Microbiology
Subtopic:
Infection Prevention and Control
Why study microbiology in Nursing:
To understand diseases caused by microorganisms
To gain insight on how microorganisms cause diseases in the human body
To understand the modalities of controlling infections
Gain insight on how to treat infections
Prevention of Protozoa Infections:
Proper disposal of wastes. Boiling of drinking water. Regular hand washing before and after defecation and eating and whenever need be. Educating the community including food handlers and health workers. Screening and treatment of all food handlers. Covering food and water to prevent contamination from house files. Proper cooking of meat. Using of insect repellants and bed nets.
Prevention of Helminth Infections:
Proper disposal of feaces. Avoid eating uncooked food. Daily washing of hands before and after eating food. Finger nails should be regularly cut to avoid collection of eggs. Treat the entire family at some time to prevent infections. Encourage people to wear shoes and sandals. Health education. Destroying intermediate host like snails. Avoiding contact with water known to contain cercarias like for shistosoma spp.
Infection Prevention and Control: Infection is the successful invasion and multiplication of micro-organism in or on body tissues with or without signs and symptoms. Infection can be classified as below;
Localized infection. Confined to a smaller part of the body
Disseminated. Infections which are widely spread in that is affect the body beyond the initial site of infection.
Systematic. Infection that affects the whole body.it is spread through blood and lymphatic system.
Types of Infection: Can be classified basing on anatomical site as Urinary tract infections, Respiratory infections, Vaginal infections, Skin infections etc.
Reservoirs of Infections:
Are places where pathogens grow and accumulate which include;
- Human reservoirs which include infected persons who are called carriers diseases such as typhoid can be transmitted from carriers. Carriers can be grouped into Patient with infection, Patient with acute infection, Convalescent carriers, Contact carriers.
- Non-living Reservoirs, include H2O, food, soil, Air and dead vegetation. Diseases such as cholera, tetanus, ebola.
- Animal reservoirs. Diseases can be transmitted from animal to humans. Animals reservoir include cattle, monkey, cats, dogs,ducks, rats etc.
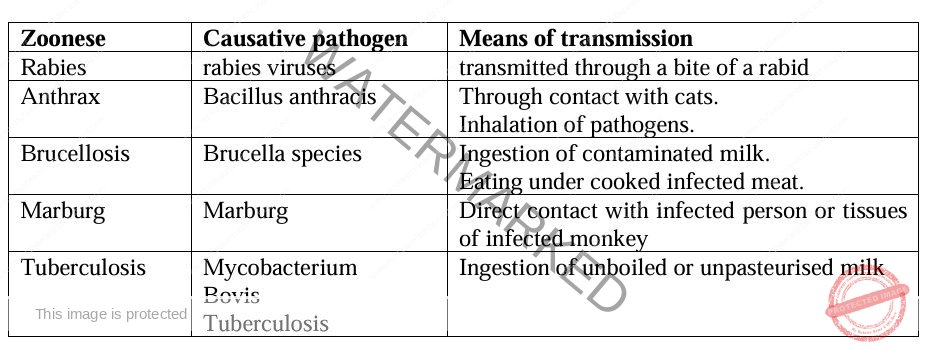
Zoonoses:
Are infectious diseases that infect animals but can be transmitted to human.
Can be transmitted through direct contact with infected animal tissues, or consumption of contaminated food stuffs like milk and meat. Examples:
Chain of Infection:
An infection can occur if all the six components are present and removal of one link in the chain prevents infection. Below are the components:
Causative agent. Refers to any micro-organism that is capable of causing disease these may be bacteria, viruses protozoa and fungi.
Reservoir. Is a environment, object in or on which micro-organism can survive and sometimes multiply. Common reservoirs include; animals, humans and non-living objects.
Portal of exit. The path by which an infectious organism leaves its reservoir. In relation to human may include; Respiratory tract, Skin, GIT, Genital, Urinary.
Mode of transmission. Is the means by which infectious organism pass from the portal of exist to the susceptible host, common modes of transmission include contact, vector borne and vehicle transmission.
Portal of entry. Is the path which an infectious organism goes through to ivadea susceptiblehost. The portal entry is usually similar to the portal exist.
Susceptible host. The host which is vulnerable to infectious. Vulnerability may occur as result of weakened immune system of the host due to age, health, status, chemotherapy.
Mode of Transmission of Infection:
This is the means by which pathogens pass from the portal exit in the reservoir to the susceptible host. The three major modes include;
Contact transmission: A person is exposed to a pathogen by either touching or being close to an infected person or object. Can be further divided into:
(i) Direct contact transmission involves person 2 person transmission through touching, kissing, sexual intercourse etc. common diseases in this route may include hepatitis A and sexually transmitted diseases.
(ii) Indirect contact. Is a where pathogens are transferred via non-living objects such as towels, eating utensils, thermometers; beddings which are contaminated disease include Hepatitis B.
Droplet transmission; involves transfer of pathogens via infections droplets generated through sneezing, coughing and laug….. diseases by this route include common cold, whooping cough, measles etc.
Vector transmission. Refers 2 transmission of an infectious disease by the bite of an infected (block flies and sand flies).
Vehicle transmission; involves transfer of pathogens via a medium like H2O, air, blood fluids and invenous fluids administered to the patients. These diseases include cholera, typhoid.
Classification of Infections:
Infections may be classified into 2 depending on the source of infections i.e. community acquired and hospital acquired.
Community Acquired: Are infections acquired within the community, they also include infections incubating during time of hospital admission.
Routes of transmission:
Fecal oral route. This can occur via contaminated food or house materials which are contaminated. Disease causing organisms include salmonella typhi, vibric cholera.
Airborne route. Are spread by inhalation of infectious droplets after infected person coughing, sneezing, laughing, organisms include; measles virus, influenza virus etc.
Direct in oculation. These occur when pathogens are injected into the body either due to accident, bite by infected animals / vectors air contaminated needles used on patients e.g plasmodium falciparum, guinea worm, HIV virus etc.
Trans placental/mother to child. Where infections are transferred from mother to child during pregnancy delivery and after delivery like T-reponema palladium, HIV etc.
Direct person to person contact. Most conditions on skin infections like ringworm, scabies etc.
Sexual contact.
Nosocomial Infections (Hospital Acquired Infections):
Are infections acquired from a hospital, or health care facility when the patient is admitted for any other reason. The most common nosocomial infections in Uganda include; Pneumonia, septicemia, Sepsis, antibiotic associated diarrhea.
Causes of Nosocomial Infections:
The common pathogens than can cause nosocomial infections are mainly bacteria and include; S. aureus, Proteus spp, ecoli, Websiellaspp – mycobacterium tuberculosis.
Sources of Nosocomial Infections:
They can be endogenous or exogenous i.e. Endogenous infection (Originates from the patients normal flora) or Exogenous infections (originates from external sources which include;
Acutely all patients, Asymptomatic patients (people incubating on infection), Inadequate sterilized equipment’s, Hospital staff during patient care, Healthy carries).
Main routes for transmission of nosocomial infections include; Contact with infected persons, Air borne, Direct inoculation, Facial oral routs.
Factors Contributing to Nosocomial Infection: Failure to health care workers to follow injection control guidelines. Increasing number of patients with compromise immunity. Overcrowding of patients in the hospital. Prolonged stay in the hospital. Age in that a patient with adversed age and young ones like babies are more susceptible to infections. Underlying diseases such as diabetes mellitus, renel failure tend to lead to increased susceptibility. Drugs being administered like nati-cancers and steroids tend to lower body or hosts’ immunity.
Patients at Risk of Nosocomial Infection:
Patients with compromised immunity due to diseases like HIV or immune suppressive drugs. Patients with broken skin (wound). Patients undergoing surgery characterization ventilation. Women in labour and delivery. Highly old and young patients.
Consequences of Nosocomial Infection: Prolonged stay in the hospital which may result into dark. Increases the cost of medical care i.e. drugs. Infected person may become a source of infections to other patients.
Prevention of Nosocomial Infection: Protecting patients with appropriate use of prophylactic anti-microbial, nutrition and vaccination. Limiting the risk of endogenous infections by minimizing invasive procedures and promoting optimal microbial use.
Prevention of infections among the staff members. Enhancing staff patient care. Surveillance of infections i.e. identifying and controlling outbreaks. Health education of both patients and staff members. Use of appropriate a septic practices like hand washing, sterilization, disinfection. Isolation of infectious patients from other patients.
Universal Precaution / Principles of Infection Prevention and Control:
Are a set of guidelines developed by the center of disease control and prevention in order to avoid contact with potentially infective body fluids and objects such as csf, pleural fluid, blood, amniotic fluid etc. which may harber infections such as hepatitis B, Hix. They include; Hand washing, Safe waste management, Adequate protective gears, Proper sharp disposal, Proper sterilization disinfectant.
Other general measures include:
Hand washing. This is effective measure for preventing the spread of pathogens. There must readily accessible hand washing facilities in a hospital. For example soap most especially liquid soap for hand washing and running water and towel for drying hands immediately after washing.
Sterilization, this is the process intendedto kill am microorganisms and is a highest level of microbial kill that is possible, sterilizers may be heat only, steam or liquid.
Cleaning, infections can be prevented fromaccuring in hospital/home as well in order to reduce their chances to contract on infections, patients medical perfuse are recommended to maintain.
Disinfection. Disinfection uses liquid chemicals on suraces and at room temperature to kill diseases causing microorganismultras let light has also been used to disinfect the rooms of patients infected with clostridium difficult after discharges.
Personal protective equipment e.g. gloves, bonnets, shoes, covers, face shield, surgical mask and respirators. Many are most of those items are disposable to avid carrying infections materials from the patients to another and to avoid difficult or costly to disinfection.
Auti microbial surfaces, microorganisms are known to survive on non-antimicrobial in animate “touch” surface e.g. bedrails, over-the-bed trays, call buttons, bathroom hard wore etc. as a public hygienic measure in addition to regular cleaning.
Vaccination of health care workers.
Waste Management and Disposal:
Refer to how the different wastes in hospital and homes are segregated. The methods used for disposal of wastes from hospital and homes are almost similar.
The main difference is the type and amount involved. In medical field wastes and their disposals is of high standards due to the fear of infection spread to the handlers and public.
General Principles of Segregation, Storage and Transportation:
All health care workers should understand the risks and safety procedures for the wastes they are handling.
All the containers which are filled with wastes should labeled to help the person in charge and to control the workers. Separate containers should be available in each a medical area for proper segregation of wastes. Local storages inside or near to a medical area may be needed if wastes are not collected frequently. Do not mix hazardous and non-hazardous wastes during collection, transport and storage. Collection wastes are often taken to central storage site before treatment and disposal.
Health Care Wastes:
Is the total wastes generated in healthy facility during health care service delivery like during diagnosis, prevention and treatment of diseases.
Types of Wastes:
Wastes may be classified into two;
Hazardous health care wastes (Is a waste with potential to cause harm to both human and environment if improperly handled. Almost 20% of all health care waste is estimated to be hazardous. Examples include; Un used blood, Human tissue, Contaminated animal carcasses, Disinfectants, Drugs, Needles, Syringes, Laboratory reagents, Swabs and bandages) and
Non-hazardous flow (Are wastes that are harmless to both humans and environment. They contribute almost 80% of wastes generated in a health facility, although they are harmless, they become nuisance when not appropriately disposed off. Examples include; papers, boxes, empty tins and discarded food).
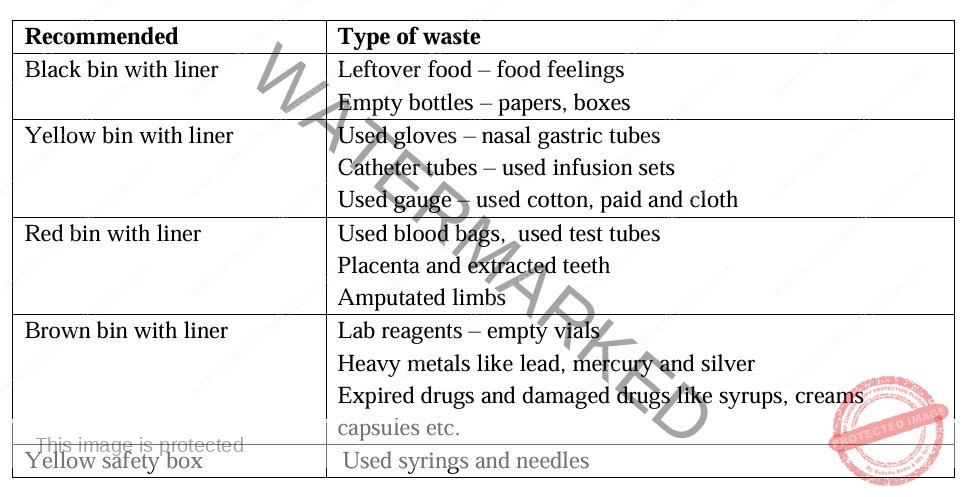
Segregation of Medical Wastes:
The responsibility of segregation of wastes lies one person who has generated the wastes.
All wastes should be segregated and disposed off in their appropriate container. Cobour coding also provides a visual indication of the potential risk posed by the wastes in that container i.e. Red – highly infectious wastes, Yellow – infectious wastes, Brown – pharmaceutical and chemical wastes, Black – general/noninfectious wastes, Yellow/ white sharp container for sharp wastes only.
Segregated wastes become easy to be carried by the workers in that if bins become full, its liner wrapped tightly and taken to incineration.
Waste Segregation Chart:
Sharp Disposal and Handling
A sharp is anything that can pierce, allowing a hazard to contaminate the recipient with infected body material. When handling sharps, needles must not be bent or broken by hand or removed from the syringe. All sharps should be disposed of in a safe manner, for instance, with the sharp part pointing down. Needles and syringes should be disposed of as a single unit into a puncture-resistant safety box. These sharp containers should be labeled. To avoid injuries, sharp containers should be filled up to only ¼ of their capacity and then sealed. It is important to avoid patient movements during the time of administering drugs by injection. Furthermore, avoid carrying and moving with sharps in hand; instead, dispose of them in a safety box immediately after the procedure. The safety box should be disposed of after sealing. The final disposal of sharps should involve being burnt and the residue buried.
To prevent accessibility to used sharps, seal sharp containers after use and dispose of them. Do not open a sealed container for re-use. Full safety boxes awaiting final disposal should be stored in a secure area that is only accessible to Health facility staff members and not the general public.
Strategies for Injection Safety and Waste Disposal
Effective strategies for injection safety and waste disposal include training health workers in injection safety issues and appropriate waste disposal. It is also beneficial to educate and encourage patients to seek treatment only from qualified providers. Support for the supervision of health workers involved in administering drugs and those who dispose of wastes is crucial. Additionally, organizing records for health workers who dispose of sharps well can be a useful measure.
Hand Washing
Hands are notorious for spreading infections from one person to another and should be washed before and after contact with each patient, before and after meals, before and after visiting the toilet, before and after breastfeeding, and whenever water is seen. Hand washing has been described as the most effective way of preventing cross-infection and is regarded as the single most important practice in preventing and controlling infection transmission. Hand washing is defined as the vigorous rubbing together of all lathered hand surfaces, including the skin up to the wrist (and up to the elbow for surgical scrubbing), for a minimum of 10 seconds, using running water, soap, and friction to remove all, or inactivate any transient microorganisms, debris, and organic materials.
Before the hand washing procedure, remove all jewellery, such as rings and watches. In case of the presence of a cut or injured tissue, cover it with an occlusive waterproof plaster. Keep the nails clean and without polish. Soap and soap dispensers should be clean.
During the procedure, wet hands and add some of the cleaning agent, i.e., soap, to form a lather. Pay attention to the area under the fingernails. Avoid splashing water on yourself and the floor because microorganisms can spread, and even the slippery floor is dangerous. Avoid touching other body parts with contaminated hands.
The teaching of hand washing involves several steps: palm to palm; right palm over the left dorsum and vice-versa; palm to palm with fingers interlocked; back of the fingers to opposing palm with fingers interlocked; rotational rubbing in the palm using the fingertips; and the right thumb clasped in the left palm and vice versa. Continue washing the hands for 1 minute, and two minutes for pre-operative use. Rinse the hands and dry them thoroughly. Dry hands from the elbow down using a single towel or disposable paper. Always keep the hands higher than the elbow. Drop the towel into the disposal bin.
Adequate Protective Gear
Adequate protective gear helps to protect the body from the infected body fluids of the patient. Examples include gloves to protect the hands, goggles to protect the eyes against splashes, an apron to protect clothes from contamination, face masks, face shields, and gumboots.
Definition of Terms
Disinfection: is the destruction of harmful microorganisms from a non-living object, except bacterial spores.
Aseptic: characterized by the absence of pathogenic microbes.
Sanitization: the reduction of microorganisms to levels considered safe by public health standards.
Decontamination: the process of making used instruments safer for handling before cleaning.
Cleaning: the process that removes foreign materials and organic matter, typically done using water and soap.
Pasteurization: a process used to eliminate pathogens from food using heat, such as milk.
Aseptic techniques: are measures used to prevent contamination of surgical instruments, medical personnel, and patients during procedures.
Bacteriostatic agent: agents that inhibit the growth of bacteria but do not kill them.
Bactericidal: agents that kill bacteria.
Related Topics
- Concepts of Microbiology
- Classification and Types of Microorganisms
- Pathogenic Microorganisms
- Normal Flora
- Characteristics and Mode of Spread of Disease-Causing Microorganisms
- Pathological Effects of Microorganisms
- Simple Laboratory Tests
- Infection Prevention and Control
- Introduction to Immunity
- Antibodies
- Principles of Immunization
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

