Integumentary Disorders of the Skin
Subtopic:
stings and bites

The terms “stings and bites” describe injuries where the skin surface is breached by animals, insects, or plants. These injuries can lead to a spectrum of reactions, ranging from minor localized irritation to severe systemic medical conditions.
The terms “sting” and “bite” are specifically used to differentiate the nature of the injury and the method by which it is inflicted.
Insect Bites:
Mechanism: Insect bites occur when certain insects, such as mosquitoes, fleas, or bedbugs, use their specialized mouthparts to penetrate the skin.
Purpose: This skin penetration is typically for feeding purposes, as these insects extract blood from the host.
Common Symptom: Insect bites typically result in localized itching at the site of the skin puncture.
Insect Stings:
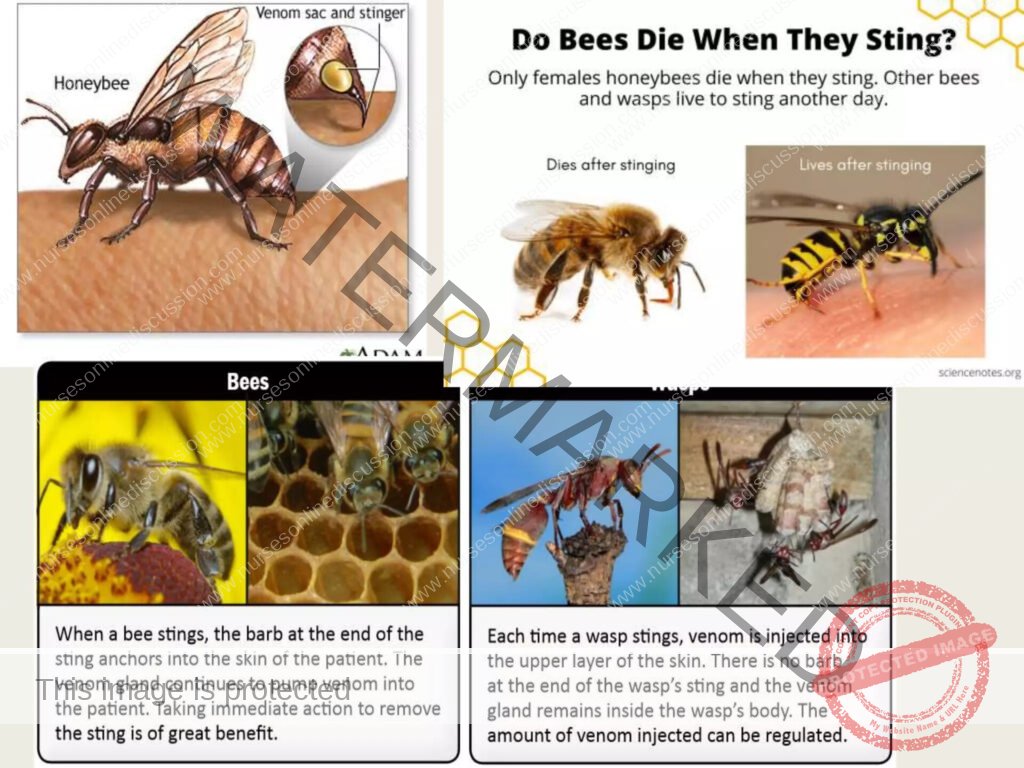
Mechanism: Insect stings are delivered by insects like bees, wasps, or hornets, which utilize a barbed stinger or other specialized body part to pierce the skin.
Purpose: The primary purpose of stinging is defense. Insects inject venom into the skin as a protective mechanism when they feel threatened or disturbed.
Other Animal Bites and Stings:
Animal Bites: Animal bites, exemplified by dog bites, occur when an animal uses its teeth to puncture or lacerate the skin. The mechanism is typically forceful tearing or puncturing of tissue by teeth.
Animal Stings: Animal stings encompass injuries from creatures like jellyfish or scorpions. These animals employ a specialized body part – such as nematocysts in jellyfish or a stinger in scorpions – to inject venom into the skin. The mechanism involves venom delivery through specialized structures.
Plant Stings:
Mechanism: Certain plants are equipped with minute needles or hairs on their leaves or stems. When contact is made, these needles or hairs can detach and become embedded in the skin.
Effect: These plant structures, once lodged in the skin, cause localized discomfort and irritation. Plants possessing such features are known as stinging plants.
INSECT STINGS AND BITES – Causes
The likelihood of insect stings and bites is influenced by several factors, primarily revolving around the presence of insects, individual behaviors, and environmental conditions.
Sources of Stings and Bites:
Insects: A wide range of insects are common culprits for both stings and bites:
Bees
Wasps
Hornets
Mosquitoes
Ants (especially fire ants or other stinging varieties)
Arachnids: This group, though technically not insects, includes common biting and stinging creatures:
Spiders (though most spider bites are not clinically significant, some species are a concern)
Ticks
Contributing Factors:
Environmental Exposure: Time spent outdoors, particularly in natural environments where insects are abundant, directly increases the risk. High-risk environments include:
Forests
Gardens
Fields
Areas near standing water (for mosquitoes)
Provocation of Insects: Many stinging insects, like bees and wasps, are not inherently aggressive but will sting defensively if they feel threatened. Provoking actions can include:
Disturbing nests or hives.
Making sudden movements near them.
Accidentally stepping on them (especially bees in ground nests).
Attractants: Certain elements can inadvertently attract insects, increasing the chance of encounters and potential stings or bites. These attractants include:
Sweet scents and perfumes that mimic floral odors.
Bright clothing colors that may attract insects.
Sweet foods and drinks left exposed outdoors, which attract foraging insects like wasps and bees.
Seasonal Influence: Insect activity levels are strongly influenced by temperature and weather patterns. Risk is generally higher during:
Warmer months (spring, summer, and early fall).
Periods of increased insect breeding and foraging activity.
Geographic Location: The types and prevalence of insects vary significantly across different geographic regions. Therefore, the specific risks of stings and bites are regionally dependent:
Certain areas may have higher populations of venomous spiders.
Some regions are known for aggressive bee or wasp species.
Mosquito-borne diseases are more prevalent in specific climates and locations.

Pathophysiology of Insect Stings and Bites
The body’s reaction to insect stings and bites is a multi-stage process that involves both direct effects of injected substances and the body’s immune response:
Exposure – Skin Penetration: The process begins when an insect stings or bites. This involves the insect using its biological tools:
Sting: Insects with stingers use this appendage to pierce the skin.
Bite: Biting insects utilize their mouthparts to puncture the skin surface.
Injection: Through either method (sting or bite), the insect introduces substances into the host’s skin.
Introduction of Venom or Saliva: The key element causing reactions is the injection of either venom (in stings) or saliva (in bites) into the skin.
Venom and Saliva Composition: These injected fluids are complex mixtures containing various compounds. These substances are foreign to the human body and can act as:
Irritants to tissues.
Triggers for the immune system.
Activation of the Immune Response: The body’s immune system recognizes components within the injected venom or saliva as foreign substances. This recognition triggers a defensive immune response.
Immune Chemical Release: Immune cells respond by releasing various chemical mediators. A primary mediator released is histamine.
Localized Effects at the Sting or Bite Site: The release of histamine and other inflammatory mediators primarily results in local inflammation, confined to the immediate area of the sting or bite. This localized inflammatory response leads to classic symptoms:
Redness: Due to increased blood flow to the area.
Swelling: Caused by fluid leaking from blood vessels into surrounding tissues.
Pain: Stimulation of pain receptors in the skin.
Itching: Histamine’s direct effect on nerve endings, causing the sensation of itch.
Systemic Effects (Potential): In some cases, the venom or saliva can extend beyond the local site and produce systemic effects, meaning effects that are felt throughout the body. Systemic reactions occur via two main pathways:
Allergic Reaction: In individuals with allergies, the immune system overreacts, leading to a widespread allergic response.
Toxic Reaction: Certain venoms are potent enough to cause toxic effects in the body even without a specific allergy, particularly if a large amount of venom is injected (e.g., from multiple stings) or in very sensitive individuals.
Signs and Symptoms of Insect Stings and Bites
Reactions to insect stings and bites can vary significantly, from mild local irritation to severe, systemic allergic reactions.
Localized Reactions: These symptoms are confined to the area of the sting or bite:
Localized Redness: Noticeable redness of the skin directly at and around the sting or bite location.
Swelling at the Site: Development of localized swelling around the area where the insect sting or bite occurred.
Pruritus (Itching): Itching sensations specifically at the sting or bite site, often ranging from mild to intense.
Pain or Tenderness: Localized pain or tenderness to the touch around the affected area.
Vesicle or Wheal Formation: Formation of a small blister (vesicle) or a raised, hive-like area (weal) at the sting or bite point.
Rash or Hives: Development of a localized rash or hives in the immediate vicinity of the sting or bite.
Puncture Mark or Stinger (Visible): In some cases, a visible puncture mark from the insect’s mouthparts or a retained stinger (especially from bees) may be apparent at the center of the reaction site.
Systemic Reactions: These indicate a more widespread response beyond the localized area:
Dizziness: Feeling lightheaded or faint.
Generalized Weakness: Overall feeling of bodily weakness.
Nausea: Feeling sick to the stomach, potentially with vomiting.
Headache: Development of a headache.
Signs and Symptoms of Anaphylaxis (Severe Allergic Reaction):
Anaphylaxis is a severe, potentially life-threatening allergic reaction to insect stings or bites (and other allergens). It constitutes a medical emergency requiring immediate intervention. Symptoms can develop rapidly and may include:
Respiratory Distress (Difficulty Breathing or Wheezing):
Subjective difficulty breathing or feeling short of breath.
Audible wheezing sounds when breathing, indicating airway constriction.
Facial, Oral, and Throat Swelling:
Rapid swelling of the face, particularly around the eyes and cheeks.
Swelling of the lips and tongue, potentially making it difficult to speak or swallow.
Throat swelling, creating a sensation of throat closure and airway obstruction.
Cardiovascular Changes (Rapid Heartbeat or Palpitations):
Rapid heartbeat (tachycardia) as the heart tries to compensate for decreased blood pressure and oxygenation.
Palpitations – awareness of a forceful or irregular heartbeat.
Generalized Skin Reactions (Severe Itching or Hives):
Severe, intense itching that is widespread over a large area of the body, not just localized.
Extensive hives breaking out over a significant portion of the skin surface.
Gastrointestinal Symptoms (Nausea, Vomiting, or Abdominal Pain):
Feeling of nausea, often accompanied by vomiting.
Abdominal pain or cramping.
Psychological Symptoms (Feeling of Impending Doom or Anxiety):
Sudden onset of intense anxiety or a sense of impending doom, a common subjective feeling during anaphylaxis.
Neurological Compromise (Loss of Consciousness or Collapse):
Loss of consciousness due to decreased blood flow to the brain.
Collapse or sudden inability to stand or remain upright.
Pathophysiology of Insect Stings and Bites
The body’s reaction to insect stings and bites is a multi-stage process that involves both direct effects of injected substances and the body’s immune response:
Exposure – Skin Penetration: The process begins when an insect stings or bites. This involves the insect using its biological tools:
Sting: Insects with stingers use this appendage to pierce the skin.
Bite: Biting insects utilize their mouthparts to puncture the skin surface.
Injection: Through either method (sting or bite), the insect introduces substances into the host’s skin.
Introduction of Venom or Saliva: The key element causing reactions is the injection of either venom (in stings) or saliva (in bites) into the skin.
Venom and Saliva Composition: These injected fluids are complex mixtures containing various compounds. These substances are foreign to the human body and can act as:
Irritants to tissues.
Triggers for the immune system.
Activation of the Immune Response: The body’s immune system recognizes components within the injected venom or saliva as foreign substances. This recognition triggers a defensive immune response.
Immune Chemical Release: Immune cells respond by releasing various chemical mediators. A primary mediator released is histamine.
Localized Effects at the Sting or Bite Site: The release of histamine and other inflammatory mediators primarily results in local inflammation, confined to the immediate area of the sting or bite. This localized inflammatory response leads to classic symptoms:
Redness: Due to increased blood flow to the area.
Swelling: Caused by fluid leaking from blood vessels into surrounding tissues.
Pain: Stimulation of pain receptors in the skin.
Itching: Histamine’s direct effect on nerve endings, causing the sensation of itch.
Systemic Effects (Potential): In some cases, the venom or saliva can extend beyond the local site and produce systemic effects, meaning effects that are felt throughout the body. Systemic reactions occur via two main pathways:
Allergic Reaction: In individuals with allergies, the immune system overreacts, leading to a widespread allergic response.
Toxic Reaction: Certain venoms are potent enough to cause toxic effects in the body even without a specific allergy, particularly if a large amount of venom is injected (e.g., from multiple stings) or in very sensitive individuals.
Signs and Symptoms of Insect Stings and Bites
Reactions to insect stings and bites can vary significantly, from mild local irritation to severe, systemic allergic reactions.
Localized Reactions: These symptoms are confined to the area of the sting or bite:
Localized Redness: Noticeable redness of the skin directly at and around the sting or bite location.
Swelling at the Site: Development of localized swelling around the area where the insect sting or bite occurred.
Pruritus (Itching): Itching sensations specifically at the sting or bite site, often ranging from mild to intense.
Pain or Tenderness: Localized pain or tenderness to the touch around the affected area.
Vesicle or Wheal Formation: Formation of a small blister (vesicle) or a raised, hive-like area (weal) at the sting or bite point.
Rash or Hives: Development of a localized rash or hives in the immediate vicinity of the sting or bite.
Puncture Mark or Stinger (Visible): In some cases, a visible puncture mark from the insect’s mouthparts or a retained stinger (especially from bees) may be apparent at the center of the reaction site.
Systemic Reactions: These indicate a more widespread response beyond the localized area:
Dizziness: Feeling lightheaded or faint.
Generalized Weakness: Overall feeling of bodily weakness.
Nausea: Feeling sick to the stomach, potentially with vomiting.
Headache: Development of a headache.
Signs and Symptoms of Anaphylaxis (Severe Allergic Reaction):
Anaphylaxis is a severe, potentially life-threatening allergic reaction to insect stings or bites (and other allergens). It constitutes a medical emergency requiring immediate intervention. Symptoms can develop rapidly and may include:
Respiratory Distress (Difficulty Breathing or Wheezing):
Subjective difficulty breathing or feeling short of breath.
Audible wheezing sounds when breathing, indicating airway constriction.
Facial, Oral, and Throat Swelling:
Rapid swelling of the face, particularly around the eyes and cheeks.
Swelling of the lips and tongue, potentially making it difficult to speak or swallow.
Throat swelling, creating a sensation of throat closure and airway obstruction.
Cardiovascular Changes (Rapid Heartbeat or Palpitations):
Rapid heartbeat (tachycardia) as the heart tries to compensate for decreased blood pressure and oxygenation.
Palpitations – awareness of a forceful or irregular heartbeat.
Generalized Skin Reactions (Severe Itching or Hives):
Severe, intense itching that is widespread over a large area of the body, not just localized.
Extensive hives breaking out over a significant portion of the skin surface.
Gastrointestinal Symptoms (Nausea, Vomiting, or Abdominal Pain):
Feeling of nausea, often accompanied by vomiting.
Abdominal pain or cramping.
Psychological Symptoms (Feeling of Impending Doom or Anxiety):
Sudden onset of intense anxiety or a sense of impending doom, a common subjective feeling during anaphylaxis.
Neurological Compromise (Loss of Consciousness or Collapse):
Loss of consciousness due to decreased blood flow to the brain.
Collapse or sudden inability to stand or remain upright.
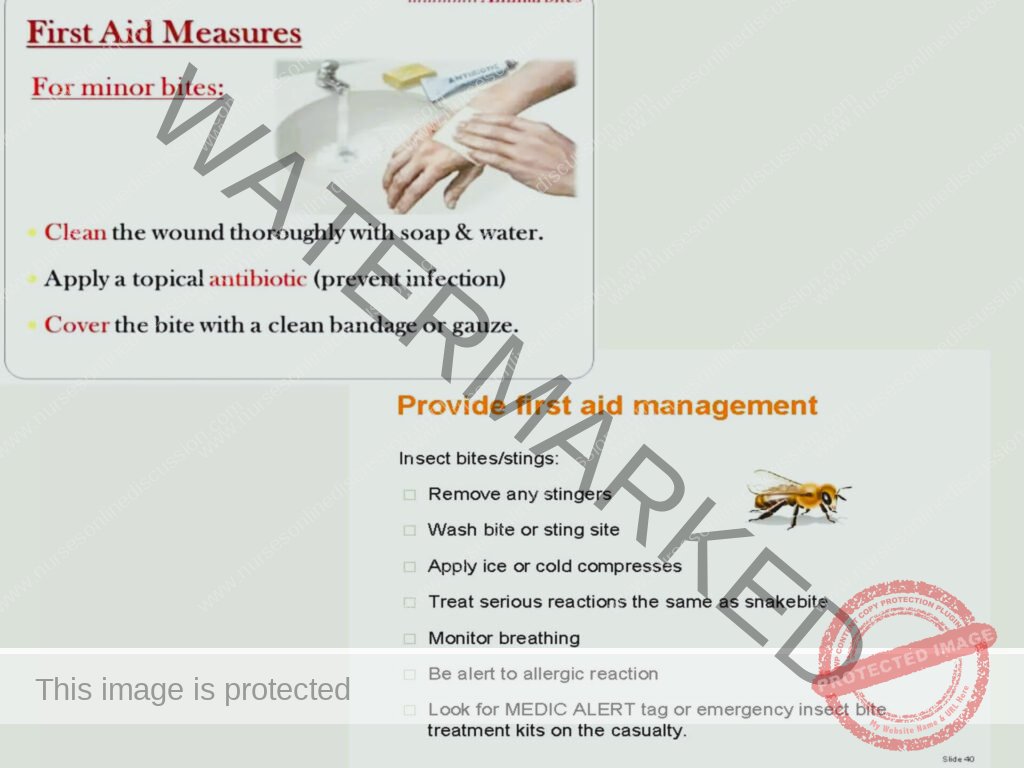
Management of Insect Bites and Stings
Immediate First Aid (During and Immediately After Sting/Bite):
Reassurance and Calm: Prioritize reassuring the casualty to reduce anxiety. Maintain a calm demeanor yourself to prevent further distress.
Stinger Removal (if applicable – Bee Stings): If a stinger is visible in the skin (common with bee stings):
Apply Firm Pressure: Use a blunt object’s edge (e.g., credit card, edge of a knife – not the blade, fingernail) to apply constant, firm pressure directly beside the stinger.
Scrape or Brush Off Stinger: Scrape or brush the stinger sideways and away from the skin surface. The goal is to remove it without squeezing the venom sac.
Avoid Tweezers: Do not use tweezers or forceps to pull out the stinger. Squeezing with tweezers can compress the attached venom sac, potentially injecting more venom into the wound.
Remove Constrictive Items (if applicable): If the sting or bite is on fingers, hands, wrists, or ankles, immediately remove any rings, bracelets, watches, or tight clothing. This is crucial in case swelling develops, which could restrict circulation if items are left in place.
Wash the Sting/Bite Site: Cleanse the area thoroughly but gently:
Wash with soap and water. Use a mild soap and clean water to wash the sting or bite site effectively to reduce risk of infection.
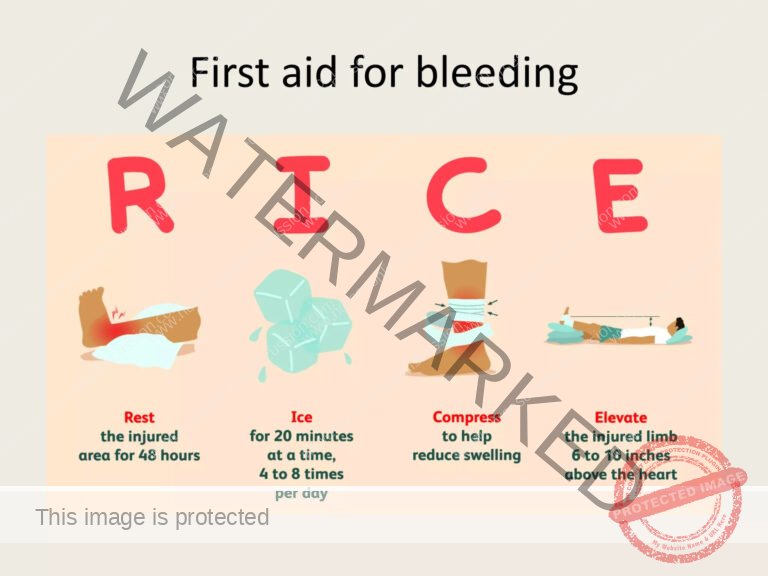
Cold Compress Application: Apply cold therapy to the affected area to reduce swelling and pain:
Prepare Cold Pack: Wrap ice or an ice pack in a clean, thin cloth or washcloth to prevent direct skin contact.
Apply Intermittently: Place the wrapped ice pack on the sting/bite site for 10 minutes, then remove it for 10 minutes. Repeat this cycle of 10 minutes on, 10 minutes off.
Avoid Direct Ice Contact: Never apply ice directly to bare skin as it can cause frostbite or cold injury.
Symptomatic Relief (for Itching): If itching is present and bothersome:
Antihistamines: Consider taking an over-the-counter antihistamine medication orally to help reduce itching and mild allergic symptoms.
Topical Creams: Apply anti-itch creams or lotions (like calamine lotion or hydrocortisone cream) to the sting/bite site for localized relief.
Monitor for Infection: Over the following days, closely observe the sting or bite area for signs of infection. Be alert for:
Increasing redness spreading beyond the initial area.
Worsening swelling that becomes excessive or spreads.
Increased pain or tenderness that intensifies over time.
Pus or any purulent discharge from the site.
Seek Medical Advice if Symptoms Persist or Worsen: Advise the individual to consult a doctor if:
Pain and swelling at the sting or bite site persist or worsen significantly beyond initial reaction.
Any signs of infection develop.
Systemic symptoms occur.
Important DO NOTs: Emphasize these points for safe first aid:
Do NOT apply a tourniquet. Tourniquets are generally not appropriate for insect stings or bites and can be harmful if improperly used.
Avoid Stimulants: Do NOT give stimulants (e.g., caffeinated drinks) as they are not helpful and may be counterproductive.
Avoid Aspirin (unless prescribed): Do NOT administer aspirin or other pain medications unless specifically prescribed by a healthcare professional. Note: Aspirin is generally contraindicated in children and adolescents due to the risk of Reye’s syndrome. Use acetaminophen or ibuprofen if pain relief is needed and appropriate.
Diagnosis of Insect Bites and Stings:
History of Exposure: Diagnosis often starts with a history of being bitten or stung by an insect, which may be witnessed or inferred from circumstances.
Physical Examination: A physical exam is essential to:
Visualize the bite/sting site to assess the appearance of the reaction.
Note characteristic signs such as localized swelling, redness, wheals, or puncture marks.
Allergy Skin Testing (Selective Cases): Skin allergy testing (skin prick or intradermal tests) may be conducted, particularly if:
There’s a history of severe allergic reactions to insect stings.
To confirm specific insect venom allergy for consideration of immunotherapy (allergy shots).
Medical Management:
In many mild cases, insect stings and bites resolve with first aid alone and may not require specific drug therapy. However, for more pronounced reactions or complications, medical management may include:
Antihistamines:
Purpose: To relieve itching and reduce the severity of allergic reactions, especially localized hives and itching.
Formulations: Can be topical (creams, lotions for localized itch) or oral (for more systemic relief).
Steroids (Corticosteroids):
Purpose: To reduce inflammation and suppress allergic responses in more significant reactions.
Administration: Systemic corticosteroids (oral or injectable) may be prescribed for moderate to severe reactions to reduce widespread inflammation. Topical corticosteroids are used for localized allergic contact dermatitis-like reactions.
Epinephrine (Adrenaline):
Life-Saving for Anaphylaxis: In cases of anaphylaxis (severe, life-threatening allergic reaction), epinephrine is the critical, first-line treatment.
Mechanism: Epinephrine works to reverse anaphylactic symptoms by:
Constricting blood vessels (raising blood pressure).
Relaxing airway muscles (improving breathing).
Reducing swelling and hives.
Administration: Typically administered via an epinephrine autoinjector (EpiPen) in emergency situations.
Prophylactic Antibiotics (Selective Use):
Limited Role: Antibiotics are not routinely prescribed for insect stings or bites.
Indication: Antibiotics may be considered prophylactically (to prevent infection) only in very specific circumstances, such as:
High risk of infection due to wound characteristics (e.g., deep puncture wounds).
Compromised immune system.
Evidence of early infection developing.
Safety Precautions to Minimize Risk:
Use Insect Repellents: Apply insect repellents containing DEET, picaridin, IR3535, or oil of lemon eucalyptus to exposed skin and clothing when outdoors to deter insects.
Protective Clothing: When in insect-prone areas, wear protective clothing to minimize exposed skin:
Long pants.
Long-sleeved shirts.
Closed-toe shoes.
Escape Attack Swarms (Bees/Wasps): If you encounter an aggressive swarm or attack:
Face Protection: Cover your face immediately to protect eyes, nose, and mouth.
Run Away: Run in a straight line as quickly as possible away from the area.
Use Shield if Possible: Try to grab a net, coat, towel, or any object to use as a temporary shield for protection while escaping.
Seek Shelter: Seek immediate shelter indoors – inside a house, tent, or car – and close doors and windows.
Avoid Attracting Insects:
Scent Awareness: Avoid wearing perfumes and strong fragrances that can attract insects.
Clothing Color: Avoid bright clothing and floral patterns, as these can be more attractive to certain insects.
Bee Pursuit: Be aware that bees can pursue perceived threats for a considerable distance, up to 400 meters (approximately 1300 feet). Bees are relatively slow fliers; most people can outrun them in an escape situation.
Colony Awareness: Stay alert for signs of bee or wasp colonies, like bees entering or exiting cracks in walls or ground nests. If you notice a colony, do not provoke it, and maintain a safe distance to avoid accidental stings.
When to Seek Emergency Medical Care:
Seek immediate emergency medical attention if any of these signs or symptoms develop after an insect sting or bite, as they may indicate a severe allergic reaction (anaphylaxis):
Respiratory Distress:
Trouble breathing.
Wheezing sounds during breathing.
Shortness of breath, feeling like you can’t get enough air.
Swelling of Face and Oral Area:
Swelling anywhere on the face, including eyelids, cheeks.
Swelling in the mouth, lips, or tongue.
Throat Symptoms:
Throat tightness, feeling like the throat is closing up.
Difficulty swallowing.
Cardiovascular/Neurological Symptoms:
Feeling weak, lightheaded, or dizzy.
Sudden drop in blood pressure, leading to faintness or dizziness.
Loss of consciousness or fainting.
Skin Color Changes:
Turning blue (cyanosis) around the lips or face, indicating oxygen deprivation.
Prevention of Insect Stings and Bites (Proactive Measures):
Avoid Provoking Nests: Steer clear of insect hives or nests, and avoid making rapid, jerky movements that might be perceived as threatening.
Scent and Color Choices: When outdoors, avoid wearing strong perfumes or heavily scented lotions and choose clothing in neutral or light colors, avoiding dark or floral patterns that can attract insects.
Use Insect Repellent: Consistently use insect repellents as directed when spending time outdoors, especially during peak insect activity times.
Protective Clothing: Wear appropriate protective clothing, such as long sleeves, long pants, socks, and closed shoes, to minimize exposed skin in areas where insects are prevalent.
Caution with Food Outdoors: Exercise caution when eating or drinking outdoors, especially sweet foods and beverages, and keep food covered to avoid attracting bees and wasps, particularly around garbage cans and picnic areas.
Emergency Kit and Epinephrine (for Known Allergies): If you have known severe allergies to insect bites or stings:
Carry an emergency allergy kit containing prescribed medications.
Always have an epinephrine autoinjector (EpiPen) readily available.
Ensure that family members, friends, and caregivers are thoroughly trained on how to recognize anaphylaxis symptoms and how to administer the EpiPen correctly in case of an emergency reaction.
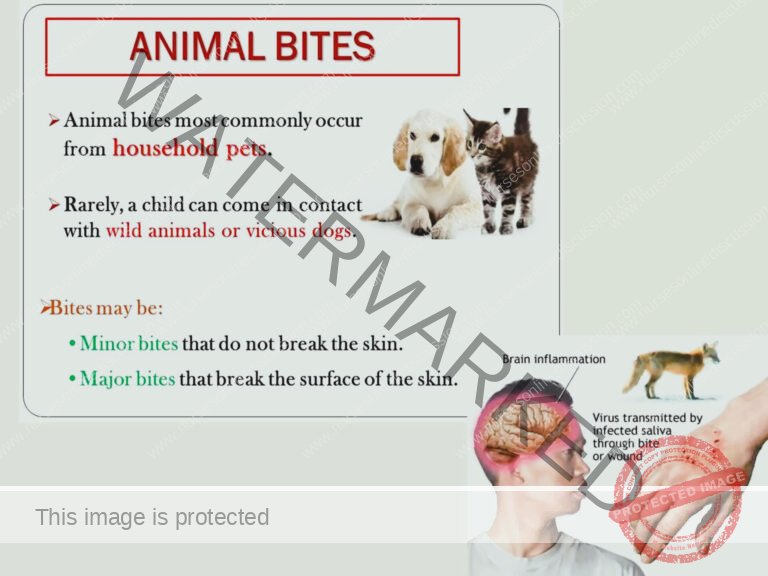
ANIMAL BITES
Animal bites, especially in children, are a common occurrence and can result in puncture wounds. It is important to properly manage these bites to prevent complications such as infection
and the transmission of diseases like rabies
General Wound Care:
Rinse the wound with saline water or sterile water under pressure to remove any dirt or debris. Wash the surrounding skin with soap and water to reduce the risk of infection.
Apply a clean dressing to protect the wound and promote healing.
If possible, elevate the affected body part to help control bleeding.

Medical Interventions (Following Animal Bites and Puncture Wounds):
Tetanus Prophylaxis:
Purpose: Tetanus is a serious bacterial infection that can enter through puncture wounds or breaks in the skin. Tetanus toxoid vaccination is crucial for prevention.
Administration: Tetanus toxoid should be administered if the injured person’s tetanus vaccination status is not up-to-date. This is especially important if they have not received a booster in the past 5-10 years, or if their primary vaccination series is incomplete or unknown.
Assessment of Vaccination History: Healthcare providers will assess the patient’s vaccination history to determine the need for a tetanus booster or initial vaccination.
Prophylactic Antibiotics (Selective Use):
Not Routine: Antibiotics are not routinely prescribed for all animal bites and stings. Most minor wounds heal without them.
Indications for Antibiotics: Prophylactic antibiotics may be considered in specific situations to prevent bacterial infection, such as:
High-Risk Wounds: Wounds considered at high risk for infection, including:
Deep puncture wounds that are difficult to clean thoroughly.
Crush injuries with tissue damage.
Bites to the hands or feet, which have higher infection risk.
Immunocompromised Individuals: Patients with weakened immune systems are at greater risk of infection, so antibiotics may be more strongly considered.
Signs of Early Infection: If there are early indicators of infection already present at the time of initial assessment (e.g., increased redness, warmth, pus).
Antibiotic Choice: If antibiotics are deemed necessary, the specific antibiotic and duration will be chosen based on the type of wound and local guidelines.
Debridement of Lacerations:
Purpose: Debridement is the surgical removal of devitalized (dead or damaged) tissue from a wound.
Necessity: Debridement may be necessary for lacerations (tears in the skin) resulting from animal bites.
Benefits: Debridement helps to:
Remove contaminated tissue that could harbor bacteria and lead to infection.
Promote wound healing by creating a cleaner wound bed and removing barriers to tissue repair.
Suspected Rabies Infection (Animal Bites – Specific Concern):
Rabies Suspicion – Immediate Action: If there is any suspicion of rabies exposure from an animal bite, immediate medical attention is absolutely crucial. Rabies is a fatal disease if it develops, but post-exposure prophylaxis can prevent it if administered promptly.
Anti-Rabies Immunoglobulin (Rabies Ig):
Passive Immunity: Rabies Immunoglobulin (Rabies Ig) provides immediate, passive immunity. It contains pre-formed antibodies against the rabies virus.
Administration: Rabies Ig is administered as part of post-exposure prophylaxis to provide rapid, short-term protection while the body develops its own immune response from vaccination.
Wound Infiltration: A portion of the Rabies Ig dose is typically injected directly into and around the wound site to neutralize the virus locally.
Inactivated Rabies Vaccine:
Active Immunity Induction: Inactivated rabies vaccine is administered to stimulate the body’s own immune system to produce antibodies against the rabies virus, resulting in active immunity.
Vaccine Series: Rabies vaccination is typically given as a series of injections over several weeks to build up immunity.
Concurrent Administration: Rabies vaccine is given concurrently with Rabies Ig in post-exposure prophylaxis for unvaccinated individuals to provide both immediate and long-term protection.
Urgency is Paramount: Rabies post-exposure prophylaxis (both Rabies Ig and vaccine) is most effective when given as soon as possible after a potential rabies exposure. Any delay increases the risk of rabies infection developing.
Animal Safety – Prevention of Bites (Education and Best Practices):
Educating Children About Animal Safety:
Approach Unfamiliar Animals with Caution: Teach children never to approach unfamiliar animals (dogs, cats, etc.) without adult supervision and permission. Emphasize that even animals that appear friendly can be unpredictable.
Vaccinate Pets Regularly: As a pet owner, ensure your pets are regularly vaccinated according to veterinary recommendations. This protects them from diseases like rabies and also reduces the risk of disease transmission through bites to humans.
Avoid Teasing or Provoking Animals: Instruct children clearly that teasing, bothering, or provoking animals is never okay. Actions to avoid include:
Pulling tails or ears.
Throwing objects at animals.
Cornering or chasing animals.
Respect Animal Space and Boundaries: Teach children to respect an animal’s personal space. When approaching even familiar animals, do so gently and calmly, allowing the animal to see and acknowledge you.
No Direct Eye Contact with Threatened Animals: Explain to children that if they encounter an animal that seems scared, threatened, or aggressive, they should avoid direct eye contact. Direct eye contact can be misinterpreted by a threatened animal as a challenge or aggressive stare, potentially triggering a defensive bite.
Never Interfere with Feeding or Young: Children should be taught never to take food away from an animal while it’s eating or to approach or handle baby animals or disturb a mother animal with her young. These situations can make animals very protective and defensive.
Cautious Approach to Restrained Animals: Emphasize that even restrained animals (e.g., dogs on leashes, animals behind fences) should be approached with extreme caution. Restraint can sometimes make an animal feel more vulnerable and potentially more reactive.
Avoid Running from Dogs: Advise children not to run directly in front of a dog. Running can trigger a dog’s chase instinct, and what starts as playful chasing can escalate into nipping or biting. Instead, teach children to remain calm and still or back away slowly.
Supervise Inexperienced Feeders: Inexperienced individuals, especially children, should never be allowed to feed dogs unsupervised. They may not understand canine body language or appropriate handling techniques and could inadvertently provoke a bite.
Alert Animals to Your Presence: When approaching an animal from behind or when entering a space where an animal may be present (e.g., going around a corner), make noise to alert the animal to your presence before getting too close. This avoids startling the animal, which can trigger a defensive reaction.
Insect Repellent for Pets: Consider using pet-safe insect repellents on your animals as directed by a veterinarian. This can help prevent bites from insects like fleas and ticks, which can indirectly affect humans in the household.
Socialize Pets Properly: Socialize your pets, especially dogs, from a young age to ensure they are comfortable and well-behaved around different people and in various situations. Proper socialization reduces anxiety and aggression.
Children Should Not Lead Dogs: Do not allow young or inexperienced children to lead dogs on leashes. Children may not have the physical strength or understanding of dog behavior to safely control a dog, especially if the dog becomes excited, scared, or aggressive.
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

