Surgical Conditions of the Ear, Nose, and Throat (ENT)
Subtopic:
Furunculosis

Furunculosis is an infection affecting the skin-lined external ear canal. This infection can be localized to a specific area or spread throughout the canal (diffuse). It manifests as a boil, also known as a furuncle, within the ear canal. This boil arises from a deep skin infection, leading to the accumulation of pus within the lesion.
Causes of furunculosis
The primary causes of furunculosis are:
Bacteria: Common bacterial culprits include Staphylococcus aureus, Pseudomonas aeruginosa, and Streptococcus pyogenes.
Viral & Fungal infections: Though less common, viruses and fungi can also cause this condition.
Other factors that can make someone more likely to develop furunculosis include:
Allergy: Allergic reactions can irritate the ear canal, making it more susceptible to infection.
Foreign bodies: Objects lodged in the ear can cause injury and create a breeding ground for bacteria.
Presence of infected water in the ear: Water contaminated with bacteria can introduce infection into the ear canal.
Injury to the ear: Trauma to the ear canal can compromise the skin barrier, increasing the risk of infection.
Clinical features
The noticeable signs and symptoms of furunculosis often include:
Pain and tenderness on pulling the ear: The pain is often described as throbbing and is exacerbated by manipulating the outer ear.
Itching: This is particularly common if the infection is fungal in nature.
Swelling: The ear canal may become visibly swollen and inflamed.
Pus discharge: A thin, mucus-like discharge containing pus (mucopurulent) may drain from the ear.
Hearing loss: If the swelling from the boil blocks the ear canal (meatus), it can lead to a temporary reduction in hearing.
Inflammation of the neighboring lymph nodes: The lymph nodes around the ear may become swollen and tender as the body fights the infection.
Difficulty in chewing: In some cases, the pain and inflammation can make chewing uncomfortable.
Diagnosis/Investigations
Diagnosing furunculosis typically involves:
History and physical examination: A doctor will ask about the symptoms and examine the ear canal visually.
Pus swab for microscopy, culture and sensitivity: If there is a discharge, a sample of the pus is taken to identify the specific microorganism causing the infection and determine which antibiotics it is susceptible to.
NB: The appearance of the discharge can provide clues about the type of infection:
Whitish or black discharge: Suggests a fungal infection.
Yellow discharge: Suggests a bacterial infection.
Management of furunculosis
Treatment for furunculosis generally includes:
Thorough cleaning of the ear by wicking: Gently cleaning the ear canal to remove debris and discharge using a cotton wick.
Antibiotic ear drops: Applying antibiotic ear drops such as chloramphenicol 0.5%, typically 2 drops every 8 hours for 14 days.
Oral antibiotics (for severe cases): If the infection is severe, oral antibiotics like cloxacillin capsules (250-500mg four times a day for 5 days) may be prescribed. For children, the dosage is typically 12.5-25mg per kilogram of body weight.
Steroid ear drops: Steroid ear drops like betamethasone can help reduce inflammation.
Analgesics for pain: Pain relievers such as paracetamol (PCT) 1g three times a day for 3 days or ibuprofen can help manage the discomfort.
Warm or cold compresses: Applying warm or cool compresses can also help relieve pain.
Antifungal treatment (if fungal): If the cause is fungal, antifungal medications such as clotrimazole solution (applied once daily for 4-8 weeks) or oral fluconazole (200mg once daily for 10 days) may be used.
Proper drying of the ear: Ensuring the ear canal is thoroughly dried after cleaning or bathing, often done by ear wicking, is crucial to prevent recurrence.
Complications
If left untreated or if the infection spreads, potential complications of furunculosis can include:
Otitis media: Infection spreading to the middle ear.
Meningitis: Infection spreading to the membranes surrounding the brain and spinal cord.
Septicemia: A serious condition where the infection enters the bloodstream.
Sinus thrombosis: The formation of a blood clot within the venous sinuses of the brain.
NURSING CARE PLAN OF FURUNCULOSIS MANAGEMENT
Assessment: Swelling
Diagnosis: Impaired Skin Integrity related to pus buildup as evidenced by tender lumps in the ear canal.
Planning (Goals/Expected Outcomes): Promote skin healing and alleviate discomfort.
Implementation:
Administer prescribed antibiotics or antifungal medication based on the determined cause (bacterial or fungal).
Encourage the use of warm compresses to promote drainage from the furuncle.
Provide analgesic medication as prescribed to manage pain and discomfort.
Educate the patient on proper ear care and hygiene practices.
Rationale:
Medication is targeted to address the underlying infection, whether it is bacterial or fungal in origin.
Warm compresses are beneficial in aiding the natural drainage process and providing pain relief.
Analgesic medication is used to effectively alleviate pain and enhance patient comfort.
Patient education is crucial for preventing further complications and promoting effective self-care.
Evaluation: Skin Integrity was improved and the patient verbalized comfort.
Assessment: Hearing loss if occluding the meatus.
Diagnosis: Impaired Hearing related to occlusion of the meatus as evidenced by the patient verbalizing reduced hearing ability.
Planning (Goals/Expected Outcomes): Restore and maintain optimal hearing.
Implementation:
Administer prescribed medications to reduce inflammation within the ear canal.
Encourage the patient to keep the ear dry and to avoid inserting any foreign objects.
Monitor hearing status regularly and provide support as needed.
Rationale:
Medication is used to reduce inflammation, which in turn aids in the restoration of hearing function.
Keeping the ear dry and avoiding foreign objects helps prevent further complications and irritation.
Regular monitoring of hearing ensures early intervention if hearing status does not improve or worsens.
Evaluation: Patient verbalized having had his hearing restored.
EPISTAXIS
This refers to bleeding from the nose, commonly known as a nosebleed. The bleeding can originate from arteries, veins, or capillaries within the nasal passages.
Causes of epistaxis
Nosebleeds can be triggered by issues within the nose itself (local causes) or by broader health conditions (general causes).
LOCAL CAUSES
These are issues directly affecting the nasal passages:
Foreign bodies in the nostrils: Objects inserted into the nose can irritate and damage the delicate lining, leading to bleeding.
Fracture in the base of the skull: A break in the bone at the bottom of the skull can damage blood vessels in the nasal area, causing bleeding.
Nose Picking: This common habit can injure the fragile blood vessels lining the inside of the nose.
Trauma like blow to the nose: A direct hit to the nose can rupture blood vessels.
Tumours or new growth in the nose: Abnormal tissue growth can be fragile and prone to bleeding.
Nasal polyps: Soft, noncancerous growths in the nasal passages can sometimes bleed.
Rupture of an artery or blood vessel in the nasal cavity: A blood vessel within the nose may spontaneously break and bleed.
GENERAL CAUSES
These are systemic conditions or disorders that can contribute to nosebleeds:
Hypertension: High blood pressure can put extra pressure on the blood vessels in the nose, making them more likely to bleed.
Bleeding disorders (lack of clotting factors): Conditions that prevent blood from clotting properly can lead to prolonged or recurrent nosebleeds.
Renal failure: Kidney problems can affect blood clotting and increase the risk of nosebleeds.
Genetical inheritance (i.e. run in families) like in Telangiectasia (dilated small blood vessels): Some inherited conditions cause abnormally dilated small blood vessels that are prone to bleeding.
Allergic reactions: Nasal allergies can cause inflammation and irritation, making the nasal lining more susceptible to bleeding.
Sickle cell trait or diseases: These blood disorders can affect blood flow and vessel integrity.
Infections like Ebola, typhoid, Crimean Congo, Marburg fever, malaria etc.: Certain severe infections can damage blood vessels and lead to bleeding, including nosebleeds.
Rupture of distended blood vessel: In some cases, a blood vessel in the nose can become abnormally enlarged and rupture.
Clinical Features
The primary sign of epistaxis is:
Bleeding from the nose: This is the most obvious symptom.
Other possible signs and symptoms include:
There may be pain in bleeding nostril: Discomfort or soreness in the nostril that is bleeding.
Signs and symptoms of shock in case of severe bleeding: If the bleeding is significant, the patient may exhibit signs of shock such as lightheadedness, dizziness, rapid heartbeat, and paleness.
Signs of the predisposing cause like Hypertension, Kidney failure, Ebola, malaria and typhoid: The patient may also show symptoms related to the underlying condition causing the nosebleed.
Management of Epistaxis
The approach to managing a nosebleed depends on how severe it is, what’s causing it, and where the bleeding is originating. Management can involve methods that don’t require medication (non-pharmacological) and those that do (pharmacological).
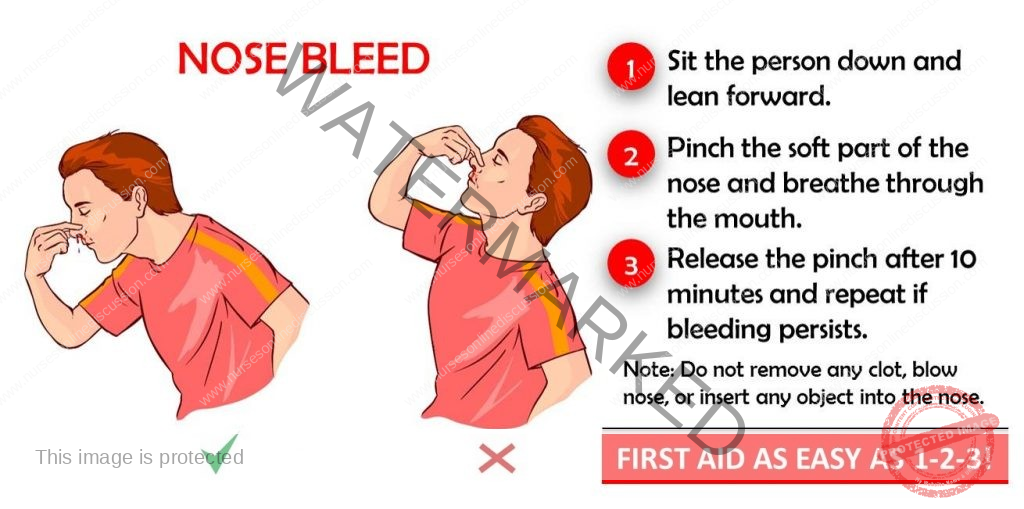
Non-pharmacological management/First aid
These are the initial steps to take when someone has a nosebleed:
Re assure the patient to allay anxiety: Calming the person down is important, as anxiety can sometimes make the bleeding worse.
Put the patient in sit up position if not in shock and instruct him to tilt the head forward to avoid pooling the blood in the posterior pharynx: Sitting upright prevents blood from flowing down the throat, which can cause nausea or choking. Tilting the head forward helps the blood drain out of the nose.
Instruct the patient to pitch nostrils (the soft parts the nose) between fingers and the thumb for about 10-15 minutes and breath via the mouth and spit out any blood: Applying direct pressure to the soft part of the nose helps to compress the bleeding vessels. Breathing through the mouth avoids swallowing blood.
Monitor vital observations i.e. TPR & BP to find out the underlying cause, if it is systemic: Checking temperature, pulse, respiration rate, and blood pressure can help identify potential underlying medical conditions contributing to the nosebleed.
Apply a cold compress on the fore head using ice pads to facilitate and aid vasoconstriction: Cold temperatures can cause blood vessels to narrow (vasoconstriction), which can help slow down or stop the bleeding.
If bleeding persists, pharmacological treatment is required.
When first aid measures are not enough to stop the nosebleed, medical interventions become necessary.
If the cause is a foreign body, it is removed if visible using forceps and antibiotics are given.
If an object is seen in the nostril, it should be carefully taken out using forceps. Antibiotics help prevent infection after the removal.
Pack the nose with a piece of gauze soaked with adrenaline or vitamin K or TEO using forceps to stop bleeding .It is can be left in position for 24-48 hours.
To apply pressure directly to the bleeding site, a gauze strip soaked in medication (like adrenaline to constrict blood vessels, vitamin K to aid clotting, or Terramycin Ear Ointment (TEO) which has antibacterial properties) is inserted into the nasal cavity. This packing is typically left in place for one to two days.
Cauterization with electrical cautery or diathermy machine to seal off the bleeders can be done in theatre.
In a medical setting, heat is used to seal the bleeding blood vessels. This procedure can involve electrical cautery or a diathermy machine, and is usually performed in an operating room.
Ligaturing of the bleeding blood vessels can also be done.
Surgical tying off of the bleeding blood vessel can be performed to stop the flow of blood.
Pressure can also be inserted on the bleeding area in the nose by inflating a special balloon which is inserted in the nose.
A specialized inflatable balloon is inserted into the nasal cavity and then inflated to apply direct pressure to the bleeding point.
In severe bleeding, the patient is resuscitated with IV Fluids like normal saline or given oral fluids to prevent shock and dehydration.
When significant blood loss occurs, intravenous fluids, such as normal saline, or oral fluids are given to restore blood volume and prevent the dangerous drop in blood pressure known as shock, as well as to combat dehydration.
Blood transfusion may also be considered depending on the lost blood after doing Hb, grouping and cross-matching.
If the amount of blood lost is substantial, determined by measuring hemoglobin levels and ensuring blood compatibility through grouping and cross-matching, a blood transfusion may be necessary.
Other investigations which may be done include;
Additional tests can help identify the underlying cause of the nosebleeds.
Blood for CBC to rule out underlying infections
A Complete Blood Count can help detect signs of infection that might be contributing to the nosebleeds.
Blood Slide (b/s) Rule out Malaria Parasites
A blood smear is examined under a microscope to check for the presence of malaria parasites, especially in areas where malaria is common.
Bleeding and clotting time
These tests measure how long it takes for blood to clot, helping to identify potential bleeding disorders.
Prevention of epistaxis
Taking steps to avoid nosebleeds is important.
Early treatment and control of predisposing conditions like Hypertension.
Managing underlying health issues such as high blood pressure can reduce the risk of nosebleeds.
Treatment of hemorrhagic infections like malaria and typhoid fever
Prompt and effective treatment of infections that can cause bleeding helps prevent nosebleeds associated with these illnesses.
Avoid nose picking
Refraining from picking the nose prevents damage to the delicate nasal lining.
Avoid violence that could lead to blows to the nose
Taking precautions to prevent facial injuries can help avoid trauma-induced nosebleeds.
Seeking for medical attention and advice in case of re-occurrence.
If nosebleeds happen repeatedly, it’s important to consult a doctor to identify and manage any underlying causes.
Complications
Potential problems that can arise from nosebleeds include:
Severe hemorrhage leading to anemia, hemorrhagic shock, septic shock
Significant blood loss can result in a deficiency of red blood cells (anemia), a life-threatening condition due to low blood volume (hemorrhagic shock), or shock caused by widespread infection (septic shock).
Sinusitis
Inflammation or infection of the sinuses can sometimes occur as a consequence of nosebleeds or their treatment.
Pneumocephalus (presence of air or gas within the cranial cavity)
In rare cases, air can enter the skull, especially after trauma or certain medical procedures.
Septal pressure necrosis
Prolonged pressure from nasal packing can damage the nasal septum, potentially leading to tissue death.
Neurogenic syncope during packing
Fainting can occur due to a nervous system response during the insertion of nasal packing.
Epiphora (from blockage of lacrimal duct)
Tear overflow can result if the tear duct is blocked, sometimes due to swelling or pressure from nasal packing.
Hypoxia from impaired nasal air movement)
Difficulty breathing due to blocked nasal passages from bleeding or packing can lead to a shortage of oxygen in the body.
Infections may result if sterility is not maintained especially in nasal packing.
If sterile techniques are not followed, particularly when inserting nasal packing, infections can develop.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2026 Nurses online discussion. All Rights Reserved

