can stimulate hormone production leading to precocious puberty.
Nurses’ Roles in the Management of Precocious Puberty
Nurses play a crucial and multifaceted role in the care of children with precocious puberty and their families, encompassing assessment, education, emotional support, and coordination of care. Key nursing responsibilities include:
Assessment and Monitoring:
Conduct comprehensive assessments to collect relevant patient data, including medical history, developmental history, and family history.
Monitor the progression of secondary sexual characteristics using Tanner staging and document findings.
Monitor and document hormonal levels from lab results and track trends over time.
Regularly assess the emotional and psychological well-being of the child, noting any signs of distress, anxiety, or social difficulties.
Patient and Family Education:
Provide thorough education to the patient and family about precocious puberty, ensuring they understand the condition, its potential causes, and diagnostic processes.
Explain the purpose and significance of diagnostic tests and procedures, addressing any questions and concerns.
Offer clear and comprehensive guidance on the expected course of treatment, including medication regimens, potential side effects, and expected outcomes.
Educate on the importance of medication adherence and proper administration techniques for medications like GnRH agonists.
Emotional Support:
Provide consistent emotional support to both the child and their family throughout the entire diagnostic and treatment journey.
Actively listen to and address the concerns, anxieties, and fears expressed by the patient and family members.
Facilitate open and honest communication between all members of the healthcare team, the patient, and their family to ensure everyone is informed and involved.
Collaboration with Healthcare Team:
Actively collaborate with endocrinologists, radiologists, surgeons, psychologists, and other specialists involved in the patient’s care.
Participate in the development and implementation of the patient’s individualized care plan, contributing nursing expertise and patient-centered insights.
Effectively communicate nursing observations and assessments to the interdisciplinary team to ensure coordinated care.
Administration of Medications:
Administer medications as prescribed by the physician, particularly GnRH agonists, which are cornerstone treatments for central precocious puberty.
Educate patients and families on proper medication administration techniques, including subcutaneous or intramuscular injection techniques if applicable, and strategies for consistent adherence.
Provide detailed information on potential medication side effects and what to expect during treatment.
Monitoring for Adverse Effects:
Vigilantly monitor patients for any adverse effects of medications or surgical interventions, paying close attention to potential side effects of GnRH agonists.
Promptly report and accurately document any unexpected or adverse reactions observed, ensuring timely intervention.
Psychosocial Support:
Actively address the psychosocial challenges often associated with precocious puberty, such as body image concerns, self-esteem issues, and difficulties with social interactions and peer relationships.
Facilitate access to support groups or counseling services for both the patient and their family to provide a supportive environment and strategies for coping.
Advocacy:
Act as a patient advocate within the healthcare system, ensuring that the child’s unique needs and best interests are always prioritized.
Ensure that the patient’s rights and preferences are fully respected throughout the diagnostic and treatment processes.
Coordination of Care:
Coordinate the various aspects of the patient’s comprehensive care plan, streamlining appointments, procedures, and consultations.
Ensure smooth and effective transitions between different phases of care, such as from diagnosis to treatment, and between inpatient and outpatient settings when necessary.
Continuity of Care:
Promote continuity of care by scheduling and ensuring attendance at regular follow-up appointments with the endocrinologist and other specialists.
Establish and maintain effective communication channels between outpatient and inpatient care teams to facilitate seamless care transitions.
Patient Safety:
Prioritize patient safety during all diagnostic procedures and treatment interventions, adhering to safety protocols and guidelines.
Educate patients and families on safety measures that should be implemented at home, particularly related to medication storage, potential side effects, and recognizing warning signs.
Documentation:
Maintain accurate, thorough, and comprehensive documentation of all patient assessments, nursing interventions, medication administration, patient education, and treatment outcomes in the patient’s medical record.
Ensure that all relevant information is readily available and accessible to the entire healthcare team to facilitate informed decision-making and effective communication.
Patient Advocacy (Holistic Well-being):
Act as a strong advocate for the patient’s holistic well-being, considering and addressing their physical, emotional, and psychosocial needs.
Be prepared to address any ethical concerns that may arise during the management process, ensuring care is provided in an ethically sound and patient-centered manner.
Education on Follow-Up Care:
Provide detailed instructions for follow-up care at the time of discharge or outpatient visits, including clear medication schedules, appointment reminders, and information on potential lifestyle adjustments needed to manage precocious puberty and its effects.
Promoting Coping Strategies:
Facilitate the development of healthy coping strategies for both the child and their family to manage the emotional, social, and physical challenges associated with precocious puberty.
Encourage open communication within the family unit and provide a safe space for the patient and family members to express their feelings and concerns about the condition and its management.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

