Anatomy & Physiology 2
Subtopic:
The Urinary System
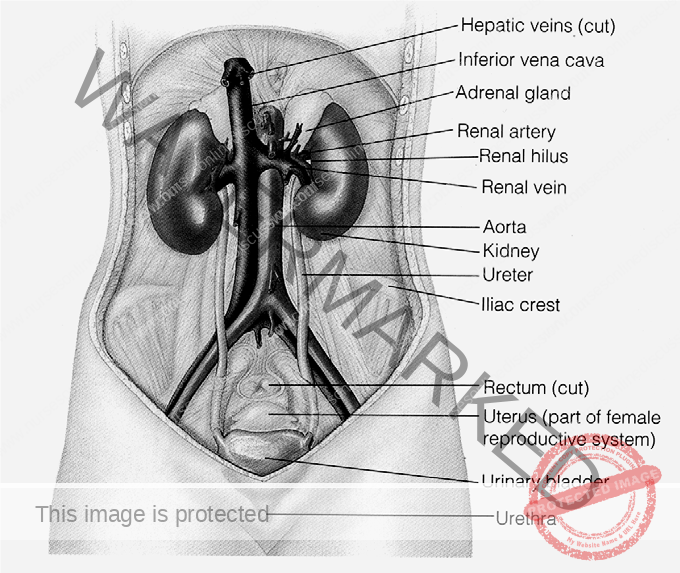
Organs of the urinary system
Major functions of the urinary system:
- Excretion of wastes such as; cellular metabolic wastes, excess salts, and toxins. One product of amino acid metabolism is nitrogen- containing waste material, mainly urea. After synthesis in the liver, urea is transported in blood to the kidneys for elimination.
- Water balance: Although the amount of water gained and lost in a day vary, the kidneys can adapt to these variations by altering urine output so that the volume of body water remains remarkably stable from day to day.
- Acid base balance of body fluids: acids are being constantly produced by cellular metabolism. Certain foods can yield acids or bases, and people can ingest anti acids such as bicarbonate. However, if the body is to function normally it must maintain the pH within normal limits (7.35 to 7.45)
- Blood pressure regulation: the kidneys depend on the blood pressure to filter the blood. If blood pressure fails, potentially limiting the filtration, specialized kidney cells release rennin. This enzyme activates angiotensinogen (protein precursor) from the liver to angiotensin I then to angiotensin II by angiotensin converting enzyme (ACE). ANGIOTENSIN II causes the constriction of blood vessels thus raising the blood pressure.
- Regulation of red blood cells production: when the kidneys do not get enough oxygen, they produce the hormone erythropoietin, which stimulate red cell production in the bone marrow.
External Anatomy of the kidney
- A pair of reddish brown, bean shaped organ located in the posterior wall of the abdominal region, one in each side of the vertebral column. They usually lie between T12 to L3. They are protected at least partially by the last pair of ribs and capped by the adrenal gland. The bean shape of the kidney is medially concave and laterally convex.
- On the medial concave border is the hilus (small indented area) where blood vessels, nerves & ureters enter and leave the kidney.
- Covering and supporting each kidney are three layers of tissue:
- Renal capsule – innermost, tough, fibrous layer
- Adipose capsule – the middle layer composed of fat, giving the kidney protective cushion.
- Renal fascia – is outer sub-serous membrane, connective tissue layer
- The kidneys, ureters, lie posterior to the peritoneum: thus, not in the peritoneal cavity but in an area called the retroperitoneal space.
- Blood supply; blood to the kidney is by a short branch of the abdominal aorta called the renal artery; after entering the kidney, the renal artery subdivides into numerous small branches which eventually make contacts with the kidney’s functional units (nephron). Blood leaves the kidneys by vessels that finally emerge to form the renal vein to the inferior venacava.
Internal Anatomy of the kidney
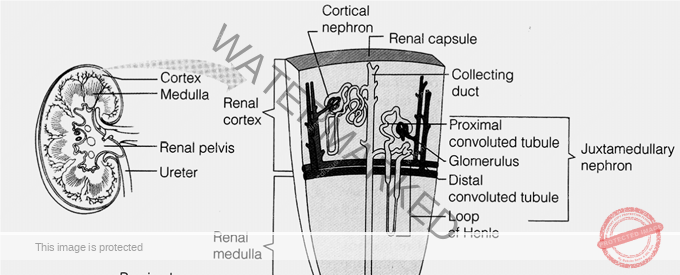
A sagital section of the kidney reveals three distinct regions called pelvis, medulla and cortex (from inside out).
The renal pelvis is the large collecting space within the kidney formed from the expanded upper portion of the ureters. The pelvis branch to two cavities, these are 2-3 major calyces and 8 to 18 minor calyces.
The Renal medulla is the middle portion of the kidney. It consists of 8 to 18 renal pyramids, which are longitudinally striped, one cone shaped area. The base of each pyramid is adjacent to the outer cortex. The apex of each renal pyramid ends in papilla, which opens to a minor calyx. Pyramids contain tubules and collecting ducts of the nephron. Tubules involved in transportation and re-absorption of filtered materials.
The renal cortex is the outermost portion of the kidney. It is divided in to two region the outer cortical and the inner juxtamedullary region. The cortical tissue that penetrates between pyramids forms Renal Columns. The renal columns composed of mainly collecting tubules.
Nerve supply
– By renal plexus of autonomic nervous system.
The nephron
The basic functional unit of the kidney is the nephron. Each nephron is an independent urine-forming unit. Each kidney contains approximately one million nephrons.
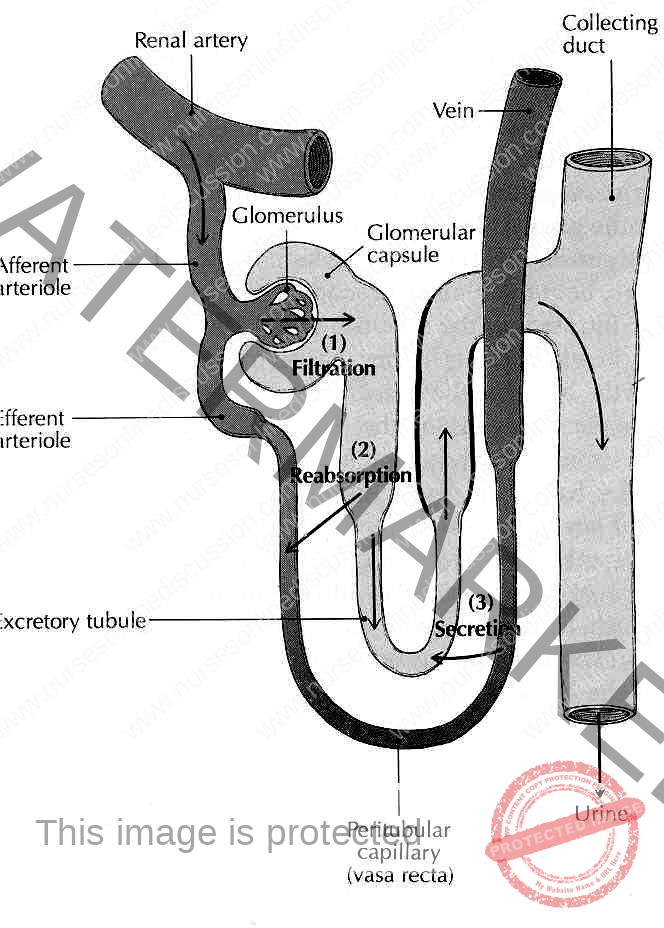
There are two parts of a kidney nephron: the renal corpuscle, and the renal tubule. Renal CorpuscleThe renal corpuscle is the part of the kidney nephron in which blood plasma is filtered. Within the glomerulus are glomerular capillaries that are located between the afferent arteriole bringing blood into the glomerulus and the efferent arteriole draining blood away from the glomerulus. The (outgoing) efferent arteriole has a smaller diameter than the (incoming) afferent arteriole. This difference in arteriole diameters helps to raise the blood pressure in the glomerulus. The area between the double-walls of the Bowman’s Capsule is called the capsular space. The cells that form the outer edges of the glomerulus form close attachments to the cells of the inner surface of the Bowman’s Capsule. This combination of cells adhered to each other forms a filtration membrane that enables water and solutes (substances that are dissolved in the water/blood) to pass through the first wall of the Bowman’s Capsule into the capsular space. This filtration process is helped by the raised blood pressure in the glomerulus – due to the difference in diameter of the afferent and efferent arterioles. SummaryIn the renal corpuscle blood is forced through the glomerular capillaries at higher pressure than the pressure at which the blood generally travels around the body (and also into the kidney itself). Helped by the increased pressure in the glomerular capillaries, a filtration process occurs in which some blood fluid is forced out of the glomerulus and into the capsular space of the Bowman’s Capsule. The fluid that is filtered into the Bowman’s Capsule is called the glomerular filtrate. Renal TubuleThe renal tubule is the part of the kidney nephron into which the glomerular filtrate passes after it has reached the Bowman’s capsule. The first part of the renal tubule is called the proximal convoluted tubule (PCT), which is shown on the right-hand side of the diagram above. The water and solutes that have passed through the proximal convoluted tubule (PCT) enter the Loop of Henle, which consists of two portions – first the descending limb of Henle, then the ascending limb of Henle. In order to pass through the Loop of Henle, the water (and substances dissolved in it) pass from the renal cortex into the renal medulla, and then back to the renal cortex. When this fluid returns to the renal cortex (via the ascending limb of Henle) it passes into the distal convoluted tubule (DCT), which is shown on the left-hand side of the diagram above. The distal convoluted tubules of many individual kidney nephrons converge onto a single collecting duct. The fluid that has passed through the distal convoluted tubules is drained into the collecting duct (far left-hand-side of the diagram above). Many collecting ducts join together to form several hundred papillary ducts. There are typically about 30 papillary ducts per renal papilla (the renal papillae being the tips of the renal pyramids – which point towards the centre of the kidney). At each renal papilla the contents of the papillary ducts drain into the minor calyces – the channels through which the fluid passes, via the major calyx, into the centre of the kidney – called the renal pelvis. |
The processes in urine formation are: -
Average Comparison of filtration, re-absorption and excretion, here variation in urine composition will occur during variation in the daily diet, fluid intake, weather and exercise.
Urine may be a waste product, but it is a carefully created waste product. There are three main stages in urine formation.
- Blood filtration, every day the kidneys filter 1700 Liter of blood
- Tubular re-absorption
- Tubular secretion.
Urine is one of the body’s waste products. It is primarily composed of water and urea. Urea is a special nitrogenous waste compound that the body must routinely remove. Urine formation occurs in the kidney in three stages: filtration, reabsorption, and secretion.
Filtration: From Blood to Kidney
The kidney is the body’s blood filtering
system. Blood vessels visit the kidney and enter a special ball of capillaries
called the glomerulus. The glomerulus is nestled within a region of the
kidney called the Bowman’s capsule. This is where filtration occurs.
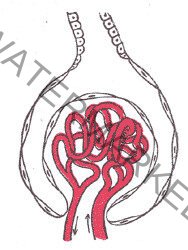
The ball of blood vessels (glomerulus) inside the Bowman’s capsule of the kidney
As blood is pushed through the tiny capillaries, the high-pressure forces some things to pass through the capillary walls. The walls act as a sieve or a filter. Hence, it is called filtration.
Water, sugar, salts, amino acids, nitrogenous wastes, and other tiny things enter the kidney as a substance called the filtrate. Blood Cells, drugs and large blood proteins that cannot fit through remain in the blood vessels. The filtrate entering the kidney is like pre-pre-urine.
Reabsorption: From Kidney Back to Body
The filtrate enters the kidney in the proximal tubule. This region of the kidney is special because many things can be removed from the filtrate. These valuable things are recollected, or reabsorbed, by the body.
Glucose, certain salts, vitamins, hormones, and amino acids are restored to the body and will not be included in urine. Sometimes, if the body has too much of something then the extra sugar or salt will stay in the filtrate. For example, diabetics with high levels of blood glucose may have glucose in their urine since it cannot all be reabsorbed.
The filtrate after reabsorption is like pre- urine
Secretion: From Body Straight to Urine
The filtrate then passes through a really neat structure called the Loop of Henle where it gains and losses water and salt. As it leaves the Loop of Henle, it enters the distal tubule. Here the final process of urine formation occurs: secretion.
Summary:
- Glumerular filtration moves water and salutes from the blood into the nephron.
- Tubular reabsorption moves useful substances back into the blood while keeping waste products in the nephron to be eliminated in the urine.
- Tubular secretion moves additional substances from the blood into the nephron for elimination. Movement of hydrogen ions is one means by which the pH of body fluids is balanced.
- The countercurrent mechanism concentrates the urine and reduces the volume excreted. The pituitary hormone ADH allows more water to be reabsorbed from the nephron.
Accessory Excretory structures
Urine is formed in the kidney, but accessory structures are required to transfer, store and eventually eliminate urine from the body. These structures are the two ureters, urinary bladder and urethra.
Ureters
Attached to each kidney is a tube called the ureter. Ureters transport urine from the renal pelvis to the urinary bladder.
The ureters pass between the parietal peritoneum and the body wall to the pelvic cavity, where they enter the pelvic cavity. It is narrow at the kidney and widen near the bladder.
The lumen of the ureters is composed of three layers:
– Innermost, Tunica Mucosa
– The middle, Tunica Muscularis (made of smooth muscle)
– The outer, Tunica Adventitia
Urinary bladder
Urinary bladder is a hollow, muscular organ that collects urine from the ureters and store until it is excreted. It usually accumulates 300 to 400 m.l. of urine but it can expand as much twice. It is located on the floor of the pelvic cavity and like the kidneys and ureters.
It is Retroperitoneal. In males it is anterior to the rectum and above the prostate gland. In females, it is located somewhat lower, anterior to the uterus and upper vagina.
The wall of urinary bladder is composed of three layers:
- Tunica mucosa, the innermost layer lined with transitional epithelium.
- Tunica muscularis, the middle layer, three layers of smooth muscle. This collectively called deterusor muscles.
- Tunica serosa (Adventitia), the outer layer derived from peritoneum and covers only the upper and lateral surfaces of the bladder.
The opening of ureters and urethra in the cavity of the bladder outline triangular area called the trigone. At the site where the urethra leaves the bladder, the smooth muscle in the wall of the bladder forms spiral, longitudinal and circular bundles which contract to prevent the bladder from emptying prematurely.
These bundles function as a sphincter called Internal Urethral Sphincter (Involuntary). along the urethra in the middle membranous portion is a circular sphincter of voluntary skeletal muscle which form the external urethral sphincter.
Urethra
Urethra is a tube of smooth muscle lined with mucosal layer. It joins the bladder at its inferior surface and transport urine outside the body during urination. It is 4cm in female and 12cm. in length in male.
In females it opens between vagina and clitoris. In male it passes through prostate, membranous portion (pelvic diaphragm muscle), spongy portion and open at the tip of penis. The spongy portion joined by ducts from bulbo-uretheral gland (Mucus secreting gland).
Urine & urination
Composition of urine varies depending on the diet, exercise, water consumption and other factors. However, it is composed of mainly water, urea, chloride, potassium, sodium,
creatinine, phosphate, sulfates and uric acid. Proteins, glucose, casts (decomposed blood) and calculi from minerals are abnormal if present in urine. The PH of urine is 5.0 to 8.0 (mostly acidic) and has translucent (clear, not cloudy) color.
To maintain the proper osmotic concentration of the extra cellular fluid to excrete wastes and to maintain proper kidney function the body must excrete at least 450ml of urine per day. A healthy person excretes 1000 to 1800 ml of urine daily. The volume and concentration of urine is controlled by:
– Antidiuretic hormone
– Aldestrone
– The Renin – angiotensin mechanism
Urination
Urination is emptying of the bladder; it is the process of conscious and unconscious nerve control. Steps of urination are:
- Conscious desire to urinate
- Pelvic diaphragm muscle relaxes
- Urinary bladder neck Moves down, outlet Opens, wall stretch,
- and wall stretch receptors are stimulated
- Smooth muscle of the urinary bladder Contracts & urine ejects.
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved Design & Developed by Opensigma.co

