Abortion
Subtopic:
Incomplete vs Complete Abortion
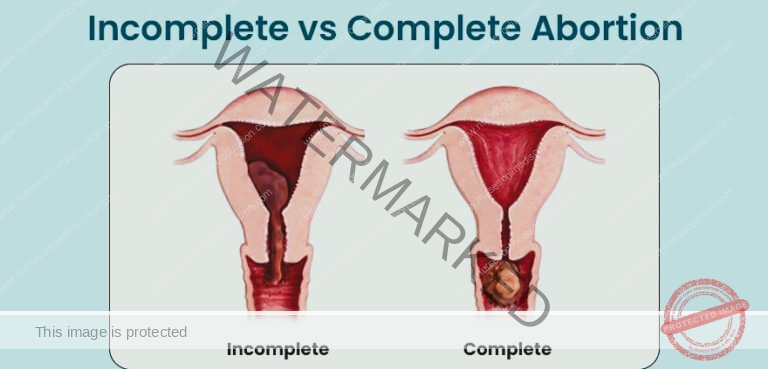
INCOMPLETE ABORTION
Incomplete abortion happens when some pregnancy material, specifically placental tissues (chorionic membranes), remain inside the uterus after a miscarriage.
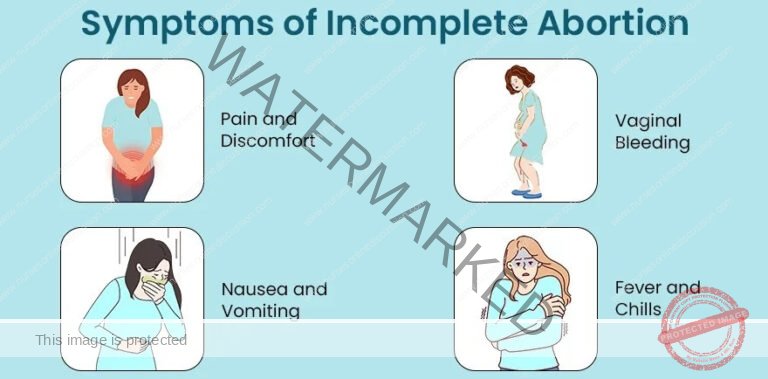
Clinical Features of Incomplete Abortion
Severe Vaginal Bleeding: Characterized by heavy and excessive vaginal bleeding, potentially including the passage of clots and tissue matter.
Abdominal Pain and Back Discomfort: Commonly involves abdominal pain, which can range from cramping to persistent, along with backache, signaling ongoing uterine contractions and tissue expulsion.
Partially Open Cervix: A physical exam might reveal the cervix is somewhat dilated and soft, indicating the abortion is incomplete and that pregnancy tissue is still in the uterus.
Enlarged Uterus: The uterus may feel larger than normal upon examination, suggesting retained tissue and blood are present within the uterine cavity.
Palpable Products of Conception: In some cases, retained pregnancy tissue may be felt during an abdominal examination.
Signs of Anemia: Symptoms like tiredness, weakness, and paleness can point to anemia caused by prolonged or significant bleeding from the incomplete abortion.
Shock Indicators: In serious situations, shock can occur, shown by symptoms such as rapid heartbeat, low blood pressure, and cold, clammy skin, reflecting the body’s reaction to substantial blood loss and poor circulation.
Fever and Shivering: The presence of fever and chills might indicate infection, a complication of incomplete abortion that requires prompt medical attention.
Offensive Vaginal Discharge: If infection is present, a foul-smelling vaginal discharge may occur, suggesting infection in the uterus or pelvis that needs medical assessment and treatment.
Emotional Distress: Dealing with the physical symptoms and the emotional impact of incomplete abortion can cause psychological distress, including feelings of sadness, worry, and depression.

MANAGEMENT OF INCOMPLETE ABORTION
Hospital Admission: Admit the patient to a gynecology unit for specialized care and monitoring.
Patient History: Gather a detailed medical history from the patient, including details about the pregnancy, symptoms, and any pre-existing conditions.
Emotional Support: Reassure the patient and their family to reduce anxiety and provide emotional comfort during this difficult time.
Laboratory Investigations: Inform the doctor to order essential blood tests, including Hemoglobin levels (HB), blood grouping, and cross-matching in preparation for potential blood transfusion.
Fluid Resuscitation: Start intravenous fluids to restore and maintain blood volume, especially if the patient has experienced significant blood loss.
Thermal Management (if in shock): If the patient is showing signs of shock, ensure they are kept warm to prevent hypothermia.
Vital Signs Monitoring: Regularly check and record vital signs such as blood pressure, pulse rate, respiration rate, and temperature to closely monitor the patient’s condition.
Informed Consent: Obtain informed consent from the patient for any medical or surgical procedures after explaining the necessary treatments and potential risks and benefits.
Uterotonic Medication: Administer medications like oxytocin or misoprostol to help the uterus contract strongly, expel any remaining pregnancy tissue, and control excessive bleeding.
Manual Removal of Tissue (if visible): If products of conception are visible in the vagina, carefully remove them using sterile gloves to prevent infection and further bleeding.
ABCs Assessment: Continuously monitor the patient’s Airway, Breathing, and Circulation to ensure they are stable and to promptly address any emergencies.
Blood Transfusion (if needed): Transfuse blood products according to the patient’s Hemoglobin results and clinical condition to correct anemia and blood loss.
Theatre Preparation: Prepare the patient for a potential surgical procedure in the operating theatre. This includes shaving the area if necessary, dressing the patient in a sterile gown, and informing the theatre staff about the case.
Surgical Evacuation: Once the patient is stable, surgically evacuate the uterus under general anesthesia in the operating theatre. Manual vacuum aspiration is generally recommended as an effective method to remove any retained products of conception.
Post-Evacuation Medication: Misoprostol (400-800 mcg every 6 hours orally) or Oxytocin may be prescribed after the procedure to further help contract the uterus and minimize ongoing blood loss.
Rh Immunoglobulin (if Rh-negative): If the patient is Rhesus negative, administer Anti-D immunoglobulin 300 μg intramuscularly as a single dose to prevent Rh sensitization.
Prophylactic Antibiotics: Administer antibiotics to prevent infection, a potential complication following an incomplete abortion or surgical evacuation.
Iron and Folic Acid Supplementation: Prescribe ferrous sulfate and folic acid supplements to help replenish iron stores and prevent iron-deficiency anemia, especially after blood loss.
Nutritional Support: Encourage a well-balanced, nutritious diet to aid in recovery and overall health.
Discharge Advice:
Rest: Advise the patient to get adequate rest at home to facilitate physical and emotional recovery.
Nutrition: Emphasize the importance of maintaining a nutritious diet to support healing and regain strength.
Follow-up Appointments: Ensure the patient understands the need to return for all scheduled follow-up reviews to monitor their recovery and address any complications.
Medication Adherence: Instruct the patient to take all prescribed medications as directed, completing the full course, even if symptoms improve.
Antenatal Care: Advise the patient to attend antenatal care clinics if they plan future pregnancies for preconception counseling and optimal pregnancy management.
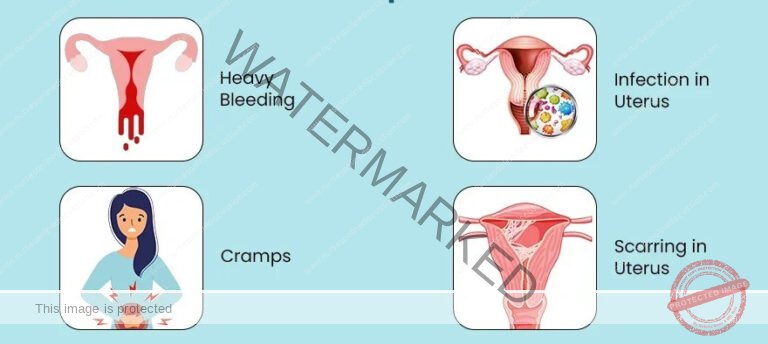
Complications of Incomplete Abortion
Hemorrhagic Shock: Severe blood loss from an incomplete abortion can trigger hemorrhagic shock. This is a dangerous condition where vital organs don’t get enough blood flow, potentially leading to rapid heartbeat, dangerously low blood pressure, and organ malfunction.
Anemia: Prolonged or heavy bleeding during an incomplete abortion can result in anemia. This condition is characterized by a low count of red blood cells, which can cause symptoms like persistent tiredness, weakness, and shortness of breath.
Sepsis (Infection): Incomplete abortion increases the risk of infection within the uterus. This can escalate to sepsis, a life-threatening condition where the body overreacts to an infection. Signs of sepsis can include high fever, rapid breathing, increased heart rate, and confusion.
Uterine Perforation (Rare): Though uncommon, procedures during an incomplete abortion can sometimes cause a uterine perforation, which is a tear or hole in the uterine wall.
Retained Tissue: Incomplete abortions can leave fetal or placental tissue behind in the uterus. This retained tissue elevates the risk of infection, continued bleeding, and ongoing symptoms.
Potential Fertility Issues: Repeated or severe incomplete abortions might raise concerns about their long-term effects on a woman’s future ability to conceive and maintain healthy pregnancies.
Emotional and Psychological Distress: Dealing with the physical and emotional realities of an incomplete abortion can be emotionally challenging, potentially leading to feelings of sadness, guilt, and heightened anxiety.
COMPLETE ABORTION
Complete abortion is when all pregnancy-related tissues are naturally expelled from the uterus.
Clinical Features of Complete Abortion
Pain Resolution: After a complete abortion, the previously experienced abdominal pain and cramping will stop, signaling that all pregnancy tissue has been successfully expelled from the uterus.
Minimal Vaginal Bleeding: Vaginal bleeding will be light or very minimal following a complete abortion, indicating the natural stopping of uterine bleeding as pregnancy tissues are fully expelled.
Uterus Returns to Normal Size: A physical exam will likely show a well-contracted uterus, meaning the uterine muscles have effectively expelled all fetal and placental tissues, allowing the uterus to return to its normal size and firmness.
Pregnancy Symptoms Fade: As pregnancy-related tissues are expelled during a complete abortion, pregnancy signs and symptoms, such as breast tenderness, nausea, and fatigue, will typically decrease and eventually disappear, showing the pregnancy has ended.
Emotional Relief and Closure: After a complete abortion, individuals may feel a sense of relief and emotional closure as the physical symptoms and uncertainty linked to the pregnancy complication are resolved.
Negative Pregnancy Test Result: A pregnancy test taken after a complete abortion is expected to be negative, confirming the absence of pregnancy hormones in the body.
Management of Complete Abortion
No Uterine Evacuation Needed: Surgical evacuation of the uterus is generally not required in a complete abortion as the uterus is already empty.
Monitor Bleeding: Observe the patient to ensure vaginal bleeding remains light and does not become heavy.
Follow-up Care: Schedule a follow-up appointment to check on the woman’s overall recovery and well-being after the abortion.
Rest Recommendation: Advise the woman to get sufficient bed rest to aid in physical recovery.
Anti-D for Rh-Negative Mothers: For mothers who are Rhesus negative, administer Anti-D immunoglobulin 300 μg IM in a single dose within 72 hours to prevent Rh sensitization.
Return Precautions: Instruct the woman to seek immediate medical attention if bleeding restarts or becomes heavy, or if she develops a fever, as these could indicate infection or other complications.
Important Note: If there is no ongoing active bleeding and an ultrasound confirms that the uterine cavity is empty, no further medical or surgical intervention is needed, and hospital admission is usually not necessary.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

