Anatomy & Physiology 2
Subtopic:
The Endocrine System
EDOCRINE SYSTEM

General Function
The nervous system and the endocrine system are the two main coordinating and controlling systems of the body. There are several differences between these two systems. For example, the nervous system acts by means of electric impulses and chemical stimuli; whereas the endocrine system has more widespread, slower, and longer lasting effects.
The endocrine system also has more generalized effects on such activities as growth, metabolism, and reproduction. Despite this difference, however, the two systems are closely interrelated.
Hormones
The chemical messengers released by the glands of the endocrine system are called hormones. Hormones are released directly into the bloodstream and carried to the tissues they affect. These tissues may be far from where the hormone is produced.
The blood reaches all cells of the body, but only certain cells respond to specific hormones; these responding cells are unique in that they have receptors to which the hormones attach.
Only cells that have receptors for a given hormone will respond to that hormone; these cells make up what is called the target tissue.
Chemistry
Hormones fall chemically in two categories:
- Proteins. Most hormones are proteins or related compounds composed of amino acids. All hormones except those of the adrenal cortex and the sex glands are proteins.
- Steroids are hormones derived from lipids and produced by the adrenal cortex and the sex glands.
All hormones are extremely potent, that is, they are effective in very small amounts.
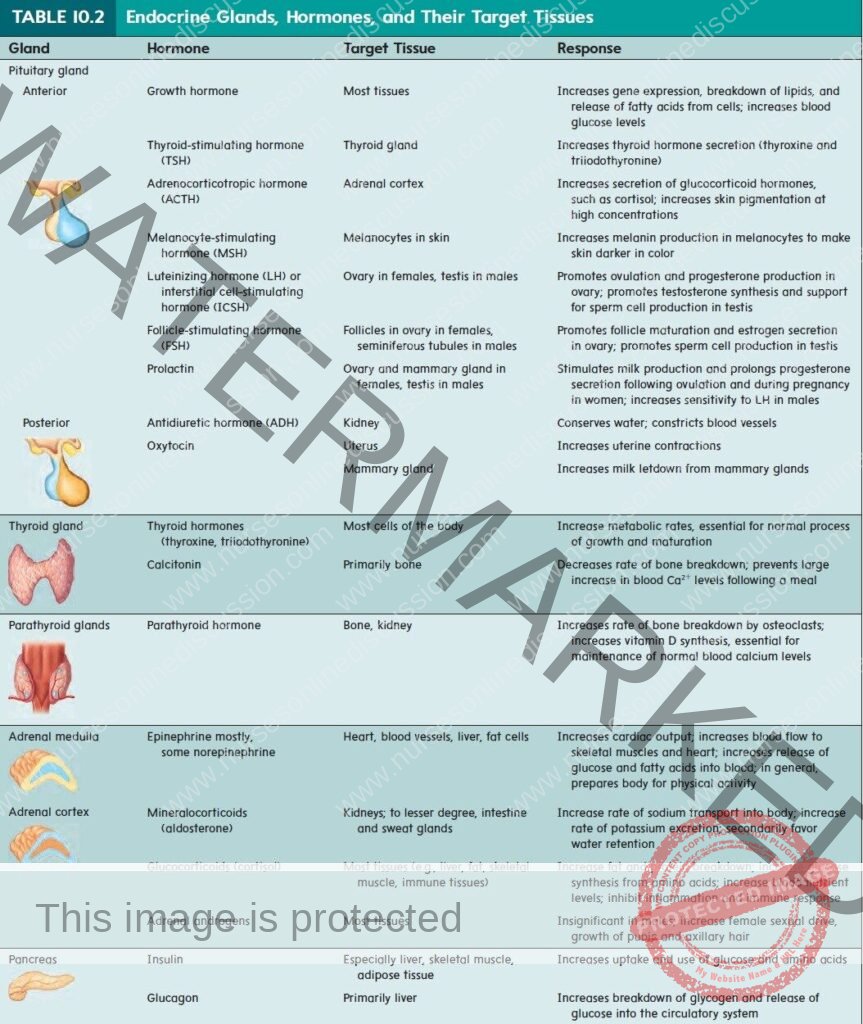
The Endocrine Glands and Their Hormones

The endocrine system consists of the glands that secrete hormones. These glands are also called the ductless glands because they secrete directly into the blood stream, in contrast to the endocrine glands, which secrete into body cavities.
Most endocrine glands, like exocrine glands, are made of epithelial tissue. Although they have no ducts, they have an extensive blood vessel network. Operations on endocrine glands, for example on the thyroid, require care in the control of bleeding.
The organs believed to have the very richest blood supply of any in the body are the tiny adrenal, or suprarenal glands, which are located near the upper part of the kidneys.
Some of the glands included in this system, such as the pancreas and the sex glands, have other non-endocrine functions as well, but hormone secretion is one of their main functions.
In addition, some body organs, such as the stomach, small intestine, and kidney, produce hormones, but since their main function is not hormone production, they are not discussed.
The Pituitary Gland
The pituitary gland or hypophysis, formerly called the “Master gland”, secretes several polypeptide hormones that directly or indirectly regulate a wide variety of metabolic and physiologic processes essential to normal growth and development as well as to the maintenance of homeostasis.
Many of the hormones secreted by the pituitary gland are critical to the activity of target glands, including the thyroid, adrenal and gonads.
Anatomy
The pituitary gland (hypophysis cerebri) is located at the base of the brain, resting within the Sella turcica of the sphenoid bone. The pituitary gland maintains elaborate neural and vascular connections with the hypothalamus of the brain, which plays a central role in the integration of neuroendocrine activity.
The pituitary gland has two major divisions: The anterior lobe (adenohypophysis) and the posterior lobe (neurohypophysis).
The hormones released from each lobe are;
Adenohypophysis:
- Somatotrophs, which secrete growth hormone (GH) or somatotropin.
- Lactotrophs, which secret prolactin (PRL).
- Corticotrophs, which produce corticotropin (ACTH) and
- beta-lipotropin (beta-LPH)
- Thyrotrophs, which secrete thyrotropin (TSH).
- Gonadotrophs, which produce follicle stimulating hormone (FSH) and luteinizing hormone (LH)
Neurohypophysis:
The neurohypophysis, which is connected directly to the hypothalamus by the infundibular (Pituitary) stalk, is rich in nerve fibers of hypothalamic origin (the hypotahlamohypophyseal tract) produce two hormones: Antidiuretic hormone (ADH or Vasopressin) and oxytocin.
These hormones are then transported along the axons of the hypothalamo hypophyseal tract to the posterior lobe of the pituitary gland for storage and ultimate release under hypothalamic control.
Hormones of the Adenohypophysis
The secretion of hormones by the adenohypophysis is controlled by hypothalamic regulatory (hypophyseotropic) hormones that are transported to the pituitary gland by the hypothalamohypophyseal portal system.
There are six recognized hypophyseotropic hormones secreted from the median eminence of the hypothalamus:
- Growth hormone-releasing hormone (GHRH; somatocrinin)
- Growth hormone-inhibiting hormone (GHIH; somatostatin)
- Corticotropin-releasing homone (CRH)
- Thyrotropin-releasing hormone (TRH)
- Gonadotropin-releasing hormone (GnRH)
- Prolactin-inhibiting hormone (PIH)
- GnRH stimulates secretion of FSH and LH.
- TRH stimulates the secretion of TSH and prolactin.
- Somatostatin inhibits the secretion of growth hormone and TSH.
Growth Hormone (GH); Somatotropin (STH)
Human growth hormone (hGH) is a peptide hormone composed of 191 amino acids, and is secreted by the somatotrophs of the adenohypophysis primarily under hypothermic control. The wide variety of factors that may affect
GH secretion is summarized below.
Actions
Effects on Growth:
Growth is a complex phenomenon influenced by genetic, nutritional, and hormonal factors. In addition to growth hormone, the thyroid hormones, insulin, androgens, and estrogens play important roles in normal human growth and development at various times of the life cycle.
GH accelerates overall body growth by increasing the mass of both skeletal and soft body tissues through hyperplasia (increased cell number) and hypertrophy (increased cell size).
The effects of GH are particularly evident in skeletal tissues where chondrogenesis (cartilage formation) and osteogenesis (bone formation) are enhanced, leading to an increase in linear growth and stature before epiphyseal closure and increased bone thickness following closure of the epiphyses.
Follicle-Stimulating Hormone (FSH)
Control of Secretion
Follicle-stimulating hormone (FSH) is a glycoprotein gonadotropic hormone whose secretion is stimulated by hypothalamic GnRH.
Inhibit, a polypeptide produced by testicular sertoli cells in the male and follicular granulosa cells in the female, acts directly on the adenohypophysis to inhibit FSH secretion.
Actions
Follicle-stimulating hormone directly stimulates the sertoli cells in testicular seminiferous tubules, there by promoting spermatogenesis in the male.
In the female, FSH stimulates follicular growth and development within the ovaries.
- Luteinizing Hormone (LH; Interstitial Cell Stimulating
Hormone; ICSH)
Control of Secretion
Like FSH, LH is a glycoprotein hormone whose secretion is stimulated by GnRH. Testosterone inhibits LH secretion through a direct action on the adenohypophysis, as well as indirectly by inhibiting hypothalamic GnRH production.
The effects of female hormones on LH secretion are more complex. Constant, moderate levels of estrogen (without progesterone) have a negative feedback effect on LH. High levels of progesterone and estrogen (luteal phase of the ovulatory cycle) inhibit LH secretion.
Actions
In the male, this hormone stimulates testosterone production by testicular interstitial cells; hence the alternate name, interstitial cell stimulating hormone (ICSH).
In the female, LH promotes maturation of ovarian follicles and sustains their secretion of estrogens. LH is also responsible for ovulation and the formation of the corpus luteum.
Thyroid-Stimulating Hormone (Thyrotropin; TSH)
Control of Secretion
Thyrotropin-releasing hormone (TRH) and cold (especially in infants) promote secretion of TSH by the thyrotrophs of the adenohypophysis. Elevated plasma levels of free thyroid hormones (T3 and T4) inhibit thyrotropin secretion. Stress also inhibits TSH secretion.
Actions
Thyroid-stimulating hormone maintains the structural integrity of the thyroid gland and promotes the synthesis and release of thyroid hormones thyroxine (T4) and triiodothyronine (T3).
Hormones of the Neurohypophysis
Antidiuretic Hormone (ADH; Vasopressin)
ADH is a polypeptide hormone of hypothalamic origin that is stored in and released from the neurohypophysis in response to a variety of stimuli.
Actions
The principal physiologic role of ADH is to regulate extracellular fluid volume and osmolality by controlling the final volume and concentration of urine. ADH increases the permeability of the distal nephron (late distal convoluted tubules and collecting ducts) to water.
The enhanced reabsorption of water from the renal tubules results in the production a concentrated urine that is reduced in volume. A large amount of this hormone causes constriction of smooth muscle in blood vessel walls and raises blood pressure (the name vasopressin).
Oxytocin:
The two major physiologic actions of oxytocin are exerted on the female breast and uterus.
Actions
It causes uterine contractions and triggers milk ejection from the breast. The ejection of milk from a lactating mammary gland follows a neuroendocrine reflex initiated by sucking, which stimulates cutaneous receptors in the areola of the breast. Oxytocin is carried by the blood to the mammary gland, where it causes contraction of myoepithelial cells surrounding the alveoli and lactiferous ducts to bring about the ejection of milk (milk letdown).
In lactating women, tactile stimulation of the breast areola, emotional stimuli, and genital stimulation may also lead to oxytocin release and activate the ejection of milk.
It also acts directly on uterine smooth muscle to elicit strong, rhythmic contractions of the myometrium. Uterine sensitivity to oxytocin varies with its physiologic state and with hormonal balance. The gravid (Pregnant) uterus is highly sensitive to oxytocin, particularly in the late stages of gestation.
Uterine sensitivity to oxytocin is greatly enhanced by estrogen and inhibited by progesterone. Oxytocin release appears to follow a neuroendocrine reflex initiated by genital stimulation. It has been suggested that oxytocin may facilitate sperm transport through the female genital tract.
The Thyroid Gland
The hormones of the thyroid gland exert a wide spectrum of metabolic and physiologic actions that affect virtually every tissue in the body.
Anatomy
The thyroid gland is the largest of the endocrine glands. A bilobed ( two roughly oval lateral lobes on either side of the larynx connected by anarrow band called isthmus) its located in the neck overlying the trachea anteriorly. The thyroid gland is composed of numerous closely packed spheres or follicles.
Each follicle consists of a simple cuboidal epithelium (follicular cells) enclosing a lumen or cavity containing a viscous hyaline substance termed colloid.
The chief constituent of the colloid is the iodinated glycoprotein thyroglobulin. Interspersed among the follicles are small clusters of parafollicular (C) cells, which secrete calcitonin, a hormone affecting calcium metabolism.
Thyroid Hormones
The follicular cells of the thyroid gland secrete two hormones, thyroxine tetraiodothyronine or T4), triiodothyronine (T3).
Storage and release of thyroid hormones:
T3 and T4 remain stored within the colloid bound to thyroglobulin until a stimulus for secretion arrives. On stimulation by TSH, portions of the TGB (colloid) are engulfed by microvilli that extend from the apical surface of the follicular cells. Droplets of the engulfed colloid fuse with lysosomes, and proteolytic enzymes release T3 and T4 from the TGB. The hormones (T3 and T4) readily diffuse to nearby capillaries and enter the bloodstream.
Actions
The thyroid hormones increase the rate of metabolism, total heat production, and oxygen consumption in most body tissues. Exceptions include the adult brain, spleen, lymph nodes, uterus, and testes.
The thyroid hormones promote normal physical growth and development, and they are essential for normal myelination and development of the nervous system in early life. Hypothyroid infants exhibit severe mental retardation and defective myelination of nerve fibers.
In normal physiologic amounts, the thyroid hormones stimulate protein synthesis, increase lipid turnover, lower plasma cholesterol, and promote GI absorption of glucose. T3 is more potent and more rapidly active than T4; in fact, the latter may be considered a prohormone, since most target cells convert T4 into T3.
The Parathyroid Glands
The parathyroid glands, usually four in number, are embedded in the dorsal surface of the thyroid gland. In response to hypocalcemia (low plasma calcium), the chief cells of the parathyroid glands secrete a hormone known as parathyroid hormone (PTH).
Parathyroid hormone regulates serum calcium levels by exerting its effects on the following target tissues:
– Bone: PTH stimulates bone resorption by activating the bone-destroying osteoclasts. The demineralization of bone elevates plasma calcium and phosphate levels; however, the renal actions of PTH lead to a net decrease in plasma phosphate levels.
– Kidneys: PTH promotes renal tubular reabsorption of calcium and increases urinary excretion of phosphate by blocking its reabsorption. PTH also stimulates the activity of a renal enzyme that catalyzes the formation of calcitriol, an active metabolite of vitamin D.
Calcitriol elevates plasma calcium and phosphate levels primarily by promoting the intestinal absorption of both ions, but also by increasing renal tubular reabsorption of calcium and phosphate.
The Pancreas
The pancreas is located in the left upper quadrant of the abdomen, inferior to the liver and gall bladder and lateral to the first portion of the small intestines, the duodenum. It has two types of cells that perfom different function: acini secrete digestive enzymes (exocrine), scattered around the pancreas are specialized cells “little islands” called islets of langerhans that produce hormones (endocrine).
The Islets of Langerhans contain four types of secretary cells, as follows:
- Alpha (A) cells, which secrete glucagon
- Beta (B) cells, which secrete insulin
- Delta (D) cells, which secrete somatostatin
- PP (F) cells, which secrete pancreatic polypeptide
Insulin-secreting beta cells are the most numerous, making up to 75% of the islet cell population. The A cells containing glucagons comprise approximately 20% of islet cell mass, whereas the somatostatin−containing D cells account for 3% to 5% of pancreatic islet cells.
The F cells make up less than 2% of islet cells and secrete a polypeptide that slows food absorption in humans, but whose exact physiologic significance is unclear.
Somatostatin inhibits the secretion of insulin, glucagons, and pancreatic polypeptide. Insulin inhibits the secretion of glucagons, whereas glucagon stimulates the secretion of insulin and somatostatin.
Glucagon
Glucagon is a 29-amino-acid polypeptide hormone secreted by the alpha cells of the pancreatic islets primarily in response to hypoglycemia (low blood sugar). Glucagon is essentially a catabolic hormone that decreases carbohydrate and lipid energy stores and increases the amount of glucose and fatty acids available for oxidation.
Control of Secretion
The plasma glucose concentration is the major physiologic regulator of glucagons secretion. In addition to hypoglycemia and fasting, the following factors promote glucagons secretion: amino acids, exercise, stress, gastrin, cortisol, CCK, acetylcholine, and beta-adrenergic stimulation.
The rate of glucagons secretion is inhibited by elevated blood levels of glucose and free fatty acids, and by somatostatin, insulin, secretin, and alpha-adrenergic stimulation.
Major Actions
– Carbohydrate metabolism: Glucagon stimulates hepatic glycogenolysis, thereby promoting the release of glucose from liver glycogen stores.
Glucagon also interacts with receptors coupled to the activation of phospholipase C, which eventually leads to calcium influx and stimulation of glycogenolysis.
In addition to stimulating hepatic glycogenolysis, glucagon inhibits glycogenesis and raises the rate of hepatic gluconeogenesis. The net effect is an elevation of blood glucose (hyperglycemia).
– Lipid metabolism: Glucagon stimulates lipolysis, thereby increasing the release of free fatty acids and glycerol from adipose tissue. Glucagon also enhances hepatic ketogenesis by facilitating conversion of fatty acids to ketone bodies.
– Protein metabolism: Glucagon exerts a catabolic action on hepatic proteins and inhibits the incorporation of amino acids into hepatic protein.
Insulin
The secretion of insulin is regulated primarily by the blood glucose level, with an elevation of blood glucose (hyperglycemia), increasing both production and release of insulin. It promotes the uptake of glucose across the plasma membrane thus increasing cellular glucose uptake. Once inside the cell glucose is metabolized for energy.
It also increases the rate at which the liver and skeletal muscles convert glucose into glycogen (the storage form of glucose) and the rate at which the liver changes excess glucose into fatty acids. These fatty acids can then be converted into fats and stored in adipose tissue or liver.
It promotes the cellular uptake of amino acids and stimulates their manufacture into proteins.
Major Actions
- Cellular membrane permeability: Insulin facilitates the transport of glucose across selected cell membranes, thereby accelerating the entry of glucose into muscle, adipose tissue, fibroblasts, leukocytes, mammary glands, and the anterior pituitary.
The transport of glucose into the liver, brain, renal tubules, intestinal mucosa, and erythrocytes is independent of insulin. Exercise and hypoxia mimic the effect of insulin on cellular permeability to glucose in skeletal muscle.
The insulin requirements of diabetics engaging in strenuous exercise may be reduced substantially and therefore must be monitored carefully to avoid hypoglycemia. Insulin also increases cellular permeability to amino acids, fatty acids, and potassium, particularly in muscle and adipose tissue.
- Carbohydrate metabolism: Insulin effectively lowers the level of blood glucose by enhancing the transport and peripheral utilization of glucose. Insulin increases muscle and liver glycogen while inhibiting those that produce glycogenolysis. Glycolytic enzymes are also activated by insulin, whereas several enzymes involved in gluconeogenesis are inhibited.
- Protein metabolism: Insulin is strongly anabolic, increasing protein synthesis and inhibiting protein catabolism. Insulin increases the incorporation of amino acids into protein by accelerating the entry of amino acids into the cell and possibly by increasing RNA synthesis.
- Lipid metabolism: Insulin stimulates formation of triglycerides (lipogenesis) and inhibits their breakdown
(lipolysis). Insulin accelerates synthesis of fatty acid and glycerol phosphate and enhances cellular permeability to fatty acids, leading to increased deposition of triglycerides in adipose tissue.
Pancreatic Somatostatin
Unlike glucagons and insulin, pancreatic somatostatin does not directly regulate intermediary metabolism. Rather, it slows digestion and absorption of nutrients by exerting several inhibitory effects on digestive processes (eg, reduced gastric acid secretion decreased gastric emptying and inhibition of CCK secretion and gallbladder contraction). Pancreatic somatostatin secretion is stimulated by elevations and gastrointestinal hormones (eg, CCK).
The Adrenal Glands
The adrenal (suprarenal) glands are paired yellowish masses of tissue situated at the superior pole of each kidney. Each gland consists of two distinct entities an outer adrenal cortex and an inner adrenal medulla−that differ in embryologic origin, character, and function.
Adrenal Medulla
The adrenal medulla develops from the embryonic ectoderm. It remains functionally associated with the sympathetic nervous system,
Actions of Adrenal Medullary Hormones
Epinephrine and norepinephrine mimic the effects of sympathetic nerve discharge, producing the following effects:
- Direct increase in cardiac rate and myocardial force of contraction
- Dilation of coronary and skeletal muscle blood vessels
- Constriction of the cutaneous and visceral vasculature
- Relaxation of respiratory smooth muscle
- Inhibition of GI motility
- Pupillary dilation (mydriasis)
- Glycogenolysis in liver and muscle
- Lipolysis
The catecholamines also elevate the metabolic rate (calorigenic action), stimulate the central nervous system, increase alertness, and stimulate respiration.
Adrenal Cortex
The adrenal cortex develops from the mesoderm during embryonic life. The cells of the adrenal cortex, which are arranged in continuous cords separated by capillaries, are characterized by an abundance of mitochondria, endoplasmic reticulum, and accumulation of lipid.
Mineralocorticoids
These are important in the regulation of electrolyte balance. They control sodium re absorption and secretion of potassium by the kidney tubules. The major hormone of the group is the Aldosterone secreted by the zona glomerulosa.
- Its secretion is regulated primarily by the rennin-angiotensin mechanism. The plasma concentrations of sodium and potassium are involved in the control of aldosterone secretion.
- Hyperkalemia (elevated plasma potassium) exerts a direct stimulating effect on the zona glomerulosa, whereas hyponatremia (low plasma sodium) activates the rennin-angiotensin mechanism.
- Atrial-natriuretic hormone (ANH) inhibits rennin secretion, and it also reduces the responsiveness of the cells in the zona glomerulosa to angiotensin II.
- Aldosterone plays a major physiologic role in the maintenance of electrolyte and fluid balance by promoting the renal tubular reabsorption of sodium and the secretion of potassium and hydrogen.
Glucocorticoids
Control of Secretion and Actions
Glucocorticoid secretion, which occurs primarily in the zona fasciculate, is controlled by ACTH.
A variety of stressful stimuli including; anxiety, fear, hypoglycaemia, hypotension, and haemorrhage, increase secretion of adrenocorticotropic hormone-releasing hormone (CRH) from the hypothalamus.
- Glucocorticoids help the body to respond to unfavorable conditions and promote tissue healing. They maintain blood glucose levels in times of stress by stimulating the liver to convert amino acids into glucose instead of protein.
- They raise the level of other nutrients in blood, including amino acids from tissue proteins and fatty acids from fats stored in adipose tissue. They also have the ability to suppress the inflammatory response and are often administered as medication for this purpose. The major hormone for this group is cortisol also called hydrocortisone.
The Sex Glands
The sex glands, the ovaries of the female and the testes of the male, not only produce the sex cells but are also important endocrine organs.
The hormones produced by these organs are needed in the development of the sexual characteristics, which usually appear in the early teens and for the maintenance of the reproductive apparatus once full development has been attained.
The main androgen produces by the male sex glands, testosterone, is responsible for the growth of and functioning of the male reproductive tract.
Those structures directly concerned with reproduction are considered primary sex characteristics.
Testosterone is also responsible for male secondary sex characteristics such as a deep voice and facial hair.
In the female, the hormones that most nearly parallel testosterone in their actions are the estrogens.
Estrogens contribute to the development of the female secondary sex characteristics and stimulate the development of the mammary glands, the onset of menstruation, and the development and functioning of the reproductive organs.
The other hormone produced by the female sex glands, called progesterone, assists in the normal development of pregnancy.
The Thymus Gland
The thymus gland lies in the upper part of the chest above the heart. Through the production of a hormone called thymosin, it helps in the development of certain white blood cells, called T-lymphocytes that help protect the body against foreign organisms. Because this gland is most active before birth and early in life, it is large during childhood but gradually shrinks in size as one reach adulthood.
The Pineal Gland
The pineal gland, a small, flattened, cone-shaped structure located between the two parts of the thalamus, produces a hormone called melatonin in a number of animals and also in humans. Melatonin, or some other hormone from the pineal, is thought to regulate the release of certain substances from the hypothalamus, which may in turn regulate the secretion of gonadotropins from the pituitary.
There is evidence from animal studies that the production of melatonin is regulated by the amount of light in the environment.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

