Sexually Transmitted Infections (STIs)
Subtopic:
Syndromic management of STI
Syndromic approach
The syndromic approach is a method used for managing sexually transmitted infections (STIs). It relies on identifying and treating STIs based on the observable signs and symptoms presented by the patient, rather than solely depending on laboratory tests for confirmation.
Instead of pinpointing a precise germ causing the infection, this approach addresses the groups of symptoms (syndromes) that are typically linked with different STIs.
This strategy is especially valuable where laboratory testing is not easily accessible or is limited. In such situations, it allows for timely and effective treatment based on clinical presentation.
Advantages of using Syndromic Approach
Enhanced Clinical Diagnosis: Syndromic methods can improve STI diagnosis in clinics. Healthcare providers can treat based on symptoms and observable signs, even without lab tests. This reduces incorrect diagnoses and ineffective treatments.
User-Friendly for Primary Care: This approach is simple for primary healthcare staff to learn and apply. It doesn’t need complex tools or specialist training, making it suitable for areas with limited resources where lab tests are scarce.
Fast Diagnosis and Treatment: Syndromic management enables quick STI diagnosis and treatment because it bypasses waiting for lab results. This helps in preventing complications and limiting STI spread.
Immediate Treatment for Symptomatic Cases: Patients showing symptoms can receive treatment in a single visit, removing the need for multiple appointments for lab work. This speeds up patient care and improves convenience.
Economical: This method is more cost-effective compared to lab-based testing. It avoids the need for pricey equipment and supplies, making it a more sustainable option in resource-constrained environments.
Accessible at Basic Health Facilities: Treatment becomes available at the first point of contact within the health system, extending STI management to lower-level health units. Referrals are then reserved for complicated situations.
Preventive Partner Care: The syndromic approach includes treating sexual partners, which is crucial for preventing re-infection and breaking the chain of transmission.
Efficient Resource Use: It optimizes resource use by reducing reliance on lab testing, making it well-suited for settings where resources are scarce.
Improved Treatment Access: Syndromic methods can increase access to STI treatment. Healthcare providers can start treatment without waiting for lab confirmations. This is particularly vital where lab access is limited for patients.
Disadvantages of using Syndromic Approach
Missed Asymptomatic Infections: Individuals without symptoms, especially women, might be overlooked. This approach is less effective in finding and treating silent infections.
Potential Medication Overuse: It can lead to unnecessary drug use, as individuals might be treated for STIs they don’t actually have. This is especially concerning when resources are limited.
Limited Diagnostic Accuracy for Some Infections: Symptoms and signs, particularly in women, may not accurately predict certain STIs like gonorrhea and chlamydia. This can result in missed or delayed diagnoses and proper treatments.
Risk of Antibiotic Resistance: Over-reliance on syndromic treatment can contribute to antibiotic resistance. Broad-spectrum antibiotics are frequently used without identifying the specific infection-causing pathogen.
Complexities with Co-infections: Managing co-infections with multiple pathogens can be challenging. This method focuses on a single syndrome and might miss other STIs present concurrently. For example, someone with genital ulcers from herpes or syphilis might also have chlamydia or gonorrhea. This can lead to insufficient treatment and possible issues.
Limited Effectiveness for Viral Infections: It may be less effective for viral STIs. Antiviral drugs often require knowing the specific virus, which the syndromic approach doesn’t provide.
Possibility of Misdiagnosis: Syndromic methods can lead to incorrect STI diagnoses. It’s not always possible to accurately pinpoint the exact STI based only on clinical signs and symptoms, which can result in wrong treatments and potential problems.
Inadequate Care for Asymptomatic Cases: This approach is not sufficient for individuals with STIs who don’t show symptoms, particularly women. This can result in untreated infections and possible health issues.
NOTE:
There are different ways to diagnose and manage STIs:
Clinical Method: Identifying and treating a specific STI based on observable signs and symptoms, guided by clinical experience.
Laboratory Testing Method: Identifying and managing STIs by determining the specific organisms causing the infection through lab tests.
Syndromic Method: Identifying and treating all possible organisms that could be causing a group of symptoms and signs related to an STI syndrome.
In current situations, the benefits of the syndromic approach are greater than its drawbacks. A theoretical cost comparison of these three methods for diagnosing 500 patients with genital ulcers, 500 with urethral discharge, and 500 with vaginal discharge found that the clinical and lab-based approaches each cost 2-3 times more than the syndromic method. Personnel costs and the consequences of incorrect diagnoses were the main reasons for this difference. By treating all STIs that can cause a syndrome, syndromic diagnosis helps avoid many complications. Even in developed countries, many healthcare providers prefer syndromic methods to avoid treatment delays while waiting for lab results.
RATIONALE OF SYNDROMIC APPROACH
Limited Lab Resources: Many healthcare settings, especially in resource-limited areas, may have limited or no lab facilities for STI testing. The syndromic approach allows for STI diagnosis and treatment based on clinical symptoms and signs, removing the need for lab confirmation.
Multiple Organisms Cause STI Syndromes: Most STI syndromes can be caused by several different organisms. For example, urethral discharge in men can be caused by Chlamydia trachomatis, Neisseria gonorrhoeae, or Trichomonas vaginalis. The syndromic approach uses broad-spectrum antibiotics effective against a wide range of organisms, ensuring treatment even when the specific cause is unknown.
Delayed Lab Results: Even when labs are available, test results might not be immediate. Patients may not return for results and treatment, causing delays and increasing transmission risk. The syndromic approach allows for immediate treatment, reducing complications and spread.
Common Mixed Infections: It’s common for patients to have mixed infections (infected with more than one STI). The syndromic approach uses broad-spectrum antibiotics effective against a variety of organisms, increasing the chance of treating all infections present.
Influence of Self-treatment and Immunity on Symptoms: Self-medication and the body’s immune response can change how STIs present clinically, making specific diagnosis based on symptoms alone difficult. The syndromic approach offers a standardized treatment plan that is effective regardless of the specific organism or the impact of self-treatment and immunity.
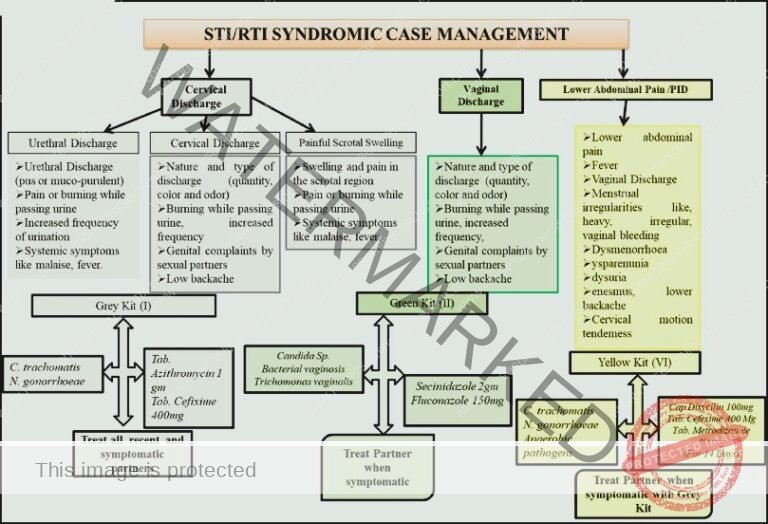
STD Syndromic Treatment Flow Charts (Algorithms)
Diagnosis and treatment flowcharts, which put the Syndromic Approach into practice, have been developed. These charts offer step-by-step directions for healthcare staff to diagnose and manage STDs using suggested medications.
STD syndromic treatment flow charts, also known as algorithms, present several benefits for diagnosing and handling sexually transmitted infections (STIs):
Focused and Enhanced Diagnostic Accuracy: Algorithms are structured to concentrate on the specific signs and symptoms of STIs. This guides healthcare providers towards more precise diagnoses by directly addressing the patient’s presenting issues.
Educational Resource for Primary Healthcare Workers: These algorithms act as valuable learning aids for frontline healthcare providers, including those who may not have extensive experience in STI management. They simplify complex diagnostic processes.
Uniformity in Treatment Protocols: Algorithms encourage the use of standardized STI treatment methods across different healthcare environments and among various providers. This consistency helps ensure that patients receive appropriate, evidence-based care, and reduces inconsistencies in treatment approaches.
Improved Disease Tracking: Algorithms facilitate the systematic collection of essential data on STI diagnoses and treatments administered. This data is crucial for public health surveillance, tracking infection trends, and assessing the effectiveness of STI control initiatives and programs.
Tool for Evaluating Training Effectiveness: Algorithms can be employed to measure how well STI training programs improve healthcare providers’ skills. By comparing diagnostic and treatment practices before and after training, the impact of educational interventions can be effectively evaluated.
Single-Visit Diagnosis and Care: Algorithms enable the complete process of STI diagnosis and treatment to be carried out within a single patient visit. This improves convenience for patients and lowers the chance of ongoing transmission by ensuring immediate care. This is especially important where patient access to healthcare is limited or follow-up visits are challenging.

STI SYNDROMES
Most Common:
Urethral Discharge: Secretion or fluid coming from the urethra. This is often a key indicator of infection in men.
Unusual Vaginal/Cervical Discharge: Any discharge from the vagina or cervix that is different in color, amount, or odor from normal. This can signal infection in women.
Genital Ulcers: Open sores or lesions appearing on the genital area. These can be painful or painless and are a sign of various infections.
Lower Abdominal Pain: Pain felt in the lower belly region. In women, this can be associated with pelvic inflammatory disease (PID) and STIs.
Swollen Groin Lymph Nodes (Bubo): Enlargement of lymph nodes in the groin area. This swelling can be a reaction to infection in the genitals or lower body.
Other Syndromes:
Painful Scrotal Swelling: Pain and swelling in the scrotum or testicles. This can indicate epididymitis or other infections.
Bartholin’s Abscess: A painful, pus-filled swelling near the vaginal opening, resulting from a blocked Bartholin’s gland.
Conjunctivitis with Pus in Newborn (Ophthalmia Neonatorum): Eye infection in newborns, characterized by pus discharge. Typically contracted during birth from an infected mother.
Genital Growths: Abnormal growths or bumps appearing on the genital area. These may be caused by viruses like HPV.
Inflammation of Glans and Foreskin (Balanitis): Redness and swelling of the head of the penis (glans) and foreskin (prepuce). Often due to infection or irritation.
Acquired Immunodeficiency Syndrome (AIDS): The late stage of HIV infection, characterized by a severely weakened immune system and susceptibility to opportunistic infections.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2026 Nurses online discussion. All Rights Reserved

