Specialized Nursing Care Procedure
Subtopic:
Neurological Assessment

Learning Objectives
Explain the purpose and indications for conducting a comprehensive neurological examination.
Identify and assemble the equipment necessary for a complete neurological assessment.
Describe the components of mental status evaluation and their relevance to neurological function.
Assess the 12 cranial nerves through appropriate functional and sensory testing procedures.
Perform and document evaluations of motor, sensory, and cerebellar functions accurately.
Interpret Glasgow Coma Scale scores to determine levels of consciousness and impairment.
A Neurological Examination
A neurological examination is a comprehensive assessment of a patient’s nervous system, including the brain, spinal cord, and peripheral nerves. It evaluates various functions, such as motor and sensory skills, balance, coordination, mental status, reflexes, and cranial nerve function.
Indications for a Neurological Exam
A complete neurological exam may be performed in the following situations:
Routine Physical Examination: As part of a general health check-up.
Post-Trauma: After any head, neck, or back injury.
Disease Monitoring: To track the progression of a neurological disease.
Specific Complaints: When a patient presents with symptoms such as:
Headaches
Blurred vision
Behavioral changes
Fatigue
Balance or coordination problems
Numbness or tingling in the extremities
Weakness or decreased movement in the arms or legs
Fever
Seizures
Slurred speech
Tremor
Level of Consciousness Assessment: To evaluate a patient’s awareness and responsiveness.
Paresthesia Assessment: To determine the extent of sensory loss in a body part.
Cranial Nerve Function Assessment: To evaluate the function of the 12 cranial nerves.
Important Note: During the assessment, ensure that the patient cannot see the substances or objects used for testing sensory functions (e.g., taste, smell, touch) to avoid biased results.
Equipment for the Procedure
Tray with:
Ophthalmoscope or Flashlight: To assess pupil responses.
Snellen Chart: To assess visual acuity.
Otoscope: To examine the ear canal and eardrum.
Tuning Fork: To assess hearing.
Pins or Needles: To assess pain sensation.
Cotton Wool: To assess light touch sensation.
Hot and Cold Water: In containers to assess temperature sensation.
Salt and Sugar: In containers to assess taste sensation.
Coffee or Lemon: In containers to assess the sense of smell.
Nasal Speculum: To examine the nasal passages.
Tape Measure: To measure areas of sensory loss.
Skin Pencil: To mark areas of sensory loss.
Reflex Hammer: To assess deep tendon reflexes.
Bedside:
Handwashing Equipment
Screen: For patient privacy.
Sharps Container
Adequate Lighting
Components of a Neurological Exam
A neurological exam typically includes the following components:
1. Mental Status Examination:
Level of Awareness: Assessed through conversation, evaluating the patient’s orientation to person, place, and time.
Attentiveness: Observe if the patient can maintain focus and attention during the exam.
Orientation: Assess orientation to self, place, and time. Disorientation to time usually precedes disorientation to place or person. Disorientation to self often suggests a psychiatric condition.
Speech and Language: Evaluate fluency, repetition, comprehension, reading, writing, and naming abilities.
Memory: Test both immediate recall (registration) and recent/remote memory (retention).
Higher Intellectual Function: Assess general knowledge, abstract thinking, judgment, insight, and reasoning.
Mood and Affect: Observe the patient’s emotional state and outward expression to determine if psychiatric issues might be influencing the neurological assessment.
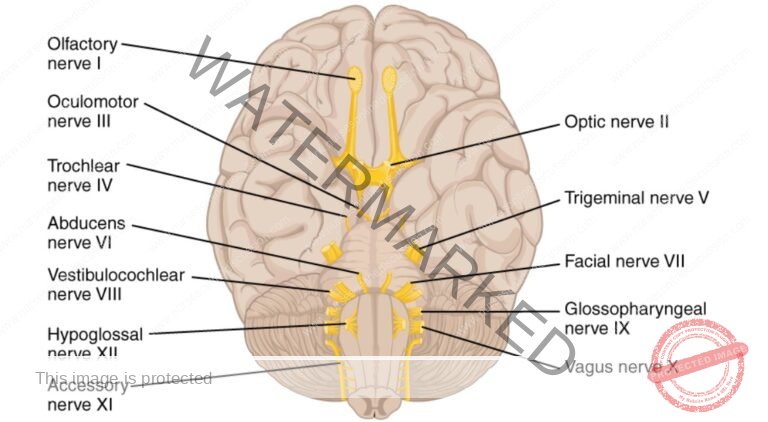
Evaluation of the Cranial Nerves
A complete neurological examination often includes an assessment of the 12 cranial nerves to evaluate brain function. Here’s a breakdown of how each nerve is typically assessed:
Cranial Nerve I (Olfactory Nerve):
Function: Sense of smell.
Assessment: The patient, with eyes closed, is asked to identify familiar odors (e.g., coffee, lemon) presented to each nostril separately.
Cranial Nerve II (Optic Nerve):
Function: Vision.
Assessment:
Visual acuity is tested using a Snellen chart.
The eyes may be examined with an ophthalmoscope.
Visual fields may be assessed.
Cranial Nerve III (Oculomotor Nerve):
Function: Controls most eye movements (upward, downward, medial), pupil constriction, and upper eyelid elevation.
Assessment:
Pupil size and reactivity to light are assessed.
The patient is asked to follow a light or object with their eyes in different directions (without moving their head).
Cranial Nerve IV (Trochlear Nerve):
Function: Controls superior oblique eye muscle, responsible for downward and inward eye movement.
Assessment: The patient is asked to follow a light or object, particularly as it moves down and inwards, towards the nose.
Cranial Nerve V (Trigeminal Nerve):
Function:
Sensory: Sensation to the face, including the forehead, cheeks, and jaw, and the inside of the mouth.
Motor: Controls muscles of mastication (chewing).
Assessment:
Light touch and pinprick sensation are tested on different areas of the face.
The patient is asked to clench their teeth while the examiner palpates the masseter and temporalis muscles.
Cranial Nerve VI (Abducens Nerve):
Function: Controls lateral rectus eye muscle, responsible for outward eye movement.
Assessment: The patient is asked to look laterally (towards the ear) with each eye.
Cranial Nerve VII (Facial Nerve):
Function:
Motor: Controls muscles of facial expression.
Sensory: Taste sensation from the anterior two-thirds of the tongue.
Assessment:
The patient is asked to make various facial expressions (e.g., smile, frown, raise eyebrows, puff out cheeks, show teeth).
Taste may be tested using different substances (e.g., sweet, sour, bitter).
Cranial Nerve VIII (Vestibulocochlear or Acoustic Nerve):
Function: Hearing and balance.
Assessment:
Hearing is tested using a tuning fork or by whispering.
Balance may be assessed using specific tests.
Cranial Nerve IX (Glossopharyngeal Nerve):
Function:
Sensory: Taste from the posterior one-third of the tongue, sensation to the pharynx.
Motor: Swallowing.
Assessment:
Taste may be tested on the back of the tongue.
The gag reflex may be tested.
Cranial Nerve X (Vagus Nerve):
Function:
Motor: Controls muscles involved in swallowing and speech.
Sensory: Sensation from the pharynx and larynx.
Parasympathetic: Innervates many internal organs, including the heart and digestive tract.
Assessment:
The patient is asked to swallow.
The gag reflex may be tested (often assessed along with CN IX).
The quality of the patient’s voice is observed.
Cranial Nerve XI (Accessory Nerve):
Function: Controls the sternocleidomastoid and trapezius muscles (involved in head turning and shoulder shrugging).
Assessment:
The patient is asked to turn their head against resistance.
The patient is asked to shrug their shoulders against resistance.
Cranial Nerve XII (Hypoglossal Nerve):
Function: Controls tongue movement.
Assessment:
The patient is asked to stick out their tongue and move it from side to side.
The patient’s speech is assessed for any difficulties.
13. Cranial Nerve Mnemonic:
it help you to remember the cranial nerves’ names

Nurses role in neurological examination
1. Provide a clam, suitable environment
2. Collect the personal data with patient &family members
3. Set the equipment needed for neurological examination
4. Assess the current level of consciousness, monitor vital parameters – temperature, pulse,
respiration, blood pressure, pupillary reaction, whether decelerating or decorticating.
5. Thorough mental status examination should be done & recorded
6. Assessment of cranial nerves should be done correctly & recorded.
7. Assessment of motor, sensory & cerebellar functions should be done & be recorded accurately.
8. During the examination, she should maintain a good support with patient &family members.
9. She should instruct the procedure correctly& then they should be asked to do it.
10. Should be informed to the concerned un it doctors if there is any
GLASGOW COMA SCALE MONITORING
| EYE OPENING | VERBAL RESPONSE | MOTOR RESPONSE | SCORE |
| No response | No verbal output | No motor response | 1 |
| Opens eyes to painful stimulus | Unintelligible sounds or words | Abnormal Extension to pain | 2 |
| Opens eyes when verbally instructed | Words are spoken but nonsensical | Abnormal Flexion to pain | 3 |
| Opens eyes on their own | Disoriented in conversation | Withdraws from painful stimulus | 4 |
| Answers questions correctly and appropriately | Reaches to remove painful stimulus | 5 | |
| Follows simple instructions | 6 |
GRADING
A GCS score of 13 or higher indicates mild impairment of consciousness.
A GCS score between 9 and 12 suggests moderate impairment of consciousness.
A GCS score of 8 or less indicates severe impairment of consciousness.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowRelated Topics
- Apply Nursing process to the management of patients
- Administer prescribed medicine appropriately
- Instilling medication
- Perform Shortening and removal of drains
- Perform Colostomy Care
- Prepare Abdominis Paracentesis (Abdominal Tapping)
- Prepare Lumbar Puncture
- Perform Gastrostomy Feeding
- Carry out gastric Lavage
- Perform Tracheostomy Care
- Ophthalmological Care
- Care of the patient`s ears
- Pre-Operative Eye Care
- Ear Care
- Peri-Operative Care:
- Orthopedic Nursing Care
- Prepare for Neurological Assessment
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

