Anatomy of the Female and Male Reproductive Organ
Subtopic:
The Male Reproductive Organs

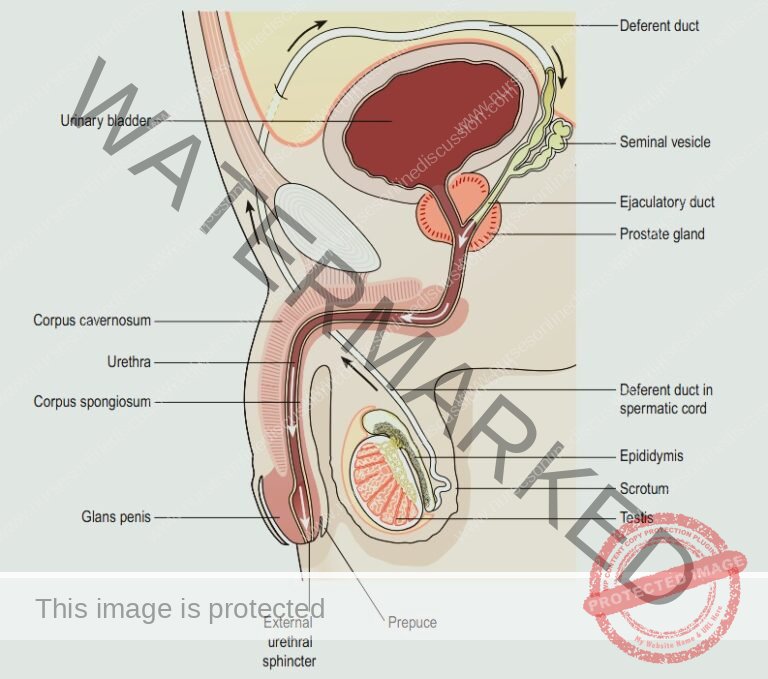
Male Reproductive System
The male reproductive system is composed of organs including the testes, a network of tubes (comprising the epididymis, ductus deferens, ejaculatory ducts, and urethra), accessory reproductive glands (seminal vesicles, prostate, and bulbourethral glands), and various supporting structures, notably the scrotum and the penis.
Functions of Male Reproductive Organs
The male reproductive system performs functions essential for both reproduction and the removal of urinary waste.
Testes:
Sperm Production (Spermatogenesis): The testes are the site of spermatogenesis, the process of generating mature sperm cells ready for fertilization.
Sperm Maturation and Storage: The epididymis is crucial for sperm to mature and develop the capacity for motility. It also acts as a storage location for sperm until ejaculation.
Epididymal Maturation: Within the epididymis, sperm undergo further development, gaining improved movement capabilities and the ability to fertilize an egg.
Testosterone Production: The testes produce testosterone, the primary male sex hormone, which is vital for sperm creation and the development of male secondary sexual characteristics. Testosterone levels are regulated by a hormonal axis involving the hypothalamus and pituitary gland.
Ejaculatory Duct:
Vas deferens: These tubes carry mature sperm from the epididymis towards the ejaculatory duct. Muscle contractions within the walls of the vas deferens aid in moving sperm along during ejaculation.
Seminal Vesicles, Prostate Gland, and Bulbourethral Glands:
Secretion Contribution: These glands produce and contribute various secretions that together form semen. These secretions are important for enhancing sperm viability and motility.
Semen Nourishment and Protection: Semen provides nutrients and protective elements for sperm, ensuring their survival and function as they travel through the female reproductive system.
Penis and Urethra:
Copulation and Sperm Delivery: The penis is the organ responsible for copulation. It facilitates the deposition of sperm into the female reproductive tract, enabling fertilization.
Urethra Function: The urethra serves as a shared pathway for both semen during ejaculation and urine during urination, allowing for the elimination of both types of fluid from the body.
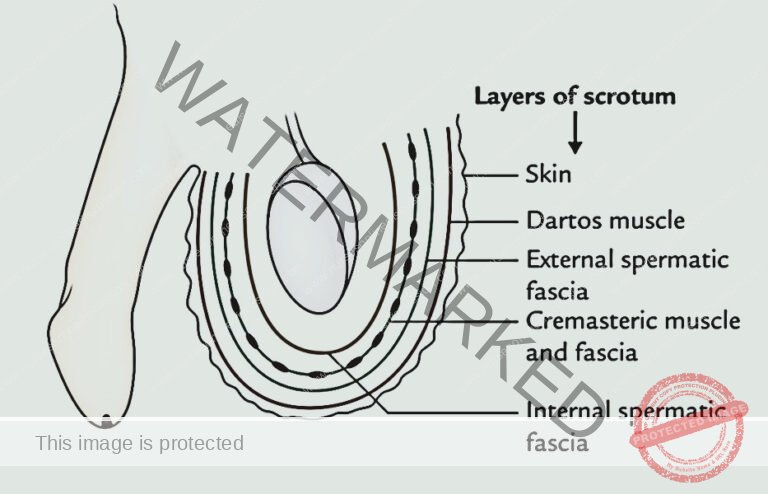
Scrotum
The scrotum is a skin sac composed of pigmented skin, fibrous connective tissue, and smooth muscle.
It’s internally divided into two separate chambers, each designed to house one testis, one epididymis, and the testicular end of the spermatic cord.
Positioned inferior to the pubic symphysis, it resides anterior to the upper thighs and posterior to the penis.
Outwardly, the scrotum appears as a single pouch of skin, but it’s visibly divided into lateral sections by a central ridge known as the raphe.
Internally, a structure called the septum divides the scrotum into two sacs. The septum is formed from a subcutaneous layer and muscle tissue that includes the dartos muscle, which consists of bundles of smooth muscle fibers.
Associated with each testis within the scrotum is the cremaster muscle, composed of small bands of skeletal muscle. These bands descend as extensions of the internal oblique muscle through the spermatic cord to encircle the testes.
The scrotum’s location and the contraction of its muscle fibers are crucial for regulating testicular temperature. Optimal sperm production necessitates a temperature approximately 2 to 3°C lower than normal body temperature. This reduced temperature is maintained because the scrotum is situated outside the pelvic cavity.
When exposed to cold temperatures, the cremaster and dartos muscles react. Contraction of the cremaster muscle elevates the testes, bringing them closer to the body for warmth absorption.
Contraction of the dartos muscle makes the scrotal skin tight and wrinkled, which diminishes surface area and thus reduces heat loss. Conversely, exposure to warmth reverses these muscle actions to dissipate heat.
Testes
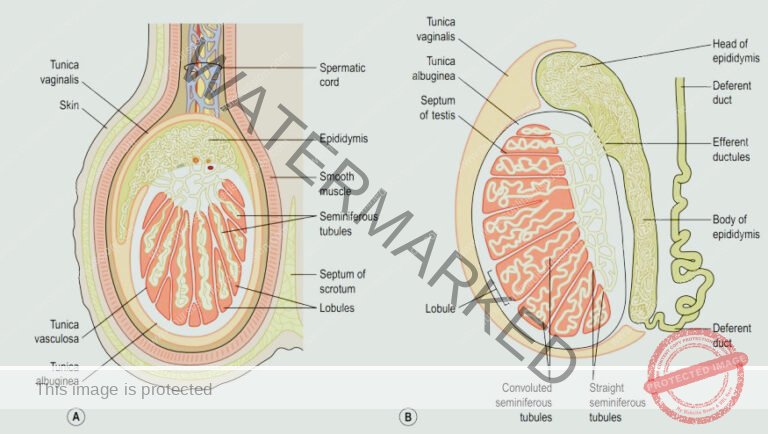
The testes are recognized as the primary male reproductive glands, functioning analogously to the ovaries in females.
They measure roughly 4.5 cm in length, 2.5 cm in width, and 3 cm in thickness, and are held within the scrotum by the spermatic cords.
They are enclosed by three tissue layers:
Tunica vaginalis: This is a dual-layered membrane that constitutes the outer covering of the testes. It originates as an extension from the abdominal and pelvic peritoneum. During fetal development, the testes initially form in the lumbar region of the abdominal cavity, situated just below the kidneys. They subsequently descend into the scrotum, drawing with them layers of the peritoneum, along with blood vessels, lymphatic channels, nerves, and the vas deferens. The peritoneum eventually encapsulates the testes within the scrotum but separates from the abdominal peritoneum. The complete descent of the testes into the scrotum is typically achieved by the eighth month of fetal development.
Tunica albuginea: Situated beneath the tunica vaginalis, this is a dense, fibrous layer. Inward extensions of the tunica albuginea form septa, which partition the internal structure of each testis into lobules. Each of these approximately 200-300 lobules contains one to three tightly packed structures known as the seminiferous tubules, which are the sites of sperm production. The process of sperm formation within the seminiferous tubules is termed spermatogenesis. The seminiferous tubules are composed of two main cell types: spermatogenic cells, which are sperm-forming cells, and Sertoli cells (also known as sustentacular cells). Sertoli cells play multiple supportive roles in spermatogenesis. They provide nourishment to spermatocytes, spermatids, and sperm; eliminate excess cytoplasm from spermatids as they mature; regulate the progression of spermatogenic cells through development; and control the release of sperm into the lumen of the seminiferous tubules. Sertoli cells also produce fluid that aids in sperm transport, secrete the hormone inhibin, and regulate the responses to testosterone and FSH (follicle-stimulating hormone).
Tunica vasculosa: The tunica vasculosa forms the vascular layer of the testis. It is an inner layer consisting of a network of blood vessels, held together by delicate connective tissue.
Spermatic Cords / Vas Deferens
The spermatic cords act as suspension structures, securing the testes within the scrotum.
Each spermatic cord is a complex bundle containing: a testicular artery, testicular veins, lymphatic vessels, the vas deferens (also known as the deferent duct), and testicular nerves. These components consolidate to form the cord as they descend from their origin points in the abdominal region.
The spermatic cord itself is encased in a protective layer composed of smooth muscle along with connective and fibrous tissues. It extends through the inguinal canal, a pathway from the abdomen to the scrotum, and attaches to the testis at its posterior aspect.
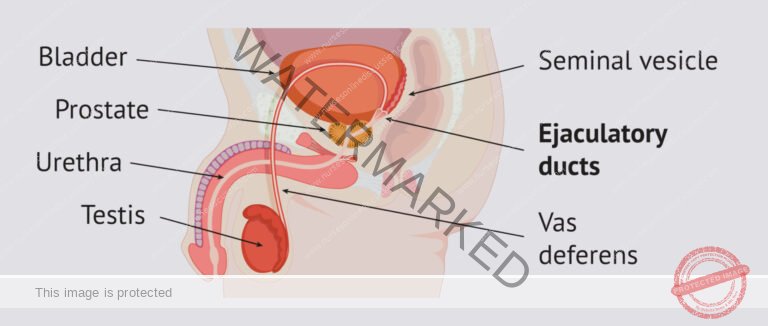
The vas deferens, a key component of the spermatic cord, is approximately 45 cm in length. It originates at the testis and ascends upwards through the inguinal canal. From there, it courses medially towards the posterior wall of the bladder, where it converges with the duct from the seminal vesicle to form the ejaculatory duct, a crucial part of the male reproductive pathway.
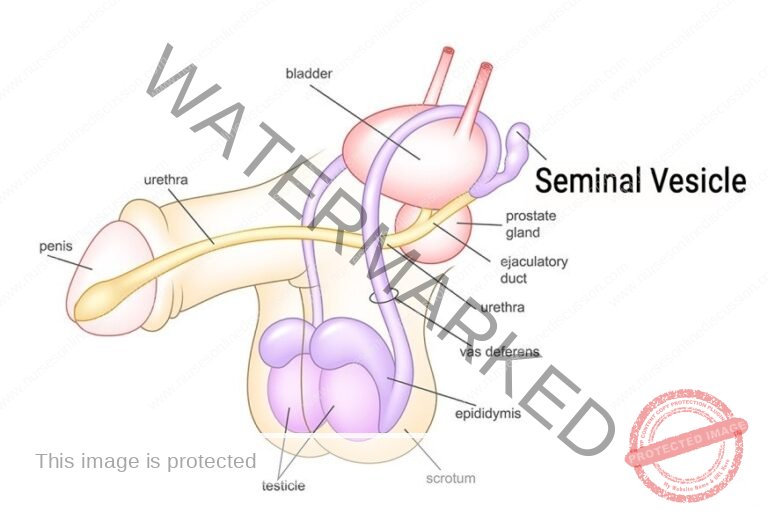
Seminal Vesicles
The seminal vesicles consist of two small sacs, approximately 5 cm in length, composed of fibromuscular tissue. They are lined internally with a columnar epithelial layer and are located on the posterior side of the bladder.
Towards their distal end, each seminal vesicle tapers into a short excretory passage. This passage then merges with the corresponding vas deferens to create the ejaculatory duct.
Functions
During ejaculation, the seminal vesicles undergo muscular contractions to discharge their stored secretions, known as seminal fluid.
Seminal fluid, which constitutes about 60% of the total semen volume, has an alkaline nature. This alkalinity is crucial to counteract the acidic environment of the vaginal tract, thereby safeguarding sperm viability. Additionally, seminal fluid is rich in fructose, a sugar that serves as a primary energy source to nourish and energize the sperm as they navigate the female reproductive pathways.
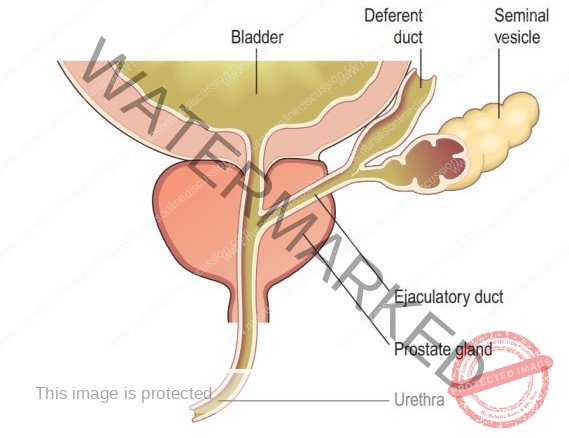
Ejaculatory Ducts
The ejaculatory ducts are constituted by two small tubes, each approximately 2 cm in length. They are formed through the joining of the duct from a seminal vesicle and a vas deferens.
These ducts traverse through the prostate gland and subsequently connect to the prostatic urethra. Their primary role is to transport seminal fluid and spermatozoa into the urethra.
The structural composition of the ejaculatory duct walls is similar in tissue layering to that of the seminal vesicles.
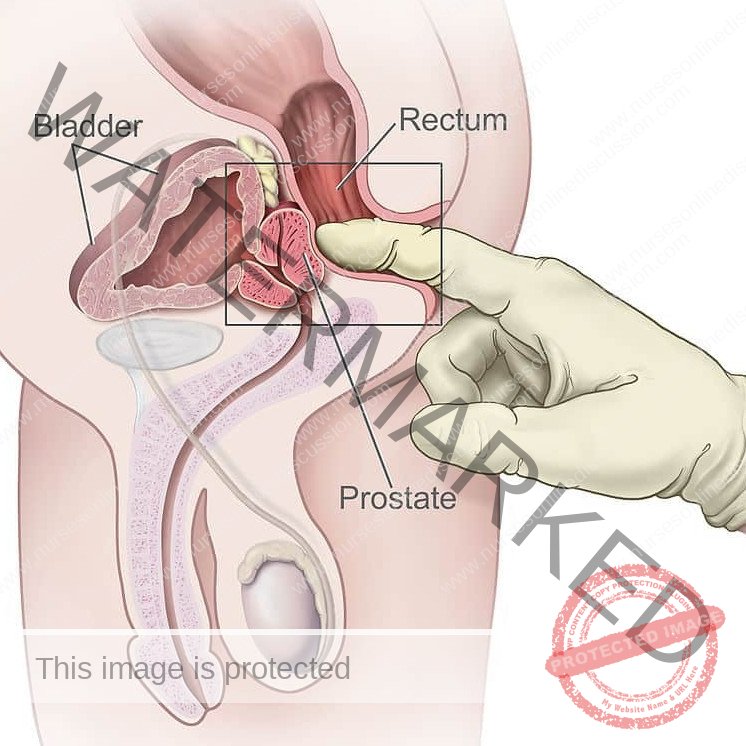
Prostate Gland
The prostate gland is situated in the pelvic region, positioned anterior to the rectum and posterior to the pubic symphysis. It completely encircles the urethra at the point where the urethra emerges from the urinary bladder.
It features an external fibrous capsule that encloses glandular tissue embedded within smooth muscle. In younger individuals, the gland typically weighs about 8 grams. However, it is prone to progressive enlargement (hypertrophy) as age advances, often reaching approximately 40 grams by age 50.
The prostate gland secretes a thin, milky fluid that is slightly acidic (with a pH of around 6.5). This prostatic fluid constitutes roughly 30% of the total semen volume and imparts to semen its characteristic milky appearance.
The prostatic secretion is rich in several proteolytic enzymes, including prostate-specific antigen (PSA), pepsinogen, lysozyme, amylase, and hyaluronidase. These enzymes play a role in ultimately breaking down the clotting proteins that originate from the seminal vesicles after ejaculation.
- A clotting enzyme present in the prostatic fluid contributes to the initial thickening of semen once it is deposited in the vagina. This thickening action is believed to enhance the retention of semen in close proximity to the cervix, thereby potentially improving the chances of fertilization.

Bulbourethral glands
Bulbourethral glands, also known as Cowper’s glands, are a pair of small glands, roughly the dimension of peas.
Positioned below the prostate gland, these glands reside on either side of the membranous urethra, embedded within the perineum’s deep muscles. Their excretory ducts empty into the spongy urethra.
Upon sexual stimulation, the bulbourethral glands release an alkaline secretion into the urethra. This fluid serves to protect sperm as they pass by counteracting any residual acidity from urine within the urethral passage.
Furthermore, they produce mucus, which acts as a lubricant for both the tip of the penis and the urethral lining. This lubrication helps to minimize sperm damage during the ejaculation process.
Penis
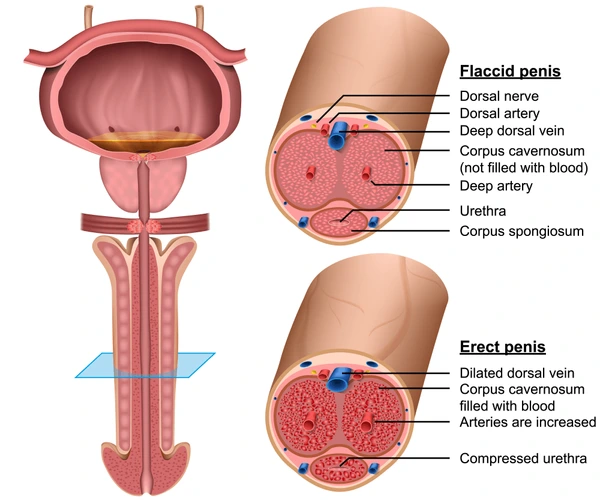
The penis houses the urethra and serves as a conduit for both the discharge of semen during ejaculation and the excretion of urine.
It possesses a cylindrical form, structurally divided into three parts: the body, the glans penis, and the root.
The main section, or body, of the penis comprises three cylindrical columns of tissue. Each of these masses is encased in a fibrous sheath known as the tunica albuginea.
The paired dorsal-lateral masses are termed the corpora cavernosa, while the singular, smaller mid-ventral mass is the corpus spongiosum. The corpus spongiosum encircles the spongy urethra and maintains its patency during ejaculation.
The entire penis is enveloped by skin and a subcutaneous layer. Beneath these outer layers lies erectile tissue, which is the primary component of these masses. Erectile tissue is characterized by numerous blood-filled spaces (vascular sinuses) lined with endothelial cells and supported by smooth muscle and elastic connective tissue.
The distal extremity of the corpus spongiosum expands slightly to form the glans penis. Within the glans penis, the distal urethra widens, culminating in a terminal slit-like opening, the external urethral orifice.
In an uncircumcised penis, the glans is covered by a retractable fold of skin called the prepuce, commonly known as the foreskin.
The base of the penis, referred to as the bulb, is anchored to the inferior aspect of the deep muscles of the perineum. It is surrounded by the bulbospongiosus muscle, a muscle that plays a role in assisting ejaculation.
The penis’s weight is supported by two ligaments that are continuous with the fascia of the penis. The fundiform ligament originates from the lower part of the linea alba, and the suspensory ligament of the penis arises from the pubic symphysis.
Sperm / Spermatozoa
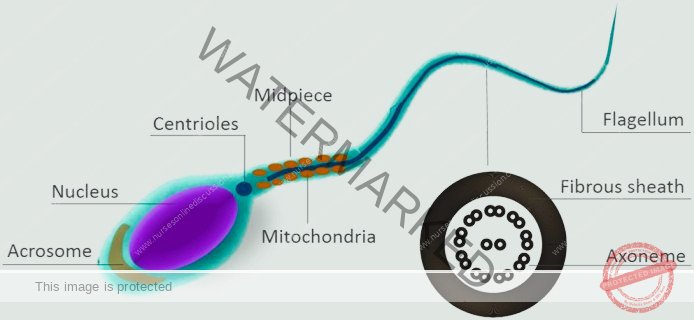
Every single day, the male body orchestrates the production of approximately 300 million sperm through a process termed spermatogenesis.
Spermatogenesis is the biological mechanism by which haploid (possessing a single set of chromosomes) spermatozoa are generated from germ cells situated within the seminiferous tubules of the testicles.
An individual sperm cell measures around 60 micrometers in length, with its primary components being the head and the tail.
The head, which is about 4-5 micrometers in dimension, houses a nucleus containing 23 densely packed chromosomes.
The acrosome, a cap-like structure enveloping the anterior two-thirds of the nucleus, is filled with enzymes. These enzymes, including hyaluronidase and proteases, are critical for facilitating penetration of the secondary oocyte during fertilization.
The tail is segmented into distinct regions: the neck, middle piece, principal piece, and end piece.
The neck region contains centrioles, while the middle piece is abundant in mitochondria, which are essential for energy (ATP) production. The principal and end pieces contribute to the overall length and motility of the tail.
Once ejaculation occurs, the majority of sperm cells have a limited lifespan, typically not surviving beyond 48 hours within the female reproductive system.
Semen
Semen is a complex fluid, a mixture of sperm and seminal fluid originating from the seminiferous tubules, seminal vesicles, prostate gland, and bulbourethral glands.
The typical volume of ejaculate in a single emission ranges from 2.5 to 5 milliliters, containing a sperm concentration of 50 to 150 million spermatozoa per milliliter.
Seminal fluid provides crucial support to sperm by offering transportation medium, essential nutrients, and protective elements.
Coagulation proteins derived from seminal vesicles initiate the coagulation of semen, causing it to thicken within approximately 5 minutes post-ejaculation.
Prostate-specific antigen (PSA) and other enzymes originating from the prostate subsequently induce semen re-liquefaction, typically occurring after 10 to 20 minutes.
The prostate gland contributes a fluid that constitutes roughly 30% of the total semen volume, significantly contributing to its characteristic milky appearance.
Hormonal functions in spermatogenesis are multifaceted, including FSH stimulation for sperm production, LH promotion of testosterone generation, and inhibin’s role in decreasing FSH secretion.
The initiation of spermatogenesis occurs at puberty, with millions of sperm being continuously produced daily under the influence of testosterone.
Erection is initiated by parasympathetic nerve fibers triggering the release of nitric oxide, which increases blood flow into erectile tissues.
Ejaculation is governed by a sympathetic nervous system reflex. It involves the release of semen from the urethra; pre-ejaculatory emission may occur, and muscular contractions play a vital role in the process.
Process of Erection
Erection is defined as the physiological process involving the enlargement and stiffening of the penis, enabling it for sexual intercourse.
Sexual stimulation – whether visual, tactile, auditory, olfactory, or even imagined – triggers parasympathetic nerve fibers originating from the sacral segment of the spinal cord. These nerve signals prompt the release of nitric oxide (NO).
Nitric Oxide (NO) acts as a vasodilator, causing relaxation of smooth muscle within the walls of arterioles supplying erectile tissue. This relaxation leads to dilation of these blood vessels.
This dilation significantly increases the volume of blood to enter the erectile tissue of the penis.
NO also promotes relaxation of the smooth muscle within the erectile tissue itself, resulting in the expansion and widening of the blood sinuses, thus contributing to the overall erection.
The engorgement and expansion of the blood sinuses exert pressure, effectively compressing the veins draining the penis, slowing down venous blood outflow and thereby helping to sustain the erection.
Process of Ejaculation:
Ejaculation is defined as the forceful expulsion of semen from the urethra to the external environment.
This process is a sympathetic reflex, coordinated by the lumbar region of the spinal cord. As part of this reflex action, the smooth muscle sphincter located at the base of the urinary bladder tightly closes. This critical action prevents the unwanted expulsion of urine during ejaculation and also ensures that semen does not mistakenly enter into the urinary bladder.
Prior to ejaculation, a sequence of peristaltic contractions occurs within the epididymis, ductus (vas) deferens, seminal vesicles, ejaculatory ducts, and prostate gland. These coordinated contractions work to propel semen into the penile portion of the urethra (specifically, the spongy urethra). This preparatory phase typically results in an emission, which is the discharge of a small volume of semen just before the main ejaculation. Emission can also occur involuntarily during sleep, known as nocturnal emission.
The muscles of the penis – including the bulbospongiosus, ischiocavernosus, and superficial transverse perineus muscles, all controlled by the pudendal nerve – contract rhythmically during ejaculation. These contractions contribute to the forceful expulsion of semen.
Following the cessation of sexual stimulation, the arterioles that supply blood to the erectile tissue of the penis constrict. Simultaneously, the smooth muscle within the erectile tissue itself contracts. These actions lead to a reduction in the size of the blood sinuses within the penis. This process effectively relieves pressure on the veins, allowing the accumulated blood to drain out, and causing the penis to revert to its flaccid (relaxed) state.
PUBERTY IN MALES
Puberty in males typically initiates between the ages of 10 and 14, characterized by a notable surge in luteinizing hormone released from the anterior pituitary gland.
This hormonal increase stimulates the interstitial cells within the testes, which in turn boosts testosterone production. The influence of testosterone then triggers a cascade of changes associated with sexual maturation, including:
Growth: Significant gains in height and weight occur, along with muscle mass and bone development.
Voice Changes: The larynx grows larger, causing the voice to deepen, a phenomenon often termed “voice breaking”.
Development of Body Hair: Hair becomes more visible across the body, notably on the face, in the underarm areas (axillae), chest, abdomen, and pubic area.
Genital and Prostate Growth: The penis, scrotum, and prostate gland experience growth and maturation.
Sperm Production: The seminiferous tubules within the testes mature, initiating the production of sperm cells (spermatozoa).
Skin Changes: The skin becomes thicker and produces more oil, potentially leading to acne.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

