Eye Conditions
Subtopic:
Visual Impairment
Vision impairment, also known as vision loss, denotes a reduction in the ability to see, to a level that presents challenges unresolvable through conventional methods like spectacles.
The term ‘visual impairment’ encompasses a spectrum of sight deficiencies, from limited vision to complete blindness.
In clinical terms, visual impairment is frequently identified when the best corrected visual acuity is poorer than 20/40 or 20/60 in the better eye.
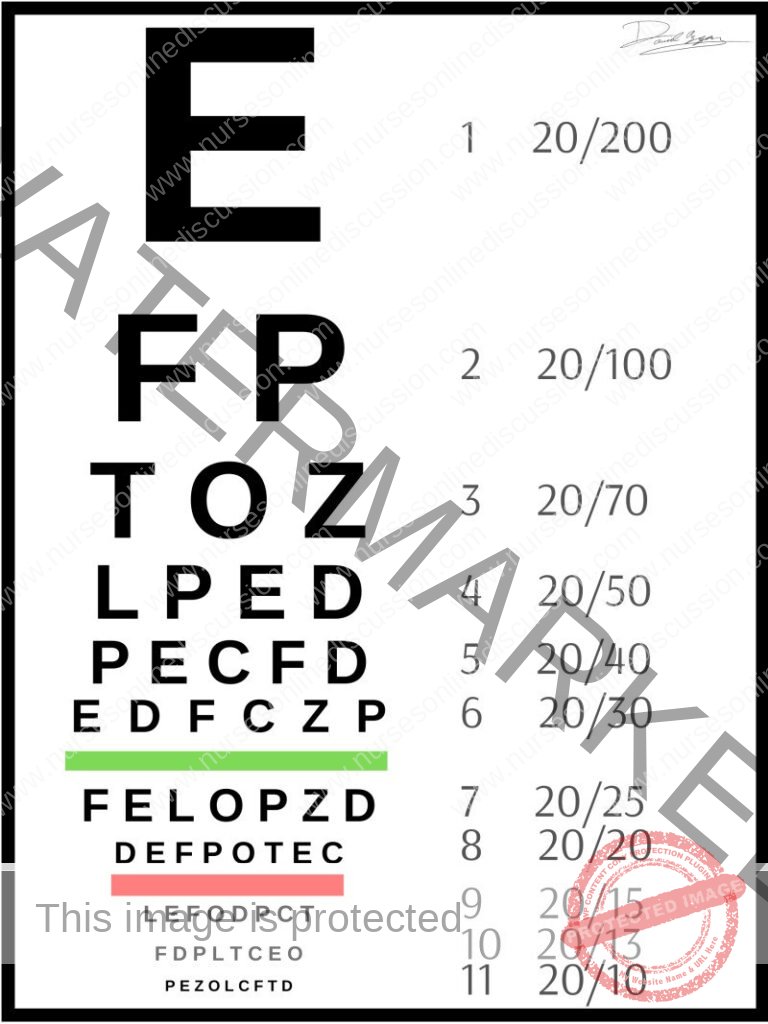
Understanding Visual Acuity Numbers
Visual acuity values are metrics employed to assess the sharpness or clarity of an individual’s eyesight. These values are presented in a fractional format, like 20/20 or 20/40.
The components of these fractions are interpreted thus:
Numerator (Top Value): The numerator, or the upper number in the visual acuity fraction, signifies the distance in feet between the individual being tested and the eye chart. For instance, a numerator of 20 indicates the person is positioned 20 feet from the chart.
Denominator (Bottom Value): The denominator, or the lower number, denotes the distance, also in feet, from which a person with typical vision could discern the same line on the eye chart as the person being examined. For example, a denominator of 20 implies that someone with standard vision could read that specific line from 20 feet away.
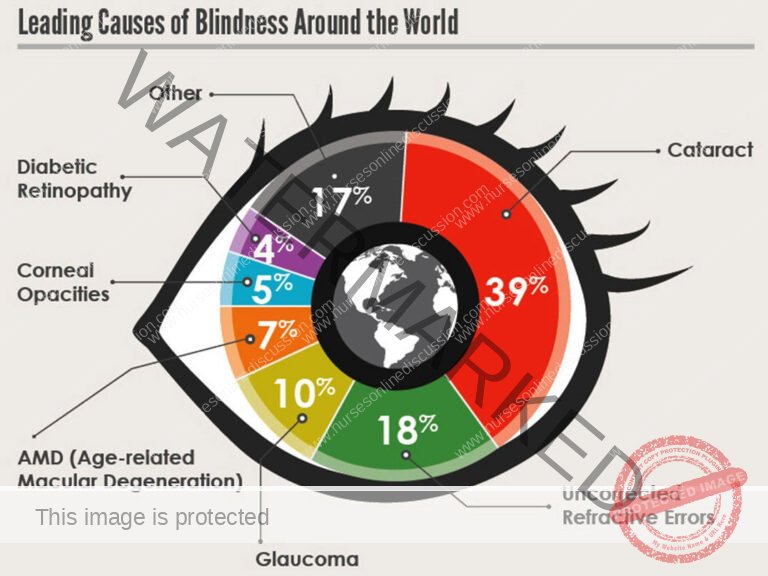
Causes of Visual Impairment
Globally, the primary origins of vision impairment are unaddressed refractive errors (43%), cataracts (33%), and glaucoma (2%). Vision loss can stem from a range of factors, encompassing inherited conditions, ocular trauma, infections, and age-related ailments.
Inherited Predispositions:
Retinitis Pigmentosa: A genetic disorder characterized by the progressive degeneration of retinal cells, resulting in a gradual decline in vision.
Congenital Cataracts: Lens opacities present at birth. If untreated, these can impede visual development and lead to impairment.
Glaucoma: A collection of eye conditions often with a genetic component, that damage the optic nerve.
Ocular Trauma:
Physical Injury: Damage to the eye resulting from accidents, athletic activities, or workplace incidents can induce vision loss or impairment.
Corneal Damage: Injury to the cornea, the transparent frontal layer of the eye, can precipitate visual disturbances.
Corneal Opacity: Clouding or scarring of the cornea, which can be initiated by corneal abrasions or, in some instances, corneal swelling.
Infectious Agents:
Ocular Infections: Untreated eye infections like conjunctivitis, uveitis, or keratitis have the potential to cause visual impairment.
Prenatal Infections: Certain maternal infections, such as rubella (German measles), can be transmitted to a developing fetus, potentially causing vision impairment in the infant.
Trachoma: An eye disease induced by the bacterium Chlamydia trachomatis. This condition remains a public health concern in 42 countries, contributing to blindness or visual impairment in approximately 1.9 million individuals.
Age-Related Conditions:
Cataracts: Lens clouding, frequently linked to the aging process, leading to blurred vision and visual decline.
Age-Related Macular Degeneration (AMD): A progressive condition affecting the macula – the central area of the retina – causing loss of central vision.
Glaucoma: Elevated intraocular pressure can harm the optic nerve, potentially resulting in vision loss.
Childhood-Onset Blindness:
Visual impairment in children can arise from diverse causes, including genetic disorders, infections, and developmental anomalies.
Other Contributing Factors:
Diabetic Retinopathy: Damage to retinal blood vessels due to diabetes, which can progress to visual impairment or blindness.
Amblyopia (Lazy Eye): Diminished vision in one eye resulting from atypical visual development during childhood.
Medication Side Effects: Certain pharmaceuticals, including some used in chemotherapy or for autoimmune conditions, may have vision-related side effects.
Uncorrected Refractive Errors: Uncorrected conditions like nearsightedness, farsightedness, and astigmatism can lead to visual impairment.
Undetermined Etiology: In a notable proportion of cases, the specific cause of visual impairment remains unidentified.
Signs and Symptoms of Visual Impairment
Diminished Visual Clarity (Blurred Vision): Objects appear indistinct or lack sharp focus.
Diplopia (Double Vision): Perception of two images of a single object.
Visual Phantoms (Floaters): Observation of specks, spots, or web-like formations drifting across the visual field.
Photopsia (Flashes of Light): Sudden bursts of light perception, particularly in peripheral vision.
Halos around Lights: Perceiving luminous rings encircling light sources, especially bright ones.
Iris Pigmentation Changes: Noticeable alterations in iris coloration, such as darkening or lightening.
Ocular Pain: Abrupt or recurring discomfort in or around the eye.
Photosensitivity (Sensitivity to Light): Discomfort or pain upon exposure to bright illumination.
Nyctalopia (Difficulty Seeing at Night): Struggling to achieve clear vision in dimly lit environments.
Peripheral Vision Loss: Reduced capacity to perceive objects or motion at the outer edges of the visual field.
Shape Agnosia (Inability to See Shapes): Difficulty in discerning and recognizing the outlines and forms of objects.
Clouded Vision: A hazy or obscured visual experience that impedes clear sight.
Shadow Vision: Perception limited to light and dark contrasts, lacking detailed visual information.
Tunnel Vision: A constricted visual field due to significant reduction in peripheral vision.
Visual impairments can also affect daily activities, including:
Reading Difficulties: Necessity to hold reading materials very close, impaired reading in low light, or reduced reading speed.
Mobility Challenges: Collisions with objects, difficulty navigating stairs or uneven terrain, or impaired depth perception.
Facial and Object Recognition Issues: Struggling to identify faces or objects, especially at a distance.
Color Discrimination Problems: Difficulty in distinguishing between colors or coordinating color combinations in attire.
Asthenopia (Eye Strain): Experiencing eye fatigue, headaches, or discomfort following prolonged visual tasks.

Diagnosis, Tests, and Investigations for Ruling Out Visual Impairment
These evaluations are crucial for assessing visual function and identifying any anomalies or impairments.
History and External Ocular Examination:
A comprehensive medical history is taken, including inquiries about family history related to visual impairment.
A visual inspection of the external eye structures is conducted, encompassing the eyelids, conjunctiva, cornea, iris, lens, and other visible components.
Visual Acuity Evaluation:
The Snellen chart assessment, also known as the visual acuity test, is frequently employed.
The individual is asked to read a sequence of letters and numbers of progressively smaller sizes from a standardized chart positioned at a distance of 6 meters (approximately 20 feet).
The smallest line of characters the person can accurately read determines their visual sharpness.
The result is presented as a ratio, providing an indication of the individual’s visual capability relative to standard vision.
Visual Field Assessment:
Perimetry and visual field testing techniques are used to evaluate the extent and integrity of the field of vision.
This test specifically examines vision beyond the central macula, measuring the scope of peripheral sight.
The assessment involves presenting brief flashes of light in the patient’s side vision, with the patient indicating when they perceive these flashes.
Any absent areas or irregularities within the visual field can be identified through this procedure.
Tonometry Examination:
Tonometry is performed to measure the intraocular pressure within the eye, a key step in screening for glaucoma.
Ocular Motility Evaluation:
This evaluation assesses the movements of the eyeballs, checking for conditions like strabismus (squint) or other oculomotor dysfunctions.
Supplementary Examinations:
In specific situations, further tests may be indicated, such as Visually Evoked Potentials (VEP), Electroretinography (ERG), and Electrooculography (EOG).
These advanced tests analyze the transmission of electrical signals from the eye to the brain and can be particularly valuable in diagnosing visual impairment, especially in younger individuals or those with complex conditions.

Classification of Visual Impairment
The International Classification of Diseases 11th Revision (ICD-11, 2018) delineates a system for classifying vision impairment, dividing it into two primary categories: distance vision impairment and near vision impairment. Assessment is conducted through the use of standardized eye charts viewed at a specified distance.
Distance Vision Impairment:
Mild: Visual acuity is less than 6/12. This signifies that an individual with mild distance vision impairment perceives at a distance of 6 meters what a person with typical vision can perceive at 12 meters.
Moderate: Visual acuity is less than 6/18. Individuals classified as having moderate distance vision impairment are able to see at 6 meters what someone with normal vision can see at 18 meters.
Severe: Visual acuity is less than 6/60. Those with severe distance vision impairment have the capacity to see at 6 meters what a person with unimpaired vision can see at 60 meters.
Blindness: Visual acuity is less than 3/60. This category encompasses individuals with extremely limited or no visual perception.
Near Vision Impairment:
Near visual acuity is less than N6 or M.08 when assessed at a standard reading distance with optimal correction (e.g., glasses). This indicates difficulty in clearly viewing close-range objects, even with vision aids.
N6 Explained: “N6” is a designation for near visual acuity measurement. It specifies the level of visual clarity for close-up tasks. The “N” prefix denotes “near,” and the numerical value corresponds to a visual acuity scale. N6 specifically refers to the ability to see clearly at a distance of 40 centimeters (approximately 16 inches) with any necessary corrective lenses in place. The ICD-11 (2018) utilizes N6 as a benchmark for classifying near vision impairment.
40 cm Context: A distance of 40 centimeters (or 16 inches) is the standard working distance employed for near visual acuity testing. It represents the distance at which an individual’s ability to see close objects is evaluated. This measurement is commonly used in eye examinations and is recognized as the standard distance for assessing near vision capability.
M.08 Interpretation: “M.08” in this context signifies near visual acuity that is worse than both N6 and M.08 at 40 cm. This indicates that individuals with M.08 near vision impairment experience difficulty seeing objects sharply at close distances, even when using vision correction like spectacles or contact lenses.
Note: The combination of blindness and hearing loss is termed deafblindness.
Management of Visual Impairment
Management strategies encompass surgical interventions, pharmaceutical approaches, rehabilitation programs, and preventative measures.
Patient Reception:
Approach the patient and their caregiver with compassion and understanding.
Gather pertinent medical history, specifically focusing on the visual impairment and any currently used assistive devices.
Ensure a comfortable waiting environment with adequate illumination and clear signage designed to aid individuals with visual impairments.
Medical Assessment and Diagnosis:
A comprehensive ophthalmological examination should be conducted to pinpoint the underlying cause and severity of the vision impairment.
Execute necessary diagnostic tests, including visual acuity assessments, visual field examinations, and imaging studies as required.
Communicate the diagnosis clearly to both the patient and their caregiver, explaining the implications and the spectrum of available treatment options.
Treatment and Management:
Following result analysis, prescribe appropriate vision correction aids, such as eyeglasses or contact lenses, when indicated.
Recommend assistive devices and technologies tailored to the patient’s specific needs, for example, magnification tools, visual aids, and adaptive technology solutions.
Refer the patient to specialized low vision rehabilitation programs for focused training and support.
Provide information regarding accessible support services, including counseling, peer support groups, and the process for registering as visually impaired if appropriate.
Rehabilitation and Training:
Organize orientation and mobility training to empower the patient to navigate their surroundings safely and independently.
Offer training in daily living skills to promote self-sufficiency in everyday activities.
Provide access to Braille instruction for individuals interested in learning this tactile literacy system. Braille is a system of touch-based reading and writing utilized by individuals who are blind or visually impaired, consisting of raised dots arranged in cells, discernable by touch.
Facilitate participation in low vision rehabilitation programs to optimize the patient’s residual vision through focused training and adaptive techniques.
Emotional and Psychological Support:
Offer access to counseling services to address the emotional and psychological challenges that can accompany visual impairment.
Connect the patient and their caregiver with relevant support groups to foster shared experiences and peer-to-peer encouragement.
Collaborate with mental health professionals to manage any psychological issues that may be related to the visual impairment.
Ongoing Monitoring and Follow-up:
Schedule regular follow-up appointments to diligently monitor the patient’s visual health and adjust the management strategy as necessary.
Provide educational resources and information to the patient and their caregiver to support ongoing self-management and care.
Discharge:
Confirm that both the patient and their caregiver fully understand the management plan and have access to all essential resources and support services.
Supply written instructions, including details on medications, scheduled follow-up appointments, and contact information for further assistance.
Coordinate with other healthcare providers involved in the patient’s care to ensure a seamless transition after discharge.
Surgical Management:
Surgical intervention is a critical aspect of management, dependent on the underlying cause of the visual impairment.
Cataract Surgery:
A frequent surgical procedure to treat visual impairment resulting from cataracts.
Involves the removal of the clouded natural lens of the eye and its replacement with an artificial intraocular lens (IOL).
Generally demonstrates a high success rate in restoring vision and enhancing visual acuity.
Corneal Transplant:
Considered when visual impairment is caused by a scarred or damaged cornea.
Replaces the impaired cornea with a healthy donor cornea.
Can be effective in improving vision and restoring corneal clarity.
Retinal Surgery:
May be indicated for visual impairment arising from retinal conditions, such as retinal detachment or macular holes.
Specific surgical techniques are tailored to the condition and may involve repair or reattachment of the retina.
Laser surgery can also be employed to treat certain retinal conditions, like diabetic retinopathy or retinal tears.
Glaucoma Surgery:
May be necessary in cases of visual impairment due to glaucoma to manage the condition.
Various surgical options exist, including trabeculectomy, tube shunt implantation, and laser trabeculoplasty.
These procedures aim to lower intraocular pressure and prevent further optic nerve damage, thereby preserving vision.
Prevention
Adopt a Nutritious Diet: Maintain a balanced diet abundant in fruits, vegetables, and omega-3 fatty acids to promote optimal eye health.
Routine Eye Examinations: Schedule regular eye check-ups for early detection and timely intervention for vision problems. The recommended frequency of examinations can vary based on age and individual risk factors.
Be Aware of Family Eye History: Understanding your family history of eye conditions can help identify potential predispositions and facilitate proactive preventative actions.
Maintain a Healthy Lifestyle: Embrace a healthy lifestyle that includes regular physical activity and abstaining from smoking to support overall eye health.
Protect Eyes from Trauma: Utilize robust eye protection when participating in activities that pose a risk to eyesight, such as sports or working with hazardous materials, to prevent injuries.
Avoid Harmful Substances: Refrain from smoking, as it significantly increases the risk of vision problems like macular degeneration and cataracts. Furthermore, minimize exposure to harsh chemicals and protect the eyes from damaging substances.
Shield Eyes from UV Radiation: Wear sunglasses that offer 99-100% protection against UVA and UVB rays to safeguard your eyes from the harmful effects of ultraviolet radiation.
Practice Good Eye Hygiene: Take frequent breaks during digital device use or when performing visually intensive tasks to prevent eye strain. Blink regularly to maintain eye lubrication and use artificial tears if needed.
Manage Chronic Conditions Effectively: Properly manage chronic conditions such as diabetes and hypertension, as they can contribute to the development of vision problems.
Genetic Testing Considerations: Genetic testing can be a valuable tool in the prevention of inherited eye disorders like Retinitis pigmentosa.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

