Gynaecology (II)
Subtopic:
Congenital anomalies of the female genital organs
These conditions represent developmental irregularities affecting the female reproductive organs that arise during intrauterine life.
Congenital anomalies of the female reproductive tract are essentially developmental abnormalities occurring in the organs responsible for reproduction, which originate during the embryonic stage.
These anomalies, affecting the female reproductive system from the uterus to the external genitalia, can stem from genetic predispositions, environmental influences, or, in many instances, undetermined factors. They can impact various components of the reproductive system, including the uterus, vagina, cervix, ovaries, and external genitalia.
These anomalies often arise from disruptions in the embryological development of the Müllerian ducts. The Müllerian ducts are critical as they are the precursors to the female reproductive organs.
In the developing female embryo, two Müllerian ducts are present. Under normal development, these ducts are programmed to transform into the fallopian tubes, uterus, cervix, and the upper portion of the vagina. Typically, these ducts undergo a process of fusion to form a single uterine cavity, followed by canalization, which is the formation of hollow channels within the tissues, ultimately shaping the final structures of the fallopian tubes, uterus, and upper vagina.
These conditions are also known as:
Uterine/vaginal anomalies
Mullerian anomalies
Mullerian duct anomalies
Aplasia (agenesis)
Aetiology/Causes
The precise origins of these embryonic developmental disruptions are often not fully understood.
Genetic Factors: These can include inherited genetic mutations or chromosomal abnormalities. Specific examples include Turner syndrome, which primarily impacts ovarian development, and Androgen Insensitivity Syndrome, which significantly affects the development of external genitalia.
Environmental Factors: Exposure to harmful substances during pregnancy can play a role. Notable examples of such exposures include medications like diethylstilbestrol (DES) (previously prescribed to prevent miscarriage), certain infections during pregnancy (such as rubella), and various environmental toxins.
Unknown Factors: In a significant number of cases, the specific cause of congenital anomalies remains unidentified.

Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome
Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome is a disorder that occurs in females and mainly affects the reproductive system.
This condition causes the vagina and uterus to be underdeveloped or absent, although external genitalia are normal. It is also known as Rokitansky-Küster-Hauser syndrome
Anomalies of the Vulva
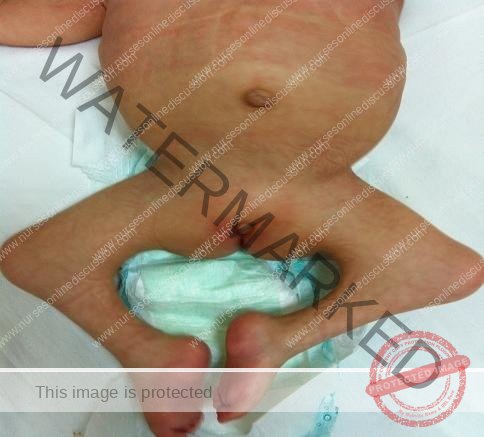
Labial Hypoplasia:Underdevelopment of the labia majora or minora, or both, resulting in smaller or absent labial structures. Labial hypoplasia is a harmless condition in which one or
both sides of the labia don’t form normally during puberty. One side may be normal while the other side grows smaller or is absent.
Can cause aesthetic concerns or discomfort, especially during activities like cycling or wearing tight clothing.
Management:
Often no treatment is required unless associated with functional or aesthetic concerns, which can be addressed surgically.
Labial Hypertrophy: Overdevelopment or enlargement of the labia majora or minora. May cause discomfort, difficulty with hygiene, or self-consciousness.
Clinical Features:
Enlarged labia, potentially causing discomfort, irritation, hygiene problems, difficulty with urination, or cosmetic concerns. May be asymmetric.
Management:
Labiaplasty: Surgical reduction to achieve a more typical size.
Conservative Management: Symptom management like use of padded undergarments.

Clitoral Hypertrophy: An unusually large clitoris. Size is relative and depends on age and other factors.
Clinical Features:
Enlarged clitoris, possibly impacting urination, sexual function, or causing cosmetic concerns. Often associated with conditions like congenital adrenal hyperplasia (CAH).
Management:
Observation, clitoroplasty (surgical reduction), hormonal therapy (if CAH is present), and psychological support are options depending on severity and associated conditions.

Fusion Anomalies: Abnormal fusion of the labia. This can range from mild to complete fusion.
Labial adhesion: Fusion of the labia majora, sometimes extending to the labia minora.
Clinical Features: Fused labia, creating an obstruction to the vaginal opening (introitus), potentially impacting urination, menstruation, and hygiene.
Management: Labiaplasty (surgical separation) is needed to create a normal vaginal opening.
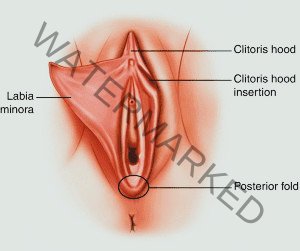
Anomalies of the Hymen
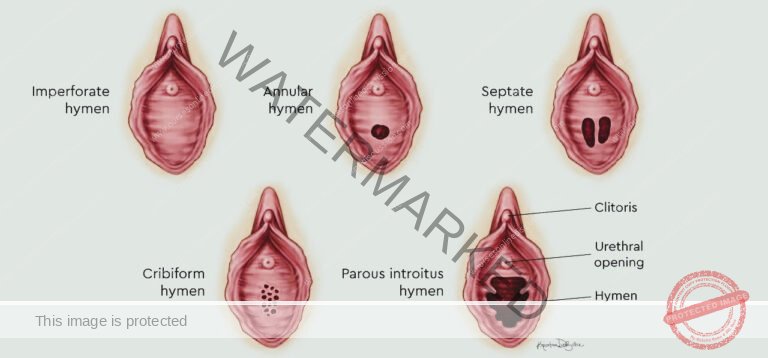
Imperforate Hymen: Characterized by a complete membrane obstructing the vaginal opening. The hymen entirely covers the vaginal orifice, preventing any opening.
Symptoms (S/S): Often undetected until puberty, it typically presents at menarche (first menstruation) with:
Cryptomenorrhea (Hidden Menstruation): Menstrual blood is produced but cannot exit the body, leading to internal accumulation.
Primary Amenorrhea: Absence of visible menstruation despite other signs of puberty.
Severe Abdominal or Pelvic Pain: Intense pain arises from hematocolpos, the build-up of menstrual blood within the vagina.
Urinary Issues: Urinary retention (inability to urinate) or urinary frequency (increased urge to urinate) can occur due to pressure on the bladder.
Constipation: Difficulty passing stools may result from pressure on the rectum.
Bulging Hymen: A noticeable outward bulging of the hymen may be observed upon physical examination.
Back Pain: Pain in the back can sometimes be associated with the pressure from retained blood.
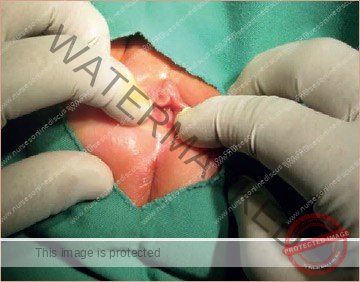
Management: Requires a surgical hymenectomy. This procedure involves creating a surgical opening in the hymen to allow for normal vaginal drainage and function.
Microperforate Hymen: Defined by a very small opening within the hymen. While an opening exists, it is significantly reduced, leading to restricted menstrual flow.
Symptoms: Symptoms may mirror those of an imperforate hymen, but are generally less severe. Common presentations include:
Spotting: Very light bleeding may occur.
Pain: Discomfort can be present, though typically less intense than with an imperforate hymen.
Delayed Complete Menstrual Evacuation: Menstrual flow may be prolonged or incomplete due to the restricted opening.
Management: Usually addressed with a minor surgical procedure to enlarge the existing hymenal opening, improving menstrual outflow.
Hymenal Variations: The appearance of the hymen exhibits significant natural diversity among individuals. These variations are generally considered within the normal spectrum unless they cause specific symptoms or functional issues. Common variations include:
Annular Hymen: The most frequent type. It presents as a circular or ring-shaped hymen surrounding a central opening. This is considered the typical hymenal configuration.
Septate Hymen: Characterized by one or more bands of tissue that traverse the hymenal opening. These bands effectively divide the opening into multiple smaller orifices. A septate hymen can sometimes lead to:
Painful Intercourse: Discomfort during sexual penetration.
Difficult Tampon Insertion: Challenges or pain when inserting tampons.
Obstruction of Menstrual Flow: In some cases, the tissue bands can impede the normal outflow of menstrual blood.
Cribriform Hymen: This variation is distinguished by numerous small perforations throughout the hymen. This sieve-like appearance typically does not cause any medical problems or require intervention.
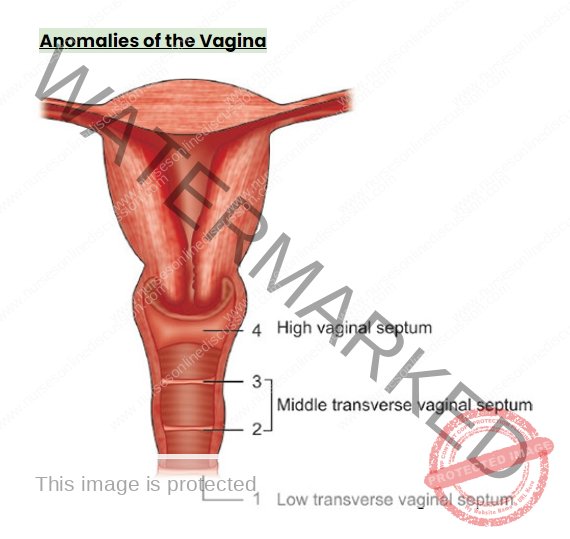
Transverse Vaginal Septum: This is a horizontal band of tissue that can partially or completely block the vaginal canal. It’s like a wall across the vagina.
Symptoms:
Primary Amenorrhea: Absence of menstruation.
Cyclic Abdominal Pain: Recurring pain with menstrual cycles.
Dyspareunia: Painful sexual intercourse.
Management: Requires surgical excision of the septum to restore a normal, open vaginal passage.
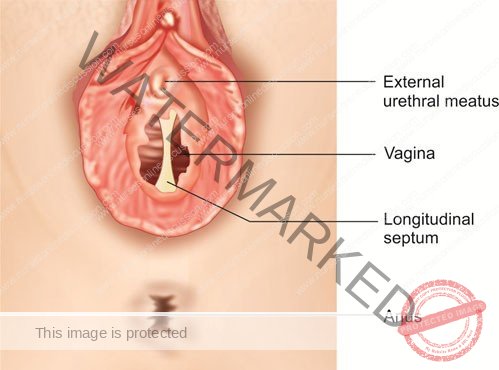
Vertical or Complete Vaginal Septum: This is a vertical wall that divides the vagina into two separate channels. It runs lengthwise down the vagina.
Potential Effects:
Dyspareunia: Painful intercourse.
Tampon Difficulty: Problems using tampons.
Childbirth Complications: Potential issues during delivery.
Management: Surgical correction is used to remove the septum, creating a single vaginal canal.
Vaginal Agenesis (Mayer-Rokitansky-Küster-Hauser (MRKH) Syndrome): This is the absence of a vagina. The vaginal canal does not develop properly. The uterus may be present and functioning or also absent.
Management: Focuses on creating a neovagina (new vagina) to allow for sexual intercourse. Techniques include:
Tissue Grafting: Using skin or tissue to create a vaginal canal.
Balloon Dilation: Using a balloon to gradually create space.
Bowel Vaginoplasty: Using a segment of bowel to construct a vagina.
Vaginal Dilators: Used to create and maintain vaginal depth and width.
Vaginal Atresia: This refers to narrowing or closure of the vagina. The vaginal canal is abnormally constricted or completely closed.
Anomalies of the Cervix
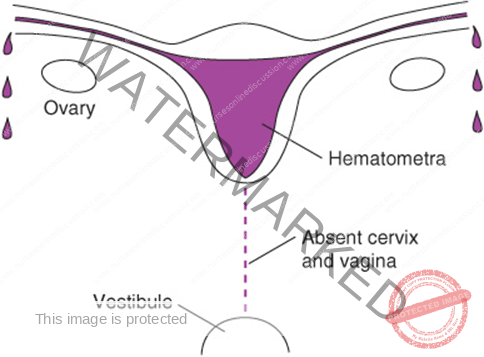
Cervical Agenesis: This is the absence of the cervix. The cervix, the lower part of the uterus, does not develop.
Clinical Features:
Amenorrhea: No menstruation.
Infertility: Inability to conceive.
Hematometra: Blood accumulation in the uterus because it cannot drain.
Management: Complex and depends on individual circumstances. It may involve:
Surgical Reconstruction: In some cases, surgical options may be explored.
Assisted Reproductive Technologies (ART): Options like surrogacy may be considered for fertility.
Cervical Hypoplasia: This is the underdevelopment of the cervix. The cervix is smaller than normal.
Symptoms:
Menstrual Irregularities: Abnormal periods.
Recurrent Pregnancy Loss: Repeated miscarriages.
Cervical Incompetence: Cervix weakens early in pregnancy, potentially leading to premature birth.
Fertility Problems: Difficulty conceiving.
Management: Varies depending on severity.
Fertility Treatments: To address conception challenges.
Surgical Correction: May be considered in some cases.
Cerclage: Stitching the cervix during pregnancy to prevent premature birth in cases of cervical incompetence.
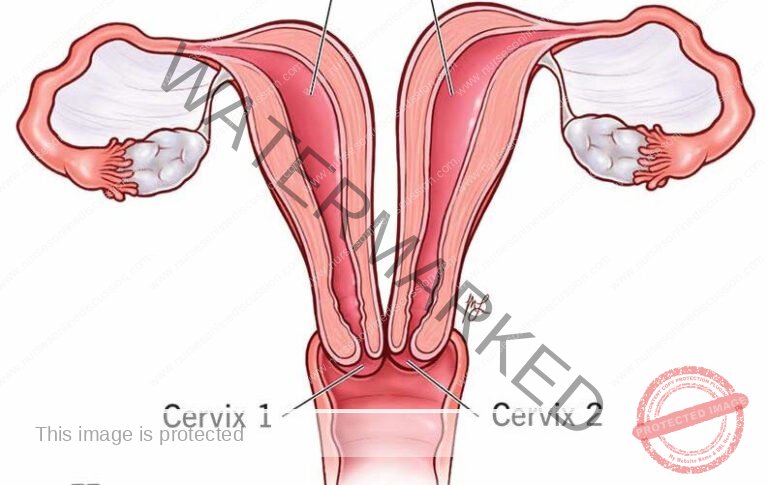
Cervical Duplication: This is when there are two cervical canals. Often associated with uterine duplication (double uterus).
Potential Effects:
Obstetric Complications: Potential difficulties during labor and delivery.
Management:
Surgical Correction: May be considered in some cases.
Monitoring During Pregnancy: Careful observation during pregnancy to manage potential complications.
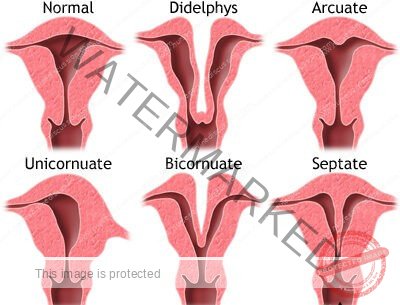
Anomalies of the Uterus
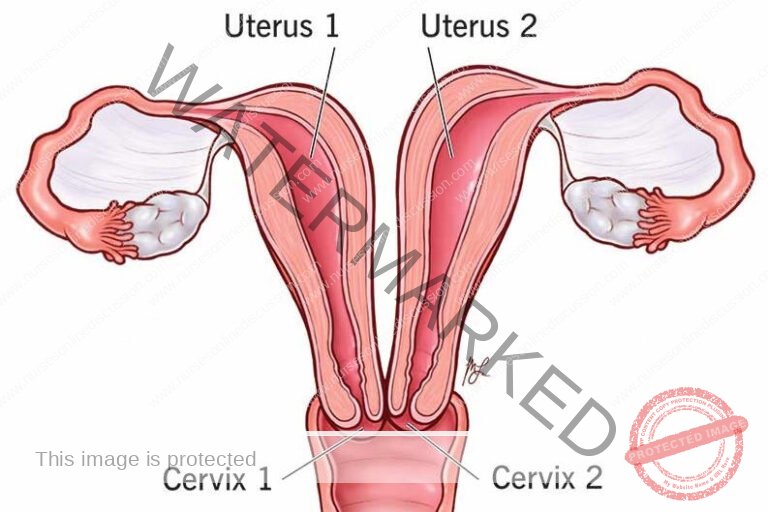
Uterine Duplication: This is when there are two separate uterine cavities. Each uterus may have its own cervix, and in rare cases, separate vaginas as well.
Potential Effects:
Menstrual Irregularities: Abnormal periods.
Infertility: Difficulty conceiving.
Recurrent Miscarriages: Repeated pregnancy losses.
Management:
Surgical Unification: Surgical procedures to join the two uterine cavities into one may be considered if symptomatic.
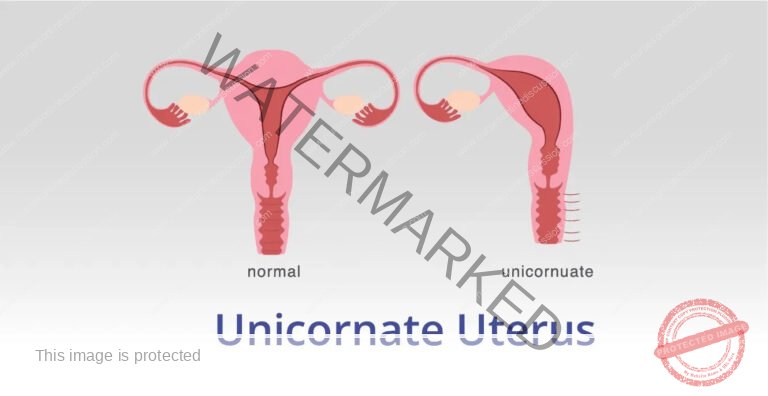
Unicornuate Uterus: In this anomaly, the uterus develops from only one Müllerian duct instead of two. This results in a single uterine horn, making the uterus half the usual size and horn-shaped.
Potential Effects:
Increased Miscarriage Risk: Higher chance of pregnancy loss.
Preterm Labor: Increased risk of premature birth.
Infertility: May experience difficulty conceiving.
Management:
Pregnancy Monitoring: Close observation during pregnancy to manage potential complications.
Surgical Interventions: Surgery may be considered in specific situations, but is not always necessary.
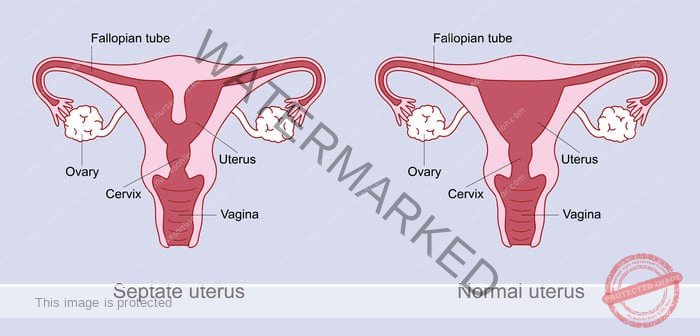
Septate Uterus: A fibrous or muscular wall (septum) divides the uterine cavity. This septum can vary in length, partially or completely separating the uterus.
Symptoms:
Infertility: Difficulty getting pregnant.
Recurrent Pregnancy Loss: Repeated miscarriages.
Management:
Hysteroscopic Metroplasty: A surgical procedure performed through the cervix using a hysteroscope to remove the septum, restoring a single uterine cavity.
Uterine Agenesis: This is the complete absence of the uterus. It is often a component of Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome.
Management:
Neovaginal Creation: Focuses on surgically creating a vagina to allow for sexual intercourse.
Gestational Surrogacy: For women desiring biological children, gestational surrogacy is the only option, as they cannot carry a pregnancy themselves.

Arcuate Uterus: This is considered a uterine variation, not a true anomaly. The fundus (top) of the uterus has a slight indentation, giving the uterine cavity a heart-shaped appearance. The indentation is typically shallow.
Significance: Often considered a normal variant and generally does not cause problems with fertility or pregnancy.
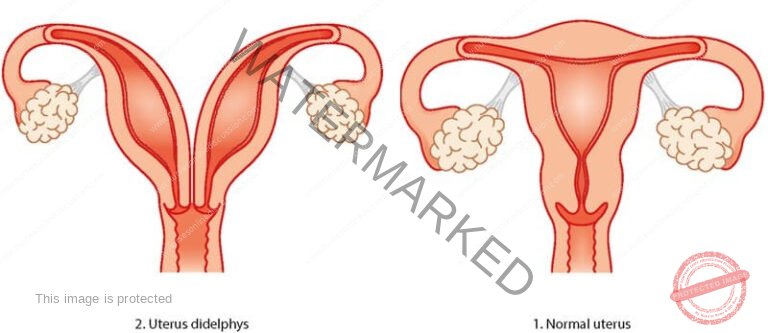
Didelphys Uterus (Uterus Didelphys): This involves complete duplication of the uterus. There are two separate uterine bodies (horns), each with its own cervix, and sometimes, two vaginas.
Potential Effects:
Pregnancy Complications: Higher risk of:
Preterm Birth: Premature delivery.
Ectopic Pregnancy: Pregnancy outside the uterus.
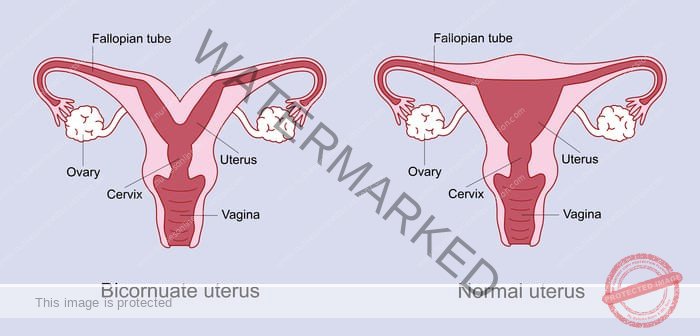
Bicornuate Uterus: The uterus has two horns that are partially fused. There is a single cervix, but the uterine cavity is partially or completely divided, creating a heart shape externally but with a partial or full internal separation.
Potential Effects: Similar to Didelphys Uterus, increased risk of:
Miscarriage: Pregnancy loss.
Preterm Labor: Premature delivery.
Ectopic Pregnancy: Pregnancy outside the uterus.
Anomalies of the Fallopian Tubes

Fallopian Tube Agenesis: This is the absence of one or both fallopian tubes. One or both tubes fail to develop.
Potential Effects:
Infertility: The impact on fertility depends on whether one or both tubes are absent and if the remaining tube is functional. Infertility is likely if both are absent or the remaining tube is blocked or damaged.
Management:
Assisted Reproductive Technologies (ART): In vitro fertilization (IVF) is often the primary option to achieve pregnancy, bypassing the need for functional fallopian tubes for egg transport.
Accessory Fallopian Tubes: This is the presence of extra fallopian tubes in addition to the normal pair. Extra, smaller tubes branch off from the main fallopian tubes.
Potential Effects:
Increased Ectopic Pregnancy Risk: The extra tubes may increase the risk of pregnancy implanting outside the uterus (ectopic pregnancy).
Management:
Surgical Removal: Surgical removal of the accessory tubes may be recommended to reduce the risk of ectopic pregnancy.
Tubal Duplication: This is the presence of duplicated segments within the fallopian tubes. Parts of the fallopian tube are doubled or branched.
Potential Effects:
Infertility: Can impair egg transport and fertilization.
Ectopic Pregnancies: Increased risk of pregnancies outside the uterus.
Management:
Corrective Surgery: Surgical repair may be attempted to correct the tubal structure and improve fertility.
Tubal Atresia: This refers to the underdevelopment or closure of one or more segments of the fallopian tubes. A section of the fallopian tube is narrowed, blocked, or missing.
Potential Effects:
Impaired Egg Transportation: The blockage or narrowing prevents the egg from traveling to the uterus.
Infertility: Leads to inability to conceive naturally.
Management:
Surgery: Surgical options may be considered to attempt to open or repair the blocked tube, depending on the extent and location of the atresia.
IVF: In vitro fertilization is often a more effective option to bypass tubal issues and achieve pregnancy.“`
(a) Forms of Birth-Related Irregularities in the Female Reproductive Organs:
Uterine Birth Defects:
Septate Uterus: The uterus is divided by a wall (septum), either partially or entirely, within its cavity.
Bicornuate Uterus: A uterus presenting with two distinct horn-shaped structures.
Unicornuate Uterus: A uterus that has developed with a single horn.
Uterus Didelphys: Characterized by two separate uterine bodies and two cervixes.
Vulvar Birth Defects:
Labial Hypoplasia: Underdeveloped or unusually small labia.
Labial Hypertrophy: Enlarged or excessively sized labia.
Hymenal Birth Defects:
Imperforate Hymen: A hymen that completely obstructs the vaginal opening.
Microperforate Hymen: A hymen featuring an extremely small opening.
Septate Hymen: A hymen with a band of tissue traversing the opening.
Vaginal Birth Defects:
Transverse Vaginal Septum: A tissue wall that divides the vagina horizontally.
Vertical or Complete Vaginal Septum: Total blockage of the vagina due to a septum.
Vaginal Agenesis: Absence or incomplete development of the vagina.
Cervical Birth Defects:
Cervical Agenesis: Absence or incomplete development of the cervix.
Cervical Duplication: The presence of two cervixes.
(b) Protective Actions Against Birth Irregularities:
Genetic Consultation: Seeking advice from genetic counselors before pregnancy to evaluate the chances of birth defects based on family health history and genetic elements.
Antenatal Care: Consistent prenatal appointments and screenings to aid in early detection and management of potential irregularities.
Teratogen Avoidance: Steering clear of harmful substances like tobacco products, alcoholic beverages, illicit drugs, and certain medications during pregnancy.
Optimal Diet: Maintaining a well-rounded diet abundant in key nutrients, notably folic acid, to aid in preventing specific birth irregularities.
Immunizations: Ensuring all recommended vaccinations are current to safeguard against infections that can lead to fetal irregularities.
Safe Environment: Taking safety measures to limit exposure to environmental risks such as radiation, chemicals, and pollutants.
Chronic Condition Management: Effectively managing pre-existing chronic conditions, such as diabetes or hypertension, before and during pregnancy to lower the risk of birth irregularities.
Genetic Screening: Considering genetic screening, such as carrier tests, to pinpoint any possible genetic irregularities before conception.
Infection Prevention: Taking steps to prevent infections during pregnancy, as certain infections can elevate the risk of birth irregularities.
Emotional Well-being: Seeking emotional support and counseling to handle stress and worry during pregnancy, as these factors can influence fetal growth.
Common Signs
Primary Amenorrhea: Lack of menstruation by age 16.
Irregular Menstrual Bleeding: Menstrual flow that is inconsistent or excessively heavy.
Pelvic Discomfort: Persistent or recurring pelvic pain.
Dyspareunia: Pain experienced during sexual activity.
Infertility Issues: Challenges in conceiving or maintaining a pregnancy to full term.
Repeated Miscarriages: Experiencing multiple pregnancy losses.
Unusual Genitalia Appearance: External genitalia that appear atypical or are ambiguous.
Urinary or Bowel Problems: Symptoms like difficulty urinating or bowel dysfunction.
Vaginal Mass or Protrusion: Feeling a lump or seeing a bulging tissue in the vaginal region.
Kidney Anomalies: Related kidney irregularities, such as missing a kidney or having a horseshoe kidney.
Standard Diagnostic Procedures for Birth Irregularities of the Female Reproductive System:
Clinical Assessment:
Detailed patient history, including family medical background.
Comprehensive physical exam to identify external genital issues and evaluate the general development of reproductive organs.
Imaging Assessments:
Ultrasound Imaging: A non-invasive method using sound waves to visualize reproductive organs and detect structural anomalies.
Magnetic Resonance Imaging (MRI): MRI provides in-depth images of reproductive organs, aiding in identifying complex irregularities.
Hormone Analysis:
Hormone Level Testing: Blood tests to assess reproductive system function and detect hormonal imbalances.
Genetic Examinations:
Genetic Testing: Techniques like karyotyping to identify chromosome abnormalities that could contribute to reproductive system birth irregularities.
Uterine and Fallopian Tube Examination (HSG):
Hysterosalpingography (HSG): An X-ray procedure using contrast dye injected into the uterus and fallopian tubes to assess their structure and find blockages or irregularities.
Minimally Invasive Visual Examination:
Laparoscopy: A minimally invasive surgical technique for direct visualization of reproductive organs using a small camera inserted through a small abdominal incision.
Tissue Analysis:
Biopsy: In certain instances, tissue sample collection for detailed examination to rule out underlying diseases.
Standard Treatment Approaches
Team-Based Care:
Multidisciplinary Team Approach: Management often involves a team of specialists including gynecologists, pediatricians, geneticists, psychologists, nurses, and others.
Surgical Solutions:
Surgical Interventions: Surgical correction may be needed for specific birth irregularities, such as obstructions in the vagina or uterus.
Timing of Surgery: Surgical timing depends on the specific irregularity and the individual’s age and development, potentially in infancy or after puberty and menstruation onset.
Non-Surgical Vaginal Creation:
Dilator Therapy: For individuals without a vagina at birth, dilator therapy can create a new vagina using a dilator to gradually stretch the vaginal area over several months.
Hormonal Regulation:
Hormonal Management: Hormone therapy may be used to regulate menstrual cycles, manage hormone imbalances, or address related conditions, alleviating symptoms like menstrual pain or irregularities.
Psychological and Social Support:
Emotional Support and Counseling: Coping with reproductive system birth irregularities can be emotionally difficult for individuals and families. Support, counseling, and groups offer guidance, education, and a safe space for sharing experiences.
Fertility Considerations:
Fertility Considerations: Fertility may be affected depending on the specific irregularity. Options for preserving fertility, such as egg or embryo freezing, may be discussed for future family planning.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

