Health Service Management
Subtopic:
Integrated Disease Surveillance And Response (IDSR)
IDSR
A strategy applied to manage multiple diseases or health conditions. It establishes connections between community, healthcare facilities, district, and national levels to ensure efficient resource use for disease management and prevention.
Integrated Disease Surveillance
A comprehensive strategy utilized by public health systems. It’s designed to observe, identify, and react to diverse diseases and health-related events in a synchronized manner.
Surveillance
Refers to the continuous and systematic process of collecting, analyzing, and interpreting health-related data. This includes the prompt sharing and application of information to guide public health actions.
Surveillance is also essential for planning, implementing, and assessing public health interventions at all levels.
Disease surveillance
Involves the continuous monitoring of diseases and factors influencing their patterns of occurrence and progression. This is crucial for enabling timely public health responses.
Disease Outbreak
Indicates a sudden upsurge in the number of cases of a particular disease within a specific geographical area and timeframe, exceeding the expected norm.
Communicable Diseases
Also known as infectious diseases. These are illnesses resulting from pathogenic microorganisms like bacteria, viruses, fungi, or parasites. They can be transmitted from person to person, either directly or indirectly.
Case Definition
A standardized set of criteria that clearly defines what constitutes a confirmed case of a specific disease. It is essential for healthcare professionals to accurately identify and categorize cases during disease surveillance activities.
Priority Diseases
Diseases that are given special attention due to their substantial impact on public health and their potential for rapid spread and serious consequences. The priority of diseases can differ based on geographical area and context.
Supervision, Monitoring, and Evaluation
These are crucial components of disease surveillance that encompass overseeing and assessing the surveillance system’s operations, tracking data quality and completeness, and evaluating the effectiveness of response approaches.
The outstanding bodies are:
Division of emergency infectious and surveillance services (DEISS): Provides specialized knowledge to design, develop, implement, monitor, and evaluate strategies for IDSR. They also facilitate the organization of tools for the program, such as laboratory equipment.
Division of epidemiology and surveillance capacity building: Offers expertise to strengthen surveillance capabilities by providing training to target countries.
Global Immunization Division (GID): Experts in vaccine-preventable disease surveillance and integrated data management are provided for an expanded program for immunization-related surveillance and routine immunization.
In 1996, a significant issue arose with Ebola. Consequently, Uganda chose to participate in the IDSR program. They tasked the CDC with investigating disease outbreaks. Other African nations, including Ethiopia, Ghana, and Burkina Faso, also utilize IDSR for managing outbreaks.
Objectives of Integrated Disease Surveillance and Response
To enhance national capacity for prompt detection, thorough recording, timely reporting, and the utilization of electronic tools, along with routine analysis and rapid feedback of IDSR priority diseases, events, and conditions at all levels.
To strengthen national and subnational laboratory capacity to confirm IDSR priority diseases, events, and conditions.
To improve capacity for public health emergency preparedness and response across all levels.
To strengthen the supervision, monitoring and evaluation system for IDSR.
To integrate multiple surveillance systems to optimize the use of tools, personnel and resources for greater efficiency.
Emphasize community participation in the detection, reporting, and response to public health events. This includes both case-based and event-based surveillance, along with risk communication in accordance with International Health Regulations (IHR).
According to WHO AFRO 1998, the objectives for IDSR include:
To strengthen district level surveillance.
To integrate the laboratory with laboratory reports.
To reduce duplication of reporting on the outbreak.
To share resources among disease control programs.
To translate surveillance and laboratory data into specific and timely public health actions.
Basic Ingredient for IDSR
IDSR has identified essential elements to achieve its objectives effectively. To ensure IDSR functions optimally, several key aspects are crucial:
Clear case definition and reporting mechanism.
Efficient communication system.
Basic but sound epidemiological framework.
Good laboratory report.
Good feedback and rapid response.
Nurses/Midwives attached to health centers to document the surveillance reports.
Core functions of IDSR
Step 1 – Case Identification and Documentation
Employ standard case definitions for healthcare settings (covering human, animal, and environmental health).
Utilize simplified case definitions at the community level.
Identify priority diseases, conditions, and events that could signal an emerging public health concern.
Step 2 – Reporting Suspected Cases to Higher Levels
Report suspected cases, conditions, or events to the designated higher authority for action.
Crucial if it involves an epidemic-prone disease, a potential Public Health Emergency of International Concern (PHEIC), or a disease targeted for elimination or eradication. Ensure immediate reporting to the next level.
Step 3 – Data Analysis and Interpretation
Compile surveillance data and analyze it to identify trends.
Compare current data with previous periods.
Interpret findings to inform public health actions at all levels. Analyze data based on person, place, and time.
Step 4 – Investigation and Laboratory Confirmation
Actively investigate suspected cases, outbreaks, or events.
Ensure cases, outbreaks or events are investigated and confirmed through laboratory testing when necessary.
Step 5 – Preparedness Planning
Ensure the availability of public health emergency preparedness and response plans.
Establish mechanisms for coordinated response measures.
Proactively prepare teams to respond quickly to outbreaks or public health events.
Set aside essential supplies and equipment readily available for immediate action.
Step 6 – Response Implementation
Upon confirmation of an outbreak, coordinate and mobilize resources (human, financial, etc.).
Implement the appropriate public health response actions.
Step 7 – Risk Communication
Implement real-time exchange of information, advice, and expert opinions.
Communicate between experts, community leaders, officials, and at-risk populations.
Encourage communication across all levels and sectors within communities.
Ensure communities provide data and report outbreaks, cases, and events.
Step 8 – Surveillance System Improvement
Monitor, evaluate, supervise and provide feedback to continuously improve the surveillance system.
Assess the effectiveness of surveillance and response systems, evaluating timeliness, data quality, information preparedness, and overall performance.
Provide feedback to reinforce health workers’ engagement in the surveillance system.
Take corrective actions to address problems and implement improvements.
Detecting and Planning for Disease Outbreak
Based on prior learning about Integrated Disease Surveillance and Response (IDSR), the central group responsible for disease control are professionals within the Center for Disease Control (CDC), often located within a hospital setting.
Key members of the team, including midwives in district outposts, are crucial for effective work. Clear case definitions are essential for accurate disease detection and detailed reporting to the CDC.
Building on earlier discussions about community health, health assessments are vital to pinpoint health issues and diagnose priority diseases within communities. Reaching a diagnosis for community health problems requires surveillance, which includes laboratory tests and actively searching for cases.
When addressing infectious diseases, established guidelines should be followed. Surveillance activities are conducted to gather information, analyze it, interpret findings, and create reports for the CDC to guide action.
To effectively carry out these activities, a well-organized team is essential. This team should typically include:
District Health Officer: A key leader overseeing health activities within the district.
Community Health Workers: Frontline workers who directly engage with communities to gather information.
Laboratory Technician: Responsible for handling laboratory tests and analysis, crucial for confirming diagnoses.
Subordinate Nurses: Provide essential support and assistance in carrying out various tasks.
Collaboration among team members and adherence to established guidelines, until the final report is written, ensures a coordinated effort. This is vital for timely and accurate responses to disease outbreaks and safeguarding public health.
Approaches to public health surveillance.
A. Passive Surveillance:
This surveillance method relies on health institutions regularly submitting reports. Data collection is routine, originating from health facilities and communities.
It is the most frequently used surveillance approach due to its straightforward implementation.
Passive surveillance encompasses the monitoring of diseases and other public health events through established reporting mechanisms.
Data management often utilizes systems such as the Health Management Information System (HMIS) for organized data collection and analysis.
B. Active Surveillance:
This approach involves a more proactive search for cases within communities and health facilities. Active case finding is achieved through:
Systematic review of patient records by healthcare providers at health facility levels to identify potential cases.
Implementing targeted screening programs for specific health conditions at strategic locations like points of entry (borders, airports) and within health facilities themselves.
Establishing and maintaining consistent communication with essential reporting individuals and institutions. This can involve various communication methods such as phone calls, electronic communications, or in-person visits to healthcare facilities and laboratories.
Intensified efforts to identify additional cases and their contacts, especially during disease outbreaks, to control spread.
Focused surveillance on diseases targeted for elimination or eradication, such as Polio (through Acute Flaccid Paralysis – AFP surveillance) and Guinea Worm disease, ensuring program goals are met.
C. Integrated Disease Surveillance:
This surveillance strategy is designed to collect health-related data for a wide range of diseases simultaneously, employing standardized tools and methodologies for consistent data collection.
It is often supported by systems like Early Warning Alert and Response (EWAR) systems to enhance rapid detection and response capabilities.
The primary objective is to establish robust systems for early warning and ensure prompt public health responses to identified threats.
Data collection and analysis within IDSR are central to its function, providing a comprehensive platform for surveillance activities.
The system primarily operates through two key information pathways:
Indicator Based Surveillance (IBS): Focuses on routine data collected through health systems.
Event-Based Surveillance (EBS): Concentrates on capturing and verifying information about unusual health events.
Indicator-based surveillance (IBS)
IBS is characterized by the ongoing and organized process of identifying, systematically collecting, continuously monitoring, thoroughly analyzing, and interpreting structured health data.
The data is structured and presented as indicators, which are typically derived from well-defined and predominantly health facility-based formal data sources, ensuring data reliability and consistency.
Common methods used within indicator-based surveillance include:
Facility-based surveillance, relying on data from health facilities.
Case-based surveillance, focusing on individual case data.
Sentinel site surveillance, using selected sites for intensive monitoring.
Syndromic surveillance, monitoring symptom patterns for early detection.
Laboratory-based surveillance, utilizing laboratory confirmed data.
Disease-specific surveillance, targeting particular diseases of interest.
Community-based surveillance, incorporating data from community level.
Event-based surveillance (EBS)
EBS is specifically focused on the rapid detection and capture of information related to health events that have the potential to pose a risk to public health, ensuring timely awareness of potential threats.
Initial information capture for EBS can originate from diverse sources, including informal channels like rumors or preliminary signals indicating a potential event. These initial signals require formal verification to assess their validity.
While not every initial alert will necessarily represent a genuine public health event, each one is systematically assessed and verified to determine its significance and the necessity for a public health response.
Detecting and Planning for Disease Outbreak
Building upon the principles of Integrated Disease Surveillance and Response (IDSR), the primary unit responsible for managing diseases is the team at the Center for Disease Control (CDC), typically based in a hospital setting.
Effective teamwork, incorporating diverse roles like midwives positioned across districts, is crucial for successful operations. Utilizing clear and consistent case definitions is essential for precise disease identification and comprehensive reporting to the CDC.
Drawing from previous discussions on community health, conducting health assessments is fundamental to pinpointing health concerns and diagnosing significant diseases within communities. To accurately diagnose community health issues, implementing surveillance measures is necessary. This includes employing laboratory analyses and proactively searching for cases.
In managing infectious diseases, adhering to established protocols is vital. The process involves selecting and executing surveillance activities to gather relevant data, followed by analysis, interpretation of findings, and preparing reports for the CDC to guide subsequent actions.
For effective execution of these activities, a structured team is required, typically composed of:
District Health Officer: A key leader responsible for overseeing all health-related activities within the district.
Community Health Workers: Frontline personnel who directly interact with communities to collect information and engage in health monitoring.
Laboratory Technician: Specialized personnel who perform laboratory tests and analyses, which are critical for confirming diagnoses.
Subordinate Nurses: Essential support staff who assist in various tasks, providing necessary aid in operations.
Collaboration within this team, along with consistent adherence to established guidelines throughout the process, culminating in report generation, ensures a synchronized approach. This coordinated effort is vital for delivering prompt and accurate responses to disease outbreaks and ultimately protecting public health.
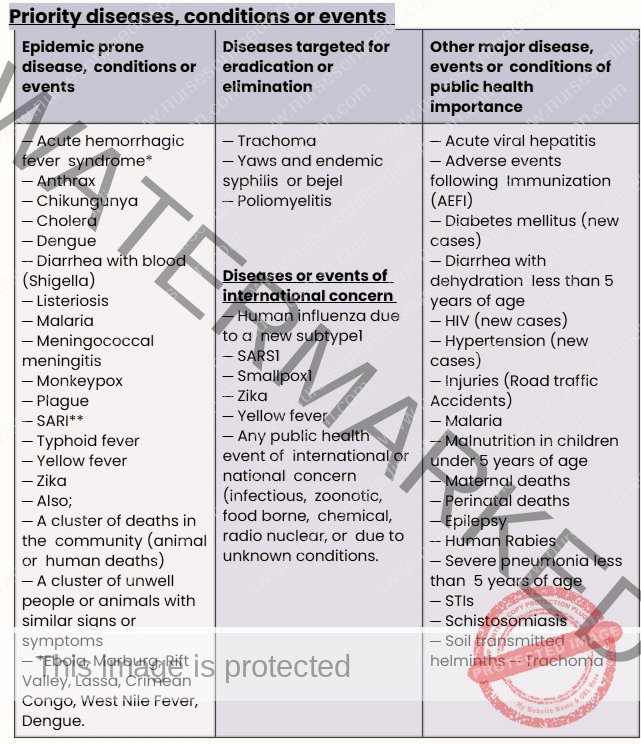
DETECTING AND REPORTING OF PRIORITY DISEASES, CONDITIONS/EVENTS
A vital function of a public health surveillance system is its capacity to identify significant diseases that fall under the responsibility of public health authorities at all levels. Prompt detection, reporting, and response to priority public health events are crucial for reducing the impact of illness and death.
Detection of suspected cases of outbreak-prone diseases should always be prioritized in health facilities and communities for the following:
Targeted Outbreak Prone Diseases, Conditions, and Events: Be vigilant for specific diseases known to cause outbreaks, as well as unusual health conditions and events.
Conditions Reported More Frequently Than Expected: Monitor for health conditions that are reported at a higher rate than typically observed within a community.
Clusters of Diseases: Investigate any groupings of similar illnesses or sudden deaths occurring after public gatherings or within specific locations.
Unusual Events with Health Risks: Be alert for any uncommon incidents that could potentially pose health risks to the population.
In Community:
Community Case Definition Importance: Community-level case definitions for priority diseases are essential. They play a significant role in surveillance by enabling early detection and prompt action for priority diseases, conditions, and events.
Community Participation: Community members should be educated and guided on surveillance practices. This empowers them to actively participate in detecting, reporting, and responding to health events related to humans or animals within their local areas.
Encourage Vigilance and Reporting: It is important to foster a culture of vigilance within communities. Encourage prompt reporting of identified events to facilitate timely and rapid responses.
Ways of detecting priority diseases, conditions and events.
Individuals Seeking Care: When a person becomes unwell and seeks medical attention at a healthcare facility.
Increased Hospital Admissions: An elevated number of hospital admissions for the same illness or related symptoms.
Community Reports: Information from community members regarding unusual events or disease patterns at the local level, such as clusters of deaths or unusual disease presentations in the community, health facility or school settings.
Healthcare Worker Observations: Health personnel conducting routine record reviews identify cases of illnesses that are not among the usual diseases reported or for priority diseases that have not been previously reported (e.g., AFP, cholera, measles).
Laboratory Register Review: Regular examination of laboratory registers reveals consistently recorded cases of priority diseases, for example, yellow fever or cholera.
Media Reports: Radio, television, newspapers, or social media outlets report potential rumors or unexplained health events in areas with potential exposure risks for humans.
Vital Records Analysis: Reviewing vital records to show an increase in maternal deaths, potentially signaling underlying health issues.
Reports of Illness in Healthcare Workers: Unusual reports of illness among healthcare staff, indicating potential workplace hazards or outbreaks.
Animal Health Events: An unusual death or a higher than normal number of deaths in animal populations, such as livestock, birds, or rodents, or an unusually high number of sick animals presenting with similar symptoms.
Environmental Hazard Observation: Environmental health officers, during assessments of water sources or bodies of water, observe potential contamination that might be attributable to chemicals like lead or other related chemicals originating from mining or industrial activities.
A STANDARD CASE DEFINITION
A case definition is a pre-established set of criteria that is agreed upon and used to determine if an individual has a suspected disease or health condition. The case definition typically specifies:
Clinical criteria (signs and symptoms)
Laboratory diagnostic criteria
Specific parameters related to time, location, and person
A case definition of a disease is a standardized set of criteria. It clearly outlines the specific characteristics, symptoms, and diagnostic findings that an individual must exhibit to be classified as having a particular disease for surveillance purposes.
It serves as a clear guiding tool for healthcare professionals and public health authorities. This ensures consistency and accuracy when identifying and categorizing cases of the disease for surveillance and response.
In simpler terms, a case definition acts as a checklist. This checklist assists healthcare workers in determining if a person’s symptoms and characteristics align with those of a specific disease. If the specified criteria in the checklist are met, then the individual can be considered a “case” of that disease for public health monitoring and response. This standardization is crucial for accurate disease tracking, monitoring trends, and implementing effective public health response measures.

Why do we need case definitions?
To aid in determining if an individual has a suspected disease or health condition, or to rule out other possible diagnoses.
To guarantee consistent diagnosis of every case, irrespective of location, time of occurrence, or the person who identified it.
To enable swift reporting and investigation, especially when clinical diagnosis takes longer to confirm.
To facilitate comparison of the number of cases of diseases, conditions, or events occurring at different times or locations.
Standard Case Definitions, for health facility level.
A three-level classification system is typically used: Suspect, Probable, and Confirmed.
Suspected case: Suggestive clinical presentation where a patient displays some clinical indicators, but lacks enough typical or definitive clinical features for a confirmed or probable diagnosis.
Probable case: Evident clinical presentation aligning with the clinical case definition. The patient exhibits typical clinical signs of the illness or has epidemiological links to a confirmed case, but laboratory confirmation is not possible. This might be because a sample was not obtained due to loss or death, or a sample was taken but was either insufficient for laboratory testing or not suitable for the required laboratory testing.
Confirmed case: A suspected or probable case that has been verified through laboratory analysis.
Priority Diseases in Uganda and their Case Definition
Activity:
Identify the most common priority diseases you have managed.
Measles
Tuberculosis
Poliomyelitis
Tetanus
Cholera
Hepatitis B
Outline the case definitions for these diseases.
Measles: Characterized by a fever accompanied by a rash, cough, and red, watery eyes.
Tuberculosis: Defined by a persistent cough lasting over two weeks, along with chest pain, and unintentional weight loss.
Poliomyelitis: Presents with muscle weakness or paralysis, frequently affecting the legs.
Tetanus: Marked by muscle stiffness and spasms, often commencing in the jaw muscles.
Cholera: Indicated by profuse watery diarrhea and vomiting, which can rapidly lead to dehydration.
Hepatitis B: Identified by jaundice, fatigue, abdominal discomfort, and dark-colored urine.
As a reminder, priority diseases are communicable diseases caused by biological agents or their products; they spread from person to person and are designated as priority due to their significant impact on human populations. Many of these diseases can result in widespread illness and mortality, and have substantial economic consequences for a country.
Uganda has experienced several outbreaks of diseases leading to fatalities. Some of these diseases include:
Measles: Commonly affects children aged 1 to 3 years, with key symptoms being rash, cough, and red, watery eyes.
Tuberculosis: Impacts individuals of all age groups, and is distinguished by a persistent cough, chest pain, and weight loss.
Poliomyelitis: Recent research highlights an increasing trend in this disease, causing muscle weakness or paralysis, often in the legs.
Tetanus: Affects people of all ages, typically starting with stiffness and spasms in the jaw muscles.
Cholera: Prevalent during rainy seasons and can become disastrous, with symptoms including severe watery diarrhea and vomiting, leading to dehydration.
Hepatitis B: Widespread throughout the country, with symptoms such as jaundice, fatigue, abdominal pain, and dark urine.
REPORTING SUSPECTED CASES OF PRIORITY DISEASE/EVENTS.
Rationale for Reporting Includes:
To detect emerging health problems or conditions and to devise appropriate responses, which includes informing relevant personnel at various levels.
To enable timely action to be taken promptly.
To track disease patterns and trends within the area.
To assess the effectiveness of implemented response measures.
In IDSR, data collection and reporting adhere to different timelines for different purposes:
i. Immediate reportable diseases, conditions and events:
Report case-based information to the next administrative level without delay.
Notify potential public health emergencies of international concern as per IHR 2005 guidelines.
Report significant events originating from community sources.
ii. Summarize Immediate and Weekly reportable diseases.
Weekly reporting of immediate notifiable diseases.
Zero reporting (even if no cases are observed, a report confirming this is necessary).
iii. Monthly /quarterly reporting.
Monthly and quarterly routine summary reports for other diseases of public health significance.
iv. Improve routine reporting practices
Assess the flow of information at each reporting level to identify bottlenecks or areas for improvement.
Maintain organized records and clear procedures for managing reporting forms to ensure efficiency.
Conduct regular periodic checks on data quality to identify and correct any inaccuracies.
Strengthen connections to enhance community-based surveillance, improving data flow and community involvement.
Enhance links between laboratory services and surveillance systems for better diagnostic data integration and information sharing.
Promote a multisectoral “One Health” approach that effectively incorporates involvement from human, animal, and environmental health sectors, alongside other relevant sectors, to strengthen overall reporting and data quality.
v. Data protection and security to protect patient’s confidentiality and privacy by using unique numbers instead of names and this will prevent identities
Record essential details of the sick person, which include:
The given name of the sick individual.
Sex, age bracket, and occupation of the person affected.
Residential address and precise location of the household.
The identified disease or condition.
The date when the symptoms first appeared.
Number of individuals affected within the same household.
Actions or interventions that were implemented.
Details of any prior contacts that are relevant.
Report promptly to local community leaders, the nearest healthcare facility in the vicinity, the health sub-district, District Health Officer (DHO), or surveillance team, and the Ministry of Health (MOH) using various communication methods like phone calls, SMS messaging, Android applications, and web-based platforms.
Create a line list that systematically records all cases observed within the health facility for detailed tracking and analysis.
ANALYZING/INTERPRETATION OF DATA IN PRIORITY DISEASES
Data is a collection of values pertaining to subjects, which can be classified as either qualitative or quantitative variables. OR Data refers to information converted into a format that is easily moved or processed effectively.
Analysis is the process of dissecting a whole entity into its individual components for detailed scrutiny of raw data. This process converts raw data into actionable information that is useful for decision-making purposes by users.
Data analysis involves a systematic approach of inspecting, cleansing, transforming, and modeling data. This comprehensive process aims to uncover valuable insights, inform conclusions, and provide solid support for decision-making processes.
Analyzing data provides essential information that is utilized to take relevant, timely, and appropriate public health interventions.
Analyzing surveillance data allows for:
Observing patterns and trends in health events over time, enabling health staff to be alerted about emerging issues or unusual disease patterns.
Identifying specific geographic locations that are at a higher risk for certain diseases or health conditions.
Characterizing personal attributes, such as age groups, gender, or occupation, that may indicate a person is at greater risk of contracting a disease or experiencing a health-related event.
Monitoring and evaluating the effectiveness and impact of public health interventions that have been implemented.
1. RECEIVE, HANDLE AND STORE DATA FROM REPORTING SITES
a) Receive Data
Ensure a meticulous record of all data received from each reporting site is maintained for accountability and tracking.
Confirm that the surveillance team at each level or reporting site where data originates effectively receives the data.
Acknowledge receipt of each data report from the reporting source to confirm successful transmission.
Systematically log each received data set or surveillance report into a suitable logbook or electronic system dedicated for each reporting site.
Document in a log the specifics of the data received, including the time and date of receipt, the content of the report, and the identity of the sender for traceability.
Verify if the data reports were submitted in a timely manner or if there were any delays in reporting schedules.
Check the completeness of each data set or report to ensure all required information is included.
Review the overall quantity of data received to assess coverage and reporting rates from different sites.
Verify that the information, whether in hard copy or electronic format, is filled out accurately and without errors.
Ensure that all sections of the reporting form are fully completed to avoid missing data points.
Check to confirm that there are no inconsistencies or discrepancies within the data presented on the forms.
Consolidate or merge the received data and then securely store it in a database system for organized access and analysis.
For guidance on electronic surveillance practices, refer to the eIDSR (electronic Integrated Disease Surveillance and Response) guide for detailed protocols.
b) Enter and clear the data
Extract data pertaining to priority IDSR diseases directly from the register and accurately input it into aggregated IDSR reporting forms. While doing so, compile data from all reporting sites by effectively liaising with health information assistants (HIAs).
Ensure that all health facility personnel are well-informed about the correct algorithm for reporting and understand the required reporting levels within the system.
Use the following practices regardless of the method

Analyze data by time
Analyze data by place
Analyze data by person
Construct a table for person analysis
Calculate the percentage of cases within specific age groups
Calculate attack rates
Calculate case fatality rate
3. Compare Analysis Results with Thresholds for Public Health Action
Alert Threshold: This is the crucial number of cases (or any relevant indicator such as proportion, or rate) that signals the need to initiate an investigation at the onset of a potential epidemic and to prepare for an appropriate response.
Action (Epidemic) Threshold: This represents the essential number or concentration of susceptible individuals needed for an epidemic to occur, triggering a determined public health action.
4. Draw Conclusions from the Findings to Generate Information Through:
Regularly compile and present data using graphs, maps, and tables. Engage in meetings with district health teams or relevant stakeholders to carefully review analysis results and thoroughly discuss the findings.
Systematically examine the findings in accordance with the district’s analysis plan, if such a plan exists and has been prepared.
Ensure to integrate your analysis with other relevant data sources, such as information from animal health or environmental monitoring, to support a more accurate and comprehensive interpretation of the findings.
Evaluate the quality and reliability of the data when interpreting the results to ensure accuracy and validity of conclusions.
At a minimum, review the findings to:
Assess the current situation based on the data.
Compare current data with previous trends and expected patterns.
Consider possible explanations for any observed increase in cases or unusual trends.
Analyze potential changes in reporting of cases that may affect data interpretation.
Examine any changes in reporting procedures that could influence the data.
Review any changes in case definitions being used for reporting to ensure consistency and accuracy.
Summarize the analysis and effectively use it to improve public health action strategies and interventions.
Prepare a comprehensive report and share the findings and recommendations with all relevant stakeholders, including the affected communities, to ensure transparency and collaborative action.
INVESTIGATION AND CONFIRMATION OF SUSPECTED CASES, OUTBREAKS/EVENTS:
Purposes:
Verify the existence of an outbreak or confirm a significant public health event and assess the immediate risk to the population.
Identify and ensure treatment for additional cases that might not have been previously reported or recognized through routine surveillance.
Collect essential information and laboratory specimens to definitively confirm the diagnosis. Accurately identify the source of infection or the underlying cause of the outbreak to implement targeted interventions.
Aid in thoroughly describing the epidemiological situation in terms of time, geographic place, and affected person characteristics to understand the scope and dynamics of the event.
Explain the modes of disease transmission and identify the population groups at higher risk of infection. Select and implement appropriate response activities aimed at controlling the current outbreak or managing the public health event effectively.
Strengthen existing prevention activities to effectively avoid future reoccurrence of similar outbreaks and enhance long-term public health security.
Steps of outbreak investigation
Prepare to conduct an investigation: Mobilize Public health emergency rapid response team (PHERRT)
Clearly define specific tasks for each member of the PHERRT, outlining their expected contributions.
Establish clear lines of supervision and communication pathways within the team and with external entities.
Determine the geographical scope and specific locations where the investigation will be concentrated.
Secure all necessary official authorizations and permissions to conduct the investigation effectively.
Finalize and prepare standardized forms and methodologies for consistent and comprehensive data collection and specimen handling.
Organize transportation arrangements and other logistical needs to ensure team mobility and operational efficiency.
Assemble and pack all essential supplies required for collecting laboratory specimens and conducting field investigations.
Verify and confirm the outbreak/event
Review patient clinical histories and relevant epidemiological data to understand the event’s nature.
Collect appropriate laboratory specimens for diagnostic confirmation and pathogen identification.
Obtain laboratory results to definitively confirm the diagnosis and characterize the causative agent.
Define and search for additional cases
Develop a clear and operational case definition to ensure consistent case identification.
Isolate and provide appropriate treatment to confirmed cases to prevent further transmission and manage illness.
Actively search for additional cases by reviewing health facility records and investigating reported cases and deaths.
Extend case finding to the community, actively searching for suspected cases and deaths, including contact tracing to identify chains of transmission.
Develop a line list and record information about the additional cases
Create a detailed line list to systematically record and track key information for each identified case.
Analyze data about the outbreak; Interpret analysis results
Interpret the time analysis results to understand the temporal pattern of the outbreak.
Interpret the person analysis results to identify high-risk populations and demographic factors.
Interpret the place analysis results to determine geographical distribution and potential environmental links.
Analyze collected data to formulate preliminary hypotheses about the outbreak’s origins and transmission.
Test and refine the initial hypotheses through further analytic studies and data review.
Report writing and dissemination of findings.
Prepare a comprehensive report documenting the investigation process, findings, and recommendations.
Disseminate the report to relevant stakeholders and public health authorities for informed decision-making and action.
Implement prevention and control measures.
Put into action targeted prevention and control strategies based on the investigation’s findings to contain and mitigate the outbreak.
Conduct an assessment to determine if the event is a potential public health emergency of international concern (PHEIC).
Evaluate the severity, scale, and potential international implications of the event to determine if it meets PHEIC criteria.
Maintain and intensify surveillance.
Continue and enhance surveillance activities to monitor the outbreak’s progression and detect any resurgence or new cases.
Conducting regular risk assessment after the outbreak has been confirmed.
Regularly perform risk assessments to adapt response strategies, evaluate ongoing risks, and plan for post-outbreak management and prevention.
RESPONDING TO OUTBREAKS AND OTHER PUBLIC HEALTH EVENTS
Preparation: Preparations for public health events involve the following;
Establish a permanent PHEOC (command and control Centre) for overseeing public health emergency preparedness and response activities.
The Public Health Emergency Operations Center (PHEOC) must develop essential elements to be fully functional to support preparation and response to emergencies.
Develop detailed plans and standard operating procedures for all critical operations within the PHEOC.
Implement robust telecommunication technology and infrastructure to ensure timely and reliable communication.
Establish an information management system to support data-driven and informed decision-making processes (e.g., using HMIS/DHIS2 platforms).
Ensure the availability of trained human resources capable of effectively staffing and managing the PHEOC during emergencies.
Establish a district or regional public health emergency management committee (PHEMC)
Form a Public Health Emergency Management Committee (PHEMC) at the district or regional level.
Clearly identify and appoint members of the PHEMC, defining roles and responsibilities.
Define the specific functions and operational procedures of the PHEMC in emergency response.
Schedule and conduct regular PHEMC meetings to ensure preparedness and coordination.
Establish public health emergency management committee at all level
Ensure a Public Health Emergency Management Committee is established and functional at every relevant administrative level to facilitate coordinated response.
These includes;
Coordination/management subcommittees.
Roles: Coordinate all aspects of the operations response, planning and management including;
Selecting participating organizations and clearly assigning specific responsibilities to each partner involved in the response.
Designing, implementing, and rigorously evaluating control interventions to ensure effectiveness and adapt strategies as needed in collaboration with partners.
Facilitating coordination of technical Emergency Preparedness and Response (EPR) subcommittees and ensuring overall liaison with all involved partners.
Ensuring daily communication and information sharing through situation reports that provide updates on the evolution and current status of the outbreak.
Managing information dissemination to the public and news media to keep the community informed and manage public perception.
Providing operational support, encompassing mobilization of resources, logistics, and administrative support necessary for field operations.
Being responsible for staff wellbeing and security, ensuring the safety and support of all personnel involved in the response efforts.
Finance and administration.
Track expenditure meticulously, manage payments efficiently, and provide essential administrative services to support financial operations.
Ensure appropriate cash flow management, including tracking material and human resources, carefully looking at costs, budget preparation, monitoring, and maintenance of all administrative records related to finances.
Logistics committee.
Provide budgetary support and secure funding specifically for epidemic preparedness and response activities.
Manage the procurement process for all necessary equipment and supplies required for outbreak response.
Maintain adequate stocks of essential supplies and equipment, ensuring readiness for rapid deployment in emergencies.
Arrange for transport and establish reliable communication systems to support logistical operations.
Liaise with other agencies and partners for logistical support, ensuring seamless resource mobilization and delivery.
Provide accountability for all resources utilized during epidemic preparedness and response activities, ensuring transparent and responsible resource management.
Planning committee.
Evaluate the overall situation through comprehensive information gathering and analysis to understand the evolving context of the emergency.
Conduct thorough assessment of the various options for dealing with the situation, including resource implications and feasibility.
Keep meticulous track of all resources utilized and needed throughout the response to inform planning and resource allocation.
Case management and infection prevention and control committee
Ensure the development and availability of clear guidelines and Standard Operating Procedures (SOPs) for effective case management and rigorous infection prevention and control protocols across all healthcare facilities.
Enhance the capacity of isolation facilities to appropriately manage cases and implement robust infection prevention and control measures to minimize transmission.
Conduct thorough risk assessments specifically targeting healthcare workers to identify and mitigate occupational hazards.
Confirm that appropriate and high-quality medical care is consistently provided to all patients, adhering to established clinical protocols.
Organize and offer ambulance services to facilitate the safe and efficient collection and transportation of suspected cases from the community, strictly following the defined referral system.
Systematically collect data from all treatment facilities involved in the response (if applicable) and promptly submit this data to the surveillance subcommittee for comprehensive oversight.
Ensure proper and thorough disinfection of homes and environments where suspected, probable, or confirmed cases, as well as deaths from infectious diseases, have occurred to minimize environmental contamination.
Conduct safe and dignified burial of deceased individuals from isolation facilities and communities, adhering to cultural sensitivities and public health guidelines to prevent further spread.
Organize and implement training and refresher training programs for healthcare workers specifically in isolation facilities and other health facilities within the affected district to maintain high standards of care and safety.
Surveillance and laboratory
Ensure that all relevant surveillance guidelines and tools are readily available and effectively utilized in all health facilities to standardize surveillance practices.
Enforce the consistent application of the outbreak case definition to ensure uniform case identification and reporting.
Conduct active case finding initiatives, thorough case investigations, and rigorous contact tracing and follow-up activities to identify and manage all potential cases.
Implement verification processes for suspected cases, alerts, and rumors circulating within communities to promptly assess and respond to potential threats.
Ensure the proper and systematic filing of case investigation forms, contact tracing records, and follow-up documentation for efficient data management and future reference.
Implement protocols for proper collection, secure packaging, safe transportation, and accurate testing of specimens obtained from suspect, probable cases, and deceased individuals to ensure reliable laboratory diagnoses.
Communicate laboratory test results promptly and effectively to clinical services to facilitate timely patient management and public health actions.
Conduct comprehensive data management activities and provide regular epidemiological analysis and reports to inform decision-making and track outbreak dynamics.
Organize specialized training for health personnel in advanced disease surveillance techniques to enhance workforce capacity and surveillance quality.
Establish and maintain close collaboration with burial teams, infection control specialists, and social mobilization groups to ensure a coordinated and comprehensive response effort.
Risk communication and social mobilization
Ensure the development and distribution of accessible risk communication materials and plans to effectively inform the public about the health risks and preventive measures.
Conduct rapid assessments to understand community knowledge, attitudes, practices, and behaviors regarding prevailing public health risks and events to tailor communication strategies.
Organize comprehensive sensitization and mobilization campaigns targeting communities to promote awareness, understanding, and engagement in prevention efforts.
Serve as the primary point of contact for information to be released to the press and broader public, ensuring consistent and accurate messaging.
Liaise closely with different subcommittees, local leadership, and Non-Governmental Organizations (NGOs) involved in activities aimed at mobilizing communities to maximize reach and impact.
Psychosocial support committee
Provide essential psychological and social support services to suspected, probable, and confirmed cases, as well as affected families and communities to address mental health and social well-being needs.
Provide wellness care and psychological support specifically to the response team members to manage stress and ensure their mental health during demanding operations.
Prepare bereaved families and communities for culturally sensitive and dignified burials, offering support during grief and bereavement.
Prepare communities for the reintegration of convalescent cases and patients who have fully recovered, promoting social inclusion and reducing stigma.
Water sanitation and hygiene- WASH committee
Conduct detailed environmental health risk assessments specifically focused on the outbreak context to identify and mitigate environmental transmission pathways.
Ensure consistent provision of clean and safe water to affected communities and healthcare facilities to prevent waterborne transmission and support basic hygiene.
Implement improved water management strategies at both household and community levels to optimize water usage and minimize contamination risks.
Plan and execute comprehensive sanitation improvement campaigns to enhance environmental sanitation and reduce disease vectors.
Plan and promote improved hygiene practices, emphasizing hand-washing, food hygiene, and overall sanitation practices within communities to promote behavioral change and prevent transmission.
Vaccination campaign committee/EPI team
Identify specific high-risk groups within the population during the outbreak who should be prioritized and targeted for vaccination to maximize impact and protection.
Accurately compute the targeted population size to ensure sufficient vaccine supply and logistical planning for the vaccination campaign.
Conduct meticulous micro-planning for all aspects of vaccination logistics, including cold chain management, vaccine delivery and distribution, human resource allocation, community mobilization needs, and waste handling procedures for a smooth and efficient campaign.
Conduct the vaccination campaign in accordance with established protocols and implement post-vaccination campaign validation exercises to assess coverage and effectiveness.
Establish public health emergency rapid response team (PHERRT) Roles of PHERRT includes;
Investigate rumors and formally reported outbreaks, rigorously verify diagnoses, and thoroughly assess other public health emergencies, including conducting laboratory testing to confirm etiologies.
Collect additional samples from new patients and, when necessary, from old cases to gain comprehensive epidemiological and diagnostic information (samples can include human, animal, food, and water sources depending on the nature of the event).
Conduct thorough follow-up activities by visiting and interviewing exposed individuals and affected communities to gather detailed histories, establish a robust case definition, and work collaboratively with the community to identify additional cases.
Assist in establishing and implementing effective mechanisms for the implementation of Infection Preventive Control Measures in healthcare and community settings to minimize transmission.
Assist in generating a comprehensive line list of cases, and perform descriptive epidemiological analysis of data (Person, Place and Time) to generate initial hypotheses about the outbreak’s dynamics, which is crucial for planning for further analytical studies.
Propose appropriate and evidence-based strategies and control measures, including risk communications activities, tailored to the specific context and needs of the outbreak.
Establish an appropriate and coordinated risk communication system, ensuring consistent messaging and utilizing a trained spokesperson to effectively communicate with the public and media.
Coordinate rapid response actions, working in close collaboration with national and local authorities, international partners, and other relevant agencies to ensure a unified and effective response.
Initiate the swift implementation of the proposed control measures, including capacity building activities to strengthen local response capabilities and ensure sustainability.
Conduct ongoing monitoring and rigorous evaluation of the effectiveness of implemented control measures through continuous epidemiological analysis of the control efforts and adapting strategies as needed.
Conduct Risk Assessments to rigorously determine if the outbreak qualifies as a potential Public Health Emergency of International Concern (PHEIC), based on established criteria.
Prepare detailed investigation reports that are comprehensive and structured to effectively share findings and recommendations with the PHEMC for informed decision-making.
Contribute actively to ongoing preparedness assessments and the final evaluation of each outbreak response to identify lessons learned and areas for improvement.
Schedule and conduct daily meetings during active outbreaks to ensure real-time coordination and information sharing, and meet quarterly during periods without outbreaks to maintain preparedness and review protocols.
Participate regularly in simulation exercises to test preparedness plans, enhance team coordination, and identify gaps in response capabilities.
4. Risk mapping for outbreaks and other public health events.
Risk assessment and mapping techniques should be used as a valuable tool to enhance preparedness. This approach helps to pinpoint at-risk geographical areas or specific populations, prioritize preparedness activities based on risk levels, and effectively engage key policy makers and operational partners in targeted interventions.
5. Resource mapping to identify the available resources in every geographical area to ensure prompt mobilization and distribution of such resources including materials, human and funds in an outbreak situation
6. Prepare an emergency preparedness and response plan to strengthen the ability of the national to subnational levels to respond promptly when an outbreak/event is detected. This plan should; Response to outbreaks/events
Declaring an outbreak and activating the response structures: Once an epidemic threshold is reached at the district level, the head of DHMT should promptly notify the region and the Ministry of Health (MOH). MOH will then assess whether the event constitutes a potential Public Health Event of International Concern.
Mobilize PHERRT for immediate action which includes: Convene the district public health management team for outbreak/event. Once confirmed, DHMT will collaborate with the district authority to convene PHEMC to assess and implement the response strategy.
Select and implement appropriate public health response activities. These includes;
Strengthen case management and infection prevent and control measures (IPC).
Build the capacity for response staff through targeted training and support.
Enhance surveillance activities during the response to track the outbreak’s progression.
Enhance surveillance collaboration with neighboring border districts to prevent cross-border spread.
Engage community participation actively during the response to ensure community ownership and support.
Inform and educate the community comprehensively about the outbreak, risks, and preventive measures.
Conduct a mass vaccination campaign if indicated and deemed necessary by public health assessment.
Improve access to clean and safe water to ensure basic sanitation and hygiene.
Ensure safe disposal of infectious waste to prevent environmental contamination and further transmission.
Improve food handling practices to minimize foodborne transmission risks.
Reduce exposure to infectious or environmental hazards through targeted interventions and public health advisories.
Ensure safe and dignified burial and handling of deceased bodies in accordance with cultural norms and public health guidelines.
Ensure appropriate and adequate logistics and supplies are in place to support all response activities effectively.
7. Provide regular situation reports on the outbreak and events
8. Document the response including minutes of meeting, activity, process, epidemic report, evaluation reports and other relevant document
9. Treatment of cases during an outbreak with appropriate medicine and procedures. These may include;
Antibiotics, when applicable for bacterial infections.
Rehydration with fluids administered orally or intravenously to manage dehydration.
Assessment of pain and implementation of pain management strategies to alleviate suffering.
Ensure appropriate infection control measures are strictly followed to prevent secondary infections and nosocomial transmission.
Observation of vital signs and specific clinical observations to monitor patient condition and treatment response.
Other routine nursing care as needed to support patient recovery and comfort.
The Different Levels Where Surveillance Activities Are Performed
Community: Surveillance at the community level is typically performed by basic community-level service providers. These include Village Health Teams (VHTs), village leaders (religious, political, traditional), school teachers, agricultural extension workers, veterinarians, chemical and drug sellers, and traditional healers who are often the first point of contact in healthcare seeking.
Health facility: For the purpose of surveillance, all health institutions (public and private health service providers) that offer outpatient care and/or in-patient facilities are defined as a “health facility” and are crucial for case detection and reporting.
Health Sub-district (HSD): The HSD is recognized as the basic level for the effective delivery of the Uganda National Minimum Health Care Package. It is mandated with comprehensive planning, organization, budgeting, supervision, and overall management of health services at both this level and lower-level health centers. The HSD carries an essential oversight function of health care services within its jurisdiction, often with a referral facility at the level of a general hospital or Health Centre (HC) IV. For surveillance purposes, the HSD receives, consolidates, and reviews reports from all lower-level health facilities within its catchment area and submits aggregated reports to the district level.
District: The District health services have the primary responsibility of planning and directing the implementation, supervision, and continuous monitoring of integrated health service delivery, particularly in the context of the “One Health” approach.
Regional Level: This level consists of regional referral hospitals (RRH), which are designed to provide specialized referral services, offer support supervision to lower districts, and coordinate response to public health threats to the districts within their respective regions.
National level: The national health system, at the apex, consists of the Ministry of Health and other national-level institutions. These encompass national referral hospitals, national reference laboratories, and national medical stores. It is at this level that national health policies, guidelines, and standard operating procedures are developed and resources are allocated. In relation to surveillance, this level reports on priority diseases and actively uses the IHR decision instrument for international health security.
Roles and Responsibilities of Various Actors in IDSR
Community-Based Surveillance Focal Person (Community Health Worker)
Employ simplified case definitions designed for community use to effectively identify priority diseases, health conditions, or potential hazards within the community.
Conduct regular household visits systematically to monitor community health status and detect potential health events.
Establish and maintain regular communication with key informants within the community to gather timely health-related information and insights.
Actively attend local ceremonies and community events to observe and follow up on any unusual occurrences, such as unexpected absences of individuals who were expected to be present.
Document priority diseases, health conditions, or unusual health events using standardized reporting forms and tools (like tally sheets), ensuring timely reporting within 24 hours of detection.
Participate in verbal autopsies by conducting structured interviews using questionnaires provided by health facility supervisors to gather information on deaths occurring in the community.
Promptly notify the nearest health facility and other relevant sectors about any unexpected or unusual cases of disease or deaths affecting humans or animals for immediate verification and investigation, adhering to International Health Regulations (IHR) and IDSR strategy timelines (within 24 hours).
Engage local leaders actively to gather insights on disease events and understand prevailing health trends within the community, fostering community ownership of surveillance.
Sensitize the community on the importance of reporting and seeking healthcare for priority diseases, health conditions, and any unusual health events to enhance community participation in surveillance.
Support health workers during case or outbreak investigations by assisting with contact tracing efforts and community-level data collection.
Mobilize local authorities and community members to garner support for and participation in public health response activities, ensuring broad community involvement.
Participate in risk mapping exercises to identify potential hazards and engage in training activities, including simulation exercises to enhance preparedness.
Participate in containment and response activities in close coordination with the district level, ensuring a unified and effective response.
Engage in various response activities, which may include home-based care provision, promoting social or behavior change related to traditional practices, and managing logistics for distribution of drugs, vaccines, or other essential supplies; providing trusted health education during crises is also a valuable contribution.
Provide feedback to community members regarding reported cases, actions taken, and progress of prevention activities to maintain community trust and engagement.
Verify if planned public health interventions are implemented as intended and ensure active community involvement in these interventions to maximize effectiveness and community ownership.
Participate in meetings organized by sub-district, district, and higher-level authorities to share community-level insights and contribute to broader surveillance and response planning.
Health Facility Staff and Point of Entry
Identify cases of priority diseases using the standard case definitions to ensure consistent and accurate case identification.
Document case-based information and report immediately notifiable diseases, conditions, and events to the next administrative level for prompt action and response.
Liaise effectively with the district level to receive guidance on how to conduct immediate laboratory investigations for suspected cases, ensuring timely diagnostic confirmation.
Manage case treatment and ensure appropriate referral of cases when necessary to higher levels of care based on established protocols.
Actively prepare for and participate in outbreak investigation and response activities, including active case treatment and management within the health facility.
Report summary data and case-based data (weekly reports) to the next level in a timely manner to maintain regular data flow and inform higher-level surveillance.
Conduct simple data analysis (using graphs, tables, charts) at the point of data collection to monitor trends and patterns at the facility level.
Communicate diagnoses for outbreak-prone diseases to the appropriate authorities at the district and community levels for coordinated response actions.
Convene the district rapid response team when necessary to coordinate immediate response actions within the health district.
Identify resources needed for response (human resources, financial resources, essential commodities, communication tools like phone cards) and assess timeline for their deployment to ensure resource availability for effective response.
District Surveillance Officer at District Level:
Investigate and verify potential outbreaks, ensuring prompt confirmation and initiation of control measures, collect diagnostic samples appropriately, and advise on suitable treatment and prevention protocols based on evidence.
Prepare and thoroughly analyze weekly surveillance reports and submit them to higher authorities in a timely manner for regional and national level overview and action.
Ensure that all surveillance sites within the district consistently maintain surveillance reports and ledgers/logbooks appropriately, promoting standardized data recording and management.
Maintain a current and comprehensive list of all reporting sites within the district to ensure complete reporting coverage and monitoring.
Establish and maintain a robust database of all trained and registered healthcare workers who are designated to serve as surveillance focal persons at the reporting sites, as well as other Community-Based Surveillance Focal Persons (CBS FPs) for efficient communication and network management.
Ensure there is an adequate and consistent supply of essential data collection and reporting tools available at all surveillance reporting sites to facilitate smooth and uninterrupted surveillance operations.
Ensure that the IDSR standard case definitions for all priority diseases are well understood and consistently used by healthcare workers at each site, and provide on-the-spot training and clarification if needed to enhance diagnostic accuracy and reporting consistency.
Monitor key performance indicators (such as data timeliness and completeness) of the IDSR system as stipulated in the IDSR guidelines to evaluate system performance and identify areas needing improvement.
Periodically update graphs, tables, charts, etc., to visualize surveillance data and compare current data with previous months, quarters, weeks, or years (important for trend analysis and making informed recommendations for response actions).
Provide in-person feedback to surveillance reporting sites on a weekly or monthly basis regarding the quality and completeness of their reporting and the proper implementation of the IDSR system to enhance data quality and site performance.
Closely follow up (often through phone calls) with the reporting sites to ensure they report data on time and address any reporting delays or issues promptly.
Conduct regular supportive supervision visits to various surveillance sites, including health facilities, border entries, and communities, and build their capacity to effectively analyze and interpret their surveillance data to guide local decisions and actions.
Sign and date the inpatient and outpatient record books, registries, or line-lists to formally document the visit and provide written recommendations for data quality improvement.
Support healthcare facilities to verify alerts originating from the community and ensure appropriate follow-up and verification of community-reported events.
Arrange and lead the investigation of verified cases or outbreaks, ensuring thorough investigation and documentation of findings.
Maintain an updated line list of suspected cases under investigation for effective case tracking and management.
Assist healthcare facilities in the safe collection, proper packaging, secure storage, and timely transport of laboratory specimens for confirmatory testing to ensure accurate and timely laboratory diagnoses.
Receive laboratory results from the Province/Region and promptly communicate them to the concerned healthcare facility for immediate clinical and public health actions.
Conduct/coordinate on-the-job trainings for the surveillance sites to continuously build capacity and address knowledge gaps for surveillance staff, especially with new staff.
Review the quality of surveillance data from time to time by conducting data quality audits and develop appropriate measures to improve data quality in the district, ensuring data accuracy and reliability.
Maintain a rumor logbook to systematically record events reported for the surveillance site, including rumors and alerts, for tracking and follow-up.
Ensure cross-border (district-district) coordination and collaboration on surveillance issues and provide notification of any outbreaks in the neighboring district, promoting regional cooperation for disease control.
The District Health Management Team:
Coordination via District Medical Officer: Engage with the District Executive, District Commissioner, and Regional Medical Officer on overall surveillance activities and planning.
Support for District Surveillance Officer: Assist the local Surveillance Officer in carrying out planned tasks.
Integrate Surveillance into District Health Plans: Incorporate surveillance actions into the broader District Health Plan.
Resource Mobilization: Collaborate with district authorities to secure funding for local surveillance efforts.
Ensure Prompt Fund Disbursement: Facilitate the quick release of allocated funds for surveillance work.
Monitor IDSR Performance: Track the effectiveness of IDSR and the results from data analysis and monitoring tools.
Risk Mapping Participation: Engage in district risk mapping and contribute to action plan development based on findings.
Outbreak Response Support: Aid the EPR committee in setting up rapid response teams during outbreaks and ensure they are operational (refer to section 5).
Reporting Initial Investigation Findings: Communicate the results of initial investigations to the Province/Region authorities.
Community Assessment & Risk Mapping: Take part in community assessments and risk mapping initiatives.
EPR Committee Establishment and Functionality: Assist in setting up and ensuring the operational effectiveness of EPR committees.
Community Health Education Programs: Design, deliver training for, and implement community health education initiatives.
Response Training Support: Participate in and support response training for healthcare facilities and community members.
Collaborative Public Health Responses: Work with the Province/Region to choose and implement suitable public health response measures.
Timely Information and Education Planning: Plan and execute community information and education activities promptly.
Documentation of Response Activities: Keep records of all response actions taken.
Daily Situation Reports During Outbreaks: Provide daily reports on the district’s situation when outbreaks occur.
Other Political Leaders at the District Level:
Key Role of Political Leaders: Political leaders (e.g., Village, Ward, District Officers) are crucial in promoting behavioral changes for effective disease surveillance.
Roles:
Emergency Declaration Support: Back the declaration of public health emergencies.
Local Resource Inventory: Create an inventory of local resources (human, financial, logistics) for rapid response to prevent disease spread.
Hygiene and Sanitation Promotion: Promote adherence to hygiene and sanitation principles, including environmental cleanliness, latrine availability and use, safe water access, and personal hygiene practices like handwashing.
Reporting Illness Clusters: Report any clusters of illness or deaths to the nearest health facility.
Bylaw Implementation: Enforce bylaws to strengthen hygiene and sanitation practices.
Community Sensitization: Actively engage in sensitizing community members on promoting, maintaining, and sustaining good health.
Community-Based Health Program Facilitation: Support community-led planning, implementation, and evaluation of health programs at the Ward level (including IDSR).
Outbreak Follow-up: Conduct outbreak follow-up in coordination with healthcare providers and extension workers at the Ward level.
Administrative Support for Healthcare Providers: Offer administrative backup to healthcare providers at Ward and Village levels.
Legislative Enforcement Support: Support the enforcement of relevant laws to prevent and control infectious disease outbreaks.
Supervision of Hygiene and Sanitation Practices: Supervise subordinates to ensure adherence to hygiene and sanitation principles.
Regular Public Health Committee Meetings: Ensure regular meetings of the Public Health Care Committee (or Health Committee), especially during outbreaks.
Disease Pattern Discussion: Discuss disease trends and their implications for action in regular meetings with the District Medical Officer.
Committee Establishment and Facilitation: Ensure the establishment and smooth operation of various committees to carry out necessary activities.
Resource Mobilization for Disaster Response: Seek resources from diverse sources for disaster response, including epidemics.
Health Advocacy: Conduct advocacy on health issues through various district campaigns.
Regional or Provincial Health Management Team:
Regional/National Coordination: Engage with Regional/Provisional Commissioners and national health authorities (Chief Medical Officer/Director General of Health) on surveillance activities and planning.
Support for Regional and District Surveillance Officers: Assist Regional and District Surveillance Officers in executing planned surveillance tasks.
Integration of Surveillance into Regional/District Health Plans: Incorporate surveillance actions into regional/provincial and district health plans.
Resource Mobilization and Timely Fund Release: Secure funding and ensure the prompt disbursement of funds for surveillance and response activities.
District IDSR Performance Monitoring: Track the effectiveness of IDSR in districts and their data analysis.
Support for District Risk Mapping and Assessments: Assist districts with risk mapping, action plan development, and community assessments.
District Emergency Preparedness and Response Support: Support districts in emergency preparedness, response training, and overall public health response efforts.
Ministry of Health/National Level:
Establish Emergency Operation Center: Create a Public Health Emergency Operation Center and incident management framework.
Spokesperson and Risk Communication Plans: Designate a spokesperson and develop risk communication strategies.
IDSR Standards and Emergency Response Guidelines: Establish standards, policies, and guidelines for IDSR, and update emergency preparedness and response plans.
National Capacity Assessment and Improvement: Evaluate and enhance national-level capacity, including surge capacity for emergencies.
Resource Mobilization and Coordination for IDSR: Mobilize and coordinate resources from domestic and international sources to support IDSR activities.
IDSR Supervision, Monitoring, and Evaluation: Oversee, monitor, and evaluate IDSR activities comprehensively.
Epidemiological Bulletin Production and Dissemination: Develop and distribute epidemiological bulletins.
Epidemic Investigation Support: Support the investigation of suspected epidemic outbreaks.
National Data Management and Analysis Support: Offer data management and analytical support at the national level.
WHO and Other Partners: (UN Agencies, CDC, USAID, PATH MSF, REDCROSS, UNICEF)
Guideline Development: Assist in the creation of norms and the formulation of guiding principles.
Technical and Material Aid: Offer specialized support, knowledge, and tangible resources to improve surveillance, lab capabilities, and health data networks.
Fundraising for Activities: Back the process of securing financial resources for surveillance and outbreak response efforts.
IDSR Oversight and Assessment: Help with the direction, monitoring, and evaluation processes of IDSR implementation.
Administrative Support: Provide organizational assistance, for instance, in drafting funding applications.
Capacity Enhancement: Bolster skills through training programs and the provision of necessary equipment.
Emergency Response Support: During public health crises, deploy specialized personnel, rapid response teams, mobile labs, essential supplies, and immunizations.
Roles of a Nurse in IDSR
Nurses are essential for IDSR programs because they play key roles in healthcare delivery. Their broad patient interactions and diverse duties within healthcare settings make their involvement critical. Nurses often act as frontline healthcare providers, delivering care, patient education, and support. Their engagement in IDSR ensures early detection, rapid response, and effective management of disease outbreaks, ultimately improving community health outcomes.
Roles
Assessment and Reporting: Evaluate and report on priority disease cases, escalating information from local to higher authorities.
Coordination of Activities: Streamline IDSR coordination among various participants, including community members and technical staff at institutions such as the CDC. This ensures smooth operation and communication.
Planning and Preparation: Develop strategies and prepare for effective control of disease outbreaks within communities. This involves proactive measures and resource allocation.
Assistance in Monitoring and Evaluation: Actively participate in monitoring and assessing the effectiveness of disease outbreak programs. This ensures programs are on track and achieving goals.
Assessment, Analysis, and Reporting: Analyze and interpret data, then create clear reports on priority disease outbreaks, applying epidemiological knowledge.
Engagement in Immunization Programs: Participate in community immunization efforts to protect against vaccine-preventable diseases. Public health bodies advocate for early childhood vaccination against preventable diseases, a role nurses actively support.
Advantages of IDSR:
Cost-Effectiveness: Efficient use of existing health personnel and standard reporting formats for routine health data makes it economical.
Computerization Enablement: Facilitates the digitization of readily available data at a central point, improving data accessibility and management.
Capacity Building: Offers training and skill development opportunities for health personnel, enhancing workforce capabilities.
Community Engagement: Encourages community involvement in identifying and responding to disease outbreaks, fostering local ownership and participation.
Resource Efficiency: Streamlines effective resource application and allocation to areas of greatest need.
Rapid Public Health Response: Enables swift reactions to public health events, minimizing potential impact and spread.
Challenges in IDSR Implementation:
Financial Sustainability: Lack of consistent funding sources can hinder long-term IDSR activities and program stability.
Stakeholder Coordination: Poor collaboration among diverse stakeholders can impede unified and effective action.
Training and Staff Turnover: Insufficient training combined with high turnover of frontline health staff weakens system capacity.
Feedback Mechanism Issues: Unreliable feedback from higher to lower levels disrupts communication and responsiveness.
Supervision and Support Gaps: Inadequate oversight and assistance from higher levels diminishes field-level effectiveness.
Laboratory and Job Aid Deficiencies: Weak laboratory resources and limited availability of job aids (like case definitions and reporting forms) hamper accurate and timely data collection.
Communication and Transport Limitations: Poor communication channels and transport systems, especially at local levels, slow down response times.
Data Management and Analysis Capacity: Insufficient skills in data management and analysis at various levels limit effective data use.
Resistance to Integrated Approaches: Opposition to shifting from traditional disease surveillance methods to a more integrated IDSR approach can slow progress.
Community Engagement and Ownership Deficit: Lack of community participation and ownership of the IDSR system can undermine its local effectiveness.
Animal and Human Health System Linkages: Weak connections between animal and human health surveillance systems hinder a “One Health” approach.
Political Commitment and Leadership Shortcomings: Insufficient political will and leadership can impede sustained IDSR implementation and resource allocation.
Fragmented Health Information Systems: Disjointed health information systems can hinder data sharing and comprehensive analysis.
Limited Digital Technology Use: Underutilization of digital technologies and innovations to improve IDSR efficiency and reach.
Adapting to Evolving Epidemiology: Challenges in modifying IDSR strategies to address changing disease patterns and new health threats.
Outbreak Detection and Response Capacity: Limited ability for prompt outbreak identification, investigation, and effective response actions.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

