Conditions Affecting the Endocrine System
Subtopic:
Thyrotoxicosis
Table of Contents
Learning Objectives
Define thyrotoxicosis and distinguish it from hyperthyroidism.
Describe the anatomy and hormonal functions of the thyroid gland.
Identify common causes of thyrotoxicosis, including Graves’ disease and toxic nodules.
Explain the systemic effects of excess thyroid hormones on metabolism and organ function.
Recognize clinical signs and symptoms of thyrotoxicosis, such as weight loss and tachycardia.
Thyrotoxicosis and Related Terms
Thyrotoxicosis: This is the overarching term for a clinical condition resulting from an excess of thyroid hormones in the body, regardless of the origin. It encompasses situations where thyroid hormone levels are elevated due to any cause. Therefore, it is a broader category that includes hyperthyroidism.
Hyperthyroidism: Specifically refers to the condition where the thyroid gland itself is overproducing thyroid hormones. This is a cause of thyrotoxicosis.
Interchangeable Use: It’s worth noting that in common medical language, the terms “thyrotoxicosis” and “hyperthyroidism” are sometimes used synonymously, although technically, thyrotoxicosis is the more encompassing term.
Overactive Thyroid: This is a general, informal way to describe hyperthyroidism. Medically, it is also known as hyperthyreosis.
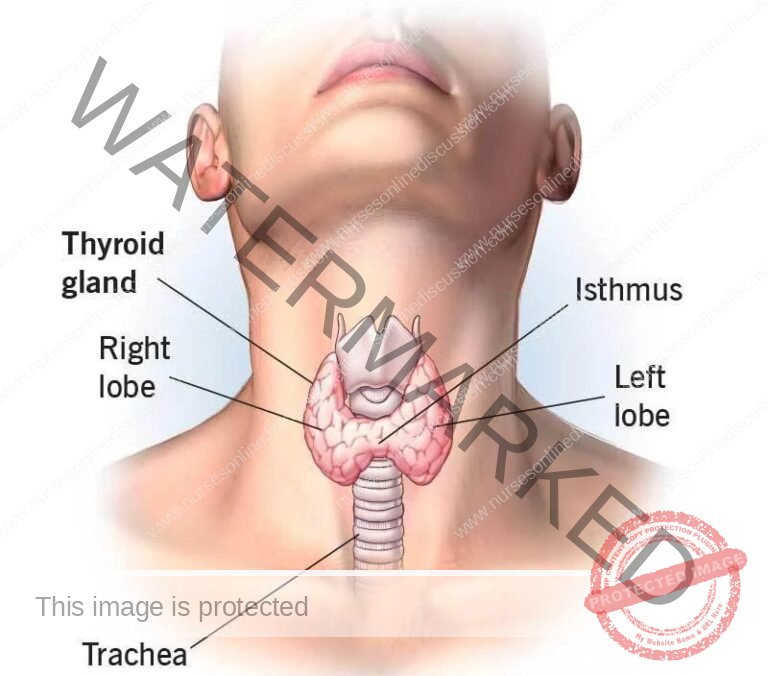
Anatomy of the Thyroid Gland
Location: Situated in the anterior aspect of the lower neck, the thyroid gland is positioned in front of the voice box (larynx) and windpipe (trachea). It lies approximately at the level of the fifth, sixth, and seventh cervical vertebrae and the first thoracic vertebra in the spinal column.
Structure and Appearance: This gland is characterized by a rich blood supply (highly vascular) and typically weighs around 25 grams. Its shape is often likened to a butterfly.
Lobes and Isthmus: The thyroid is composed of two main sections, called lobes, located on each side of the trachea. These lobes are connected in the midline by a narrow band of tissue known as the isthmus, which crosses in front of the trachea.
Primary Functions: The thyroid gland’s essential role is the production of thyroid hormones. These include:
Triiodothyronine (T3) and Thyroxine (T4): These hormones are crucial for regulating the body’s metabolism, influencing how energy is used.
Calcitonin: A hormone involved in calcium regulation within the body.
Overall, thyroid hormones are fundamental for normal growth and for the control of metabolic rate across various bodily functions.
Common Terms
a. Hyperthyroidism: This condition arises when the thyroid gland becomes overactive and produces an excessive amount of thyroid hormones. This hormonal surge speeds up the body’s metabolism, leading to symptoms like unexplained weight loss, a rapid or irregular heartbeat, increased irritability, intolerance to heat, and tremors.
b. Thyrotoxicosis: This term describes the clinical state resulting from having too much thyroid hormone circulating in the bloodstream, regardless of the source. While hyperthyroidism (overproduction by the thyroid) is a common cause, thyrotoxicosis can also occur due to thyroid gland inflammation or taking excessive thyroid hormone medication. The signs and symptoms are generally similar to those of hyperthyroidism.
c. Graves’ Disease: An autoimmune disorder and the most frequent cause of hyperthyroidism. In Graves’ disease, the body’s immune system mistakenly targets the thyroid gland. This immune attack causes the thyroid to overproduce thyroid hormones. Hallmark symptoms often include goiter (thyroid gland enlargement), exophthalmos (protruding eyes), unintentional weight loss, tremors, and heat sensitivity.
d. Hypothyroidism: This condition indicates an underactive thyroid gland, meaning it doesn’t produce enough thyroid hormones. The resulting hormone deficiency slows down the body’s metabolic processes. Common symptoms include persistent fatigue, unexplained weight gain, cold intolerance, constipation, and feelings of depression.
e. Cretinism: This term refers to a condition caused by severe hypothyroidism present from birth or developing in early infancy and left untreated. It leads to significant impairments in physical and mental development, including stunted growth, intellectual disability, and various developmental delays. Causes can include iodine deficiency during pregnancy, thyroid gland malformations, or genetic factors.
f. Myxedema: This is the term for severe hypothyroidism in adults. It’s characterized by the buildup of mucopolysaccharides in connective tissues throughout the body. This accumulation causes swelling and thickening of the skin, particularly noticeable in the face and lower legs. Key symptoms include extreme fatigue, pronounced cold intolerance, weight increase, dry skin, hair thinning, and slowed mental function.
g. Goiter: A goiter is simply an enlargement of the thyroid gland. It typically appears as a visible swelling at the front of the neck. Goiters can develop for various reasons, including iodine deficiency, thyroid gland inflammation, and thyroid disorders such as Graves’ disease and Hashimoto’s thyroiditis.
h. Hashimoto’s Thyroiditis: This is an autoimmune disease that affects the thyroid gland. In Hashimoto’s, the immune system mistakenly attacks the thyroid. This ongoing immune assault leads to chronic inflammation and damage to the thyroid gland, frequently resulting in hypothyroidism (underactive thyroid).
i. Thyroid Storm: Also known as thyrotoxic crisis, thyroid storm is a life-threatening medical emergency. It represents a sudden and dramatic worsening of hyperthyroidism symptoms. It typically occurs in individuals with untreated or inadequately managed hyperthyroidism, often triggered by a stressful event. Key signs are high fever, severe agitation or delirium, a dangerously rapid heartbeat, elevated blood pressure, vomiting, diarrhea, and jaundice. Thyroid storm necessitates urgent medical intervention and hospitalization to stabilize the patient and prevent fatal outcomes. Treatment involves medications to block thyroid hormone production and release, along with intensive supportive care.
Why we need the Thyroid Gland & Hormones
Regulation of Metabolism: The thyroid gland plays a central role in regulating metabolism, influencing the rate at which cells convert nutrients into energy. It does so by producing and releasing thyroid hormones (triiodothyronine or T3 and thyroxine or T4), which control the body’s metabolic processes.
Body Temperature Control: Thyroid hormones help regulate body temperature by influencing heat production and heat loss mechanisms. They help maintain the body’s core temperature within a normal range.
Growth and Development: Thyroid hormones are important for proper growth and development in children. They are essential for the normal development of the skeletal system, brain, and other organs. Insufficient thyroid hormone production can lead to growth and developmental delays.
Brain Function: Thyroid hormones are necessary for the normal functioning of the brain. They play a role in cognitive function, mood regulation, memory, and overall mental well-being.
Energy Levels: Thyroid hormones contribute to energy production in the body. They help convert food into usable energy, ensuring adequate energy levels for daily activities.
Heart Function: Thyroid hormones have an impact on heart rate, heart rhythm, and cardiac output. They help regulate the overall function of the cardiovascular system.
Muscle Function: Thyroid hormones are involved in maintaining muscle tone and strength. They contribute to muscle contraction and overall muscle function.
Digestion: Proper thyroid function is necessary for healthy digestion. Thyroid hormones influence the movement of food through the digestive tract and the secretion of digestive enzymes.
Reproductive Health: Thyroid hormones play a role in reproductive health, including menstrual cycle regulation in women. Thyroid disorders can affect fertility, pregnancy outcomes, and the health of the developing fetus.
Maintenance of Healthy Skin, Hair, and Nails: Optimal thyroid function is important for maintaining healthy skin, hair, and nails. Thyroid hormones contribute to the growth, maintenance, and integrity of these structures.
Causes of Hyperthyroidism and/or Thyrotoxicosis
Graves’ Disease: This autoimmune disorder is the most frequent cause of hyperthyroidism globally, accounting for a large majority of cases (50-80%). Its occurrence is often related to varying levels of iodine in one’s diet. Graves’ disease is significantly more common in women, affecting them roughly eight times as often as men, with typical diagnosis occurring in younger women between 20 and 40 years old.
Toxic Thyroid Nodule (Adenoma): Notably prevalent in areas like Switzerland (around 53% of cases there), this cause is thought to be more common due to historically lower iodine intake in the population. It involves a single, overactive benign growth (adenoma) within the thyroid gland that produces excessive hormones.
Toxic Multinodular Goiter: This condition is marked by the presence of multiple nodules throughout the thyroid gland. These nodules independently become overactive, collectively leading to an overproduction of thyroid hormones.
Thyroid Inflammation (Thyroiditis): Inflammation of the thyroid gland, known as thyroiditis, can take forms like Hashimoto’s thyroiditis (primarily causing underactive thyroid but can have a temporary hyperthyroid phase initially) and subacute thyroiditis (de Quervain’s thyroiditis). Initially, these conditions can result in a temporary release of excess thyroid hormone, but they often progress to thyroid gland damage and ultimately lead to reduced thyroid function (hypothyroidism).
Medications and External Thyroid Hormone Intake: Hyperthyroidism can arise from taking too many thyroid hormone pills or, in rare instances, from consuming contaminated meat products containing thyroid tissue. The medication amiodarone, used for heart rhythm problems, is also known to potentially disrupt thyroid function, causing either underactivity or overactivity.
Postpartum Thyroiditis (PPT): This condition affects approximately 7% of women following childbirth. PPT progresses through different phases, with an initial hyperthyroid phase. In most cases, PPT resolves on its own without specific treatment.
Struma Ovarii: A very uncommon type of tumor (specifically, a monodermal teratoma) in the ovary, where the tumor tissue is primarily thyroid tissue. This thyroid tissue can function and produce thyroid hormones, leading to hyperthyroidism.
Excessive Iodine Intake: Consuming too much iodine, especially from sources like kelp and other algae-based supplements, can sometimes trigger or worsen hyperthyroidism.
Overuse of Thyroid Hormone Supplements: Taking too high a dose of thyroid hormone replacement medication, such as levothyroxine, can result in thyrotoxicosis (excess thyroid hormone in the body).
Pituitary Adenoma (TSH-secreting): In very rare instances (less than 1% of cases), hyperthyroidism is caused by a pituitary gland tumor (adenoma) that secretes excessive thyroid-stimulating hormone (TSH). This excess TSH then overstimulates the thyroid gland to produce too much thyroid hormone.
General Causes of Thyroid Conditions
Autoimmune Conditions: Disorders where the body’s defense system mistakenly attacks the thyroid are major contributors to thyroid issues. For instance, in Hashimoto’s thyroiditis, the immune system damages the thyroid, leading to underactive thyroid function (hypothyroidism). Conversely, Graves’ disease involves the immune system stimulating the thyroid, causing it to overproduce hormones and resulting in overactive thyroid function (hyperthyroidism).
Iodine Imbalance: Iodine is essential for the thyroid to create its hormones. Both too little and too much iodine can cause problems. Iodine deficiency can lead to hypothyroidism and goiter (thyroid enlargement). Excessive iodine, while less common, can also disrupt thyroid function and sometimes trigger hyperthyroidism. Public health initiatives like iodized salt help ensure sufficient iodine intake in populations.
Thyroid Growths (Nodules): Lumps or abnormal tissue growths within the thyroid gland are called nodules. These can be non-cancerous (benign) or cancerous (malignant). Nodules can cause issues by altering hormone production or by pressing on nearby structures in the neck, potentially requiring medical attention depending on their nature and symptoms.
Medications and Medical Treatments: Certain drugs and therapies can negatively affect thyroid function. For example, lithium, used for mood disorders, is known to sometimes cause thyroid problems, including both hypothyroidism and hyperthyroidism. Radiation treatment to the head or neck area, often used for cancer therapy, can also damage the thyroid gland and impair its function.
Congenital Issues: Some individuals are born with thyroid problems. Congenital hypothyroidism occurs when a baby’s thyroid gland doesn’t develop properly or is missing at birth. This results in insufficient thyroid hormone production from infancy. Early detection and treatment are crucial in newborns to prevent developmental delays and growth issues.
Genetic Predisposition: A person’s genes can increase their likelihood of developing thyroid conditions. Specific genetic mutations or a family history of thyroid disorders can make individuals more susceptible to conditions such as thyroid cancer or autoimmune thyroid diseases.
Inflammation and Infection: Inflammation of the thyroid gland, termed thyroiditis, can disrupt its normal operation. Viral or bacterial infections can also affect the thyroid, potentially leading to various thyroid problems and functional changes.
Signs and Symptoms of Thyrotoxicosis
Thyroid hormones are vital for regulating cellular function. When these hormones are present in excessive amounts, they not only boost metabolism beyond normal levels but also amplify the effects of the sympathetic nervous system. This over-activity results in an accelerated pace of various bodily functions, often mimicking the effects of an adrenaline surge. Hyperthyroidism can present with a wide spectrum of symptoms; some individuals may show no noticeable signs, while others can experience significant clinical manifestations.
Symptoms:
Nervousness: Elevated thyroid hormones overstimulate the nervous system, causing heightened sensitivity and pronounced feelings of unease.
Irritability: The sympathetic nervous system’s hyperactivity can lead to increased agitation and a tendency to become easily frustrated.
Increased Sweating: A faster metabolism generates more heat, leading to increased sweat production as the body attempts to regulate its temperature.
Rapid Heartbeat: Excess thyroid hormones can accelerate the heart rate, causing palpitations or the sensation of a racing heart.
Tremors: The stimulated nervous system and elevated metabolic rate can contribute to involuntary trembling, particularly noticeable in the hands.
Anxiety: High levels of thyroid hormones can induce a persistent state of worry, tension, and apprehension.
Sleep Disturbance: Hyperthyroidism can disrupt regular sleep cycles, often resulting in difficulty falling asleep or staying asleep (insomnia).
Skin Thinning: The accelerated metabolic rate can affect the skin’s texture and thickness, potentially leading to a noticeable thinning.
Brittle Hair: Hormonal imbalances associated with thyrotoxicosis can negatively impact hair health, making it fine and prone to breakage.
Muscle Weakness: Thyroid hormones play a role in muscle function. Excessive levels can lead to muscle fatigue and weakness, particularly in the upper arms and legs.
Frequent Bowel Movements: An increased metabolic rate speeds up digestion, which can result in more frequent bowel movements and sometimes diarrhea.
Unintentional Weight Loss: Despite an often increased appetite, the body burns calories at a faster rate due to elevated metabolism, leading to weight loss.
Nausea and Vomiting: Digestive system disturbances, including increased stomach activity, can cause feelings of nausea and instances of vomiting.
Menstrual Changes: Altered hormone levels can disrupt the menstrual cycle in women, potentially causing lighter menstrual flow or longer intervals between periods.
Major Clinical Signs:
- Weight loss: Accelerated metabolism and increased calorie consumption contribute to weight loss.
- Anxiety: Overstimulation of the nervous system manifests as heightened anxiety.
- Heat intolerance: Elevated metabolism generates more internal heat, causing intolerance to warm environments.
- Hair loss: Changes in hormone levels impact hair follicles, resulting in hair loss, particularly in the outer third of the eyebrows.
- Muscle aches: Thyroid hormones influence muscle function, leading to aches and weakness.
- Weakness: Muscular weakness is a common symptom of hyperthyroidism.
- Fatigue: Despite increased activity, individuals may experience fatigue due to the strain on the body.
- Hyperactivity: Elevated metabolism and increased energy levels contribute to hyperactivity.
- Irritability: Overstimulation of the nervous system can lead to irritability.
- High blood sugar: Thyroid hormones can impact glucose metabolism, leading to elevated blood sugar levels.
- Excessive urination: Altered kidney function due to hormone imbalances can result in increased urination.
- Excessive thirst: Increased fluid loss through urine may lead to excessive thirst.
- Delirium: Severe cases of hyperthyroidism can cause mental confusion and delirium.Tremor: Increased nervous system activity may manifest as tremors in various parts of the body.
- Pretibial myxedema: Specific to Graves’ disease, it involves skin changes, swelling, and redness on the shins.
- Emotional lability: Mood swings and emotional instability can occur due to hormonal fluctuations.
- Sweating: Excessive sweating is a common symptom of hyperthyroidism.
- Panic attacks: The combination of heightened nervous system activity and anxiety can lead to panic attacks.
- Inability to concentrate and memory problems: Cognitive functions may be affected, leading to difficulties in concentration and memory.
Physical Symptoms
- Palpitations: Increased heart rate and irregular heart rhythms may cause palpitations.
- Abnormal heart rhythms: Hyperthyroidism can disrupt normal heart rhythms, notably causing atrial fibrillation.
- Shortness of breath: Respiratory and cardiovascular effects may result in shortness of breath (dyspnea).
- Loss of libido: Hormonal imbalances can impact sexual desire and lead to a loss of libido.
- Gynecomastia and feminization: Altered hormone levels may cause breast enlargement (gynecomastia) and feminine characteristics in males.
Note:
- An association between thyroid disease and myasthenia gravis has been recognized, with approximately 5% of patients with myasthenia gravis also having hyperthyroidism.
- In Graves’ disease, ophthalmopathy may cause enlarged eyes due to swelling eye muscles pushing the eyes forward, often with one or both eyes bulging.
- Swelling of the front of the neck (goiter) may also occur.

Minor Ocular Signs
- Eyelid retraction (“stare”): Overactive thyroid hormones can affect the muscles that control eyelid movement, leading to a wide-eyed or “staring” appearance.
- Extraocular muscle weakness: Weakness in the muscles that control eye movement may result in difficulties in moving the eyes.
- Lid-lag (von Graefe’s sign): A characteristic eye movement sign where the upper eyelid lags behind the downward movement of the eye.
- Double vision: Weakened eye muscles may cause double vision.
Exophthalmos/Proptosis in Graves’ Disease:
Exophthalmos or proptosis, the protrusion of the eyeball, is unique to hyperthyroidism caused by Graves’ disease. It results from immune-mediated inflammation in the retro-orbital fat, leading to forward protrusion of the eyes.
Exophthalmos, when present with hyperthyroidism, is diagnostic of Graves’ disease.
Diagnosis and Investigation
Physical examination: enlarged, bumpy or tender gland through the neck, Eyes for swelling, redness or bulging, Heart for for a rapid heartbeat and irregular heartbeats, Hands for tremors, Skin if its moist and warm.
Blood Tests
- The Thyroid Stimulating Hormone (TSH) Test measures TSH levels, a hormone from the pituitary gland that stimulates the thyroid. Abnormal levels may indicate hyperthyroidism or hypothyroidism.
- Thyroid Hormone (T3 and T4) Tests evaluate T3 and T4 hormone levels. Elevated levels may suggest hyperthyroidism, while decreased levels may indicate hypothyroidism.
- Thyroid Antibody Tests check for antibodies linked to autoimmune thyroid disorders like Hashimoto’s thyroiditis or Graves’ disease.
- Thyroid Function Panel combines TSH, T3, and T4 tests for a comprehensive thyroid function assessment.
Imaging Studies
- Ultrasound uses sound waves to create thyroid gland images, aiding in identifying nodules, goiter, or structural abnormalities.
- Thyroid Scan utilizes radioactive tracers to assess overall thyroid structure and function.
- Radioactive uptake study i.e. For this test, a small, safe dose of radioactive iodine (also called a radiotracer) is taken by mouth to see how much of it your thyroid gland absorbs. After 6 to 24 hours later, the neck is scanned with a device called a gamma probe to see how much of the radioactive iodine your thyroid has absorbed. If your it absorbs a lot, it means that your thyroid gland is producing too much thyroxine (T4)
- Fine-Needle Aspiration (FNA) Biopsy:
In cases of suspicious thyroid nodules or potential cancer, FNA Biopsy extracts a sample for laboratory analysis. - Thyroid Imaging:
Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) assess the thyroid and adjacent structures when further evaluation is needed.
Medical Management of Hyperthyroidism
Antithyroid Medications:
Propylthiouracil (PTU):
Typical adult dosage: 100-150 mg, administered three times daily.
Potential side effects: Risk of liver damage, skin rash, joint discomfort, and a rare but serious blood disorder called agranulocytosis (marked by a significant decrease in white blood cells).
Methimazole (Tapazole):
Standard adult dosage: 10-30 mg, given once daily or divided into two doses across the day.
Possible side effects: Skin reactions like rash and itching, nausea, and the potential for agranulocytosis.
Beta-Blockers:
These medications are used to manage symptoms associated with hyperthyroidism, such as elevated heart rate, tremors, and anxiety.
Common examples include propranolol and atenolol.
Adult dosages are variable depending on individual needs.
Possible side effects: May include tiredness, lightheadedness, and reduced blood pressure.
Radioactive Iodine (RAI) Therapy:
Administered orally as a capsule or liquid.
The purpose is to reduce the activity or destroy overactive thyroid tissue.
Potential short-term side effects: Possible temporary increase in hyperthyroidism symptoms, neck discomfort, and symptoms resembling radiation sickness (nausea, fatigue).
Management of Thyrotoxicosis
Treatment Goals:
Reduce Thyroid Gland Activity: Aim to decrease the excessive hormone production by the thyroid.
Control Heart Rate: Manage rapid heart rate (tachycardia) and elevated blood pressure (hypertension) often associated with thyrotoxicosis.
Partial Thyroidectomy (Surgical Removal): In some cases, surgical intervention to remove a portion of the thyroid gland may be necessary.
Pre-operative Management:
Hospital Admission: Typically, patients are admitted to the surgical unit approximately 3-2 days before the scheduled surgery.
Patient Positioning: Ensure the patient is in a comfortable position, accommodating their preference.
Comprehensive History Collection: Detailed patient history is taken to gather crucial information, including:
Demographic Information: Basic personal details.
Prior Health Issues: Past medical conditions.
Current Medical Status: Presence of conditions like diabetes or liver disease.
Family Health Background: History of conditions such as hypertension within the family.
Current Health Complaint: Detailed history to identify the underlying cause of the thyrotoxicosis.
Clinical Observations:
Vital Signs Assessment: Regular monitoring of temperature, pulse, respiration (TPR), and blood pressure (BP) to detect any vital sign abnormalities.
General Physical Examination: A thorough head-to-toe examination to identify any general abnormalities (using a systematic approach like JACCOLD – Jaundice, Anemia, Cyanosis, Clubbing, Oedema, Lymphadenopathy, Dehydration).
Specific Thyroid Examination: Palpation of the thyroid gland to assess for enlargement or any unusual characteristics.
Physician Consultation: Inform the physician about the patient’s condition and initial findings.
Pre-Doctor’s Visit Actions: While waiting for the physician, orient the patient to the ward environment and routine.
Medical Investigations: Upon arrival, the doctor will order necessary diagnostic tests, which may include:
Chest X-ray: To assess the lungs and mediastinum.
Thyroid Function Tests (TFTs): Blood tests to measure thyroid hormone levels.
Thyroid Biopsy: Tissue sample taken for cytological and histological examination to rule out malignancy and assess thyroid tissue.
Indirect Laryngoscopy: Examination of the larynx using a mirror to assess vocal cord function, especially important before thyroid surgery to evaluate recurrent laryngeal nerve function.
Preoperative Medications:
Based on lab results, particularly thyroid function tests, the physician will prescribe preoperative medications, which may include:
Carbimazole: 10-15 mg once daily for 12 weeks, then reduced to 5 mg every 8 hours. The last dose is given shortly before surgery. Carbimazole helps to reduce thyroid hormone levels before surgery.
Lugol’s Iodine: 0.3-0.9ml three times a day in milk, given for 10 days leading up to surgery, including the day of surgery. Lugol’s iodine helps to reduce the vascularity of the thyroid gland, minimizing bleeding during surgery.
Propranolol: 40-80 mg every 12 hours if blood pressure is elevated. Propranolol is a beta-blocker used to control heart rate and blood pressure.
Diazepam: 5mg twice daily to help calm and sedate the patient before surgery, reducing anxiety.
Digoxin: 0.25mg once daily if atrial fibrillation (irregular heart rhythm) is detected. Digoxin is used to control heart rate in atrial fibrillation.
Pre-Surgical Nursing Care:
Procedure Explanation and Consent: Explain the surgical procedure, its benefits, and expected outcomes to the patient. Obtain informed consent by ensuring the consent form is signed after the patient understands the information.
Reassurance: Provide emotional support and reassurance to alleviate patient anxiety.
Consent Form Handling: Ensure the informed consent form is properly signed and documented.
Patient Preparation: Prepare the patient for surgery:
Clean the patient as needed.
Dress the patient in a surgical gown.
Blood Sample Collection: Obtain a blood sample for hemoglobin estimation and blood group determination in case transfusion is needed.
Surgical Site Preparation: Inspect and clean the surgical site (neck area) if specifically instructed by the surgeon.
Theater Notification: Inform the operating theater staff about the patient’s readiness for surgery.
Patient Transfer to Theater: Transfer the patient to the operating theater for the procedure.
Surgical Procedure: In the operating theater, a partial thyroidectomy (removal of part of the thyroid gland) is performed.
Recovery Room Transfer: After surgery, the patient is transferred to the recovery room for immediate post-operative monitoring.
Ward Staff Notification: Ward nurses are notified to prepare for the patient’s return to the ward from the recovery room.
MANAGEMENT: POST-THYROIDECTOMY (In Case of Surgery)
Post-Operative Patient Reception:
Nurse Team Mobilization: Upon notification from the operating theater nurse, two nurses should go to the recovery room to receive the patient.
Initial Vital Signs Assessment: Immediately upon receiving the patient, assess vital signs, particularly respiratory rate and pulse, to confirm patient stability.
Ward Transfer and Bed Preparation: Transfer the patient back to the ward and place them in a prepared post-operative bed. Obtain and follow any specific post-operative instructions from the theater staff.
Positioning: Position the patient in the recovery position (usually lateral or semi-prone) to maintain airway and prevent aspiration.
Frequent Observations: Monitor vital signs frequently: every 15 minutes for the first hour, then every 30 minutes for the next hour, followed by hourly checks until the patient is fully recovered and stable.
Post-Operative Medications:
The physician will prescribe post-operative medications as needed. Common examples include:
Analgesics for Pain Relief:
Pethidine: 50mg-100mg via intramuscular injection (IM) up to 3 doses for initial pain management, followed by…
Tramadol: 100mg intravenously (IV) three times a day for 7 days for ongoing pain relief.
Sedatives:
Diazepam: 10-15mg as needed for sedation and anxiety relief.
Specific Post-Thyroidectomy Nursing Care:
Drainage Tube Management:
Tube Removal: Drainage tubes are typically removed within 48 hours post-operation, based on the volume and nature of drainage, and as per doctor’s orders.
Wound Care:
Dressing Changes: Change wound dressings whenever they become soiled to maintain wound cleanliness and prevent infection.
Suture Removal:
Timing: Sutures are usually removed on the 3rd or 4th post-operative day, only upon the doctor’s instruction and assessment of wound healing.
Drainage Management: Ensure continuous drainage into a drainage bottle or maintain a sterile dressing if drainage is minimal.
Respiratory Monitoring and Intervention:
Intubation Readiness: Be prepared for potential intubation if respiratory distress due to laryngeal edema (swelling) occurs.
Hemorrhage Monitoring:
Close Observation: Vigilantly monitor for signs of hemorrhage at the surgical site and systemically (vital signs, patient condition).
Environmental Comfort and Rest:
Calm Environment: Create a quiet and peaceful environment to promote rest.
Sleep Aids: Administer prescribed sedatives or sleep-promoting medications if needed to encourage sleep.
Drain and Suture Care:
Drain Management: Change drainage collection systems every 24 hours or as per protocol.
Suture Care: As mentioned, sutures are removed around the 3rd or 4th day upon doctor’s order.
Neck Movement Restriction:
Minimize Movement: Encourage the patient to minimize neck movements to reduce pain and strain on the surgical site.
Pain Management:
Analgesic Administration: Regularly administer prescribed analgesics to effectively manage post-operative pain.
Vital Signs Monitoring for Complications:
Frequency: Monitor vital signs every 2 hours to promptly detect potential complications such as thyroid storm or surgical site infections.
Antibiotic Administration:
Ceftriaxone: Administer prescribed antibiotics like ceftriaxone 2g every 24 hours to prevent or treat infections.
Dietary Management:
High-Calorie Diet: Order a high-calorie diet to meet increased metabolic needs, satisfy hunger, and prevent tissue breakdown.
Nutrient-Rich Foods: Encourage milk intake initially, followed by a diet rich in carbohydrates, and snacks high in protein, minerals, and vitamins, particularly vitamins A, B6, and C, to support healing.
Daily Nursing Care:
Hygiene: Provide daily oral care and skin care to maintain patient hygiene and comfort.
Elimination: Monitor and manage bowel and bladder function.
Physiotherapy:
Throat and Respiratory Exercises: Encourage gentle throat exercises and deep breathing and coughing exercises to prevent respiratory complications and stiffness.
Psychological Support (Psychotherapy):
Offer emotional and psychological support to address anxiety and promote mental well-being during recovery.
Fluid Balance Monitoring:
Intake and Output Tracking: Strictly monitor, maintain, and record fluid intake and output on patient fluid balance charts to ensure adequate hydration and detect any fluid imbalances.
Nursing Interventions
Thyroid Status Assessment: Regularly check thyroid hormone levels and observe for related symptoms. This helps in evaluating treatment effectiveness and spotting any shifts in thyroid function.
Medication Delivery: Give prescribed thyroid medications (like hormone replacement or antithyroid drugs) precisely. Pay close attention to correct dosage, timing, and method of administration.
Patient and Family Education: Thoroughly educate patients and their families about their thyroid condition. Cover the specifics of the illness, the treatment strategy, medication details, and possible side effects.
Vital Signs Monitoring: Frequently check vital signs such as heart rate, blood pressure, and body temperature. This helps assess the impact of thyroid issues and the effects of medication.
Emotional Support: Offer emotional support and foster a supportive environment. This aids patients in managing the emotional and psychological challenges associated with thyroid conditions.
Comfort Promotion: Apply measures to enhance comfort and ease symptoms like pain, fatigue, and muscle weakness. Encourage rest and utilize suitable pain management techniques.
Nutritional Guidance: Work with dietitians to create suitable meal plans. These plans should support healthy thyroid function and address any dietary needs or restrictions.
Weight and Fluid Monitoring: Regularly monitor weight and fluid balance. Changes or imbalances can be indicators of thyroid dysfunction.
Imaging Assistance: Help coordinate and assist with thyroid imaging tests like ultrasounds or radioactive iodine scans. Ensure patient comfort and safety throughout these procedures.
Team Collaboration: Work closely with doctors, specialists (endocrinologists), and other healthcare team members. This ensures well-coordinated care and clear communication about the patient’s thyroid condition and treatment.
Side Effect Monitoring: Observe patients for any potential side effects or negative reactions from their medications, especially thyroid hormone replacements or antithyroid drugs.
Self-Care Education: Instruct patients on self-care practices for effective condition management. This includes correct medication use, symptom self-monitoring, and recognizing signs that thyroid function is worsening.
Post-Thyroidectomy Care: For patients who have had their thyroid surgically removed (thyroidectomy), provide post-operative care. This includes wound management, pain relief, and monitoring for any post-surgery complications.
Thyroid Storm Management: In cases of thyroid storm (a critical condition due to severe hyperthyroidism), closely monitor vital signs. Administer prescribed medications like antithyroid drugs and beta-blockers, and provide comprehensive supportive care.
Discharge Planning: Collaborate with the healthcare team to plan for the patient’s discharge. Ensure clear instructions are given regarding medications, follow-up appointments, and long-term self-management strategies.
Complications of Thyroidectomy
Postoperative Bleeding: Due to the thyroid gland’s rich blood supply, hemorrhage can occur after surgery.
Thyroid Crisis (Thyroid Storm): A severe condition characterized by rapid heartbeat, elevated body temperature, excessive sweating, and mental confusion.
Tetany: Involuntary muscle spasms caused by low calcium levels, potentially resulting from parathyroid gland issues during surgery. Symptoms include tingling and numbness in the face, lips, and extremities.
Sore Throat: A common discomfort following surgery, usually temporary.
Hoarseness: Voice changes due to potential injury to the recurrent laryngeal nerve, which controls vocal cord function.
Hypothyroidism: Insufficient thyroid hormone production as a consequence of thyroid tissue removal.
Recurrent Thyrotoxicosis: Return of hyperthyroidism symptoms, although less common after complete thyroidectomy.
Respiratory Obstruction: Breathing difficulties arising from swelling in the larynx (laryngeal edema).
Wound Infection: Infection at the surgical site.
Advice on Discharge
Following your thyroidectomy, it’s important to adhere to these guidelines:
Medication Adherence: Take all prescribed medications as directed until completion.
Neck Exercises: Perform recommended neck exercises to prevent stiffness and promote healing.
Hygiene Practices: Maintain good personal hygiene to minimize the risk of wound infections.
Balanced Diet: Consume a nutritious and well-balanced diet to support recovery.
Scar Care: Apply a moisturizing cream, such as lanolin, to the healed incision to aid in scar management.
Medication Caution: Avoid taking any non-prescribed medications without consulting your doctor.
Temperature Regulation: Limit exposure to excessively hot environments.
Follow-up Appointments: Attend all scheduled follow-up appointments for monitoring and assessment.
Follow-up Care
Thyroid Function Monitoring: Regular blood tests are essential to check thyroid hormone levels.
Medication Adjustments: Dosage of thyroid medication may be adjusted based on blood test results and individual needs.
Patient Education
Dietary Guidance: Receive instructions on any necessary dietary considerations post-surgery.
Medication Compliance: Understand the importance of consistently taking prescribed medications.
Symptom Awareness: Learn to recognize symptoms that require immediate medical attention and know when to seek help.
Long-Term Management
Maintenance Therapy: Ongoing treatment strategies will be implemented based on the specific surgical approach and individual health status.
Continuous Monitoring: Regular check-ups are necessary to detect and manage any potential long-term complications.
Thyroid Storm Management
Rapid Identification: Promptly recognize the signs of thyroid storm, characterized by severely exaggerated hyperthyroid symptoms.
Immediate Resuscitation:
Beta-blockers (IV Propranolol): Administered intravenously to quickly control rapid heart rate and other acute symptoms.
Thioamides (Methimazole): Given to reduce thyroid hormone production.
Additional Treatments:
Iodine Solutions/Radiocontrast Agents: Used to further inhibit thyroid hormone release.
Intravenous Steroids (Hydrocortisone): Administered to manage inflammation.
Intensive Monitoring: Closely monitor vital signs and thyroid hormone levels continuously. Adjust treatment as needed based on the patient’s response.
Complications of Hyperthyroidism/Thyrotoxicosis
Cardiac Issues:
Tachycardia & Arrhythmias: Elevated thyroid hormones can cause a rapid heart rate and irregular heart rhythms, such as atrial fibrillation.
Heart Failure: Long-term strain on the heart can lead to heart muscle weakening and heart failure.
Osteoporosis: Accelerated bone breakdown leading to reduced bone density and increased fracture risk. Calcium and vitamin D imbalances can worsen bone loss.
Thyroid Storm (Severe Thyrotoxicosis): A life-threatening emergency with sudden worsening of hyperthyroidism symptoms, including very high fever, extreme rapid heart rate, and potential organ failure.
Eye Problems (Graves’ Ophthalmopathy): Associated with Graves’ disease, causing inflammation of eye tissues, bulging eyes (proptosis), double vision, and possibly vision impairment.
Skin and Hair Changes: May cause thinning skin and fine, brittle hair. Skin redness or swelling can also occur.
Psychological Effects: Chronic anxiety, mood swings, and irritability are common. Severe cases can contribute to depression or worsen existing mental health conditions.
Menstrual Irregularities: Thyroid hormone imbalances can disrupt menstrual cycles, leading to lighter or irregular periods, and longer cycle lengths.
Muscle Weakness and Atrophy: Hyperthyroidism can cause muscle weakness, particularly in the upper arms and thighs. Prolonged muscle breakdown can result in muscle wasting.
Digestive Issues: Increased bowel movements and diarrhea are frequent symptoms. Chronic digestive problems can lead to nutrient deficiencies and weight loss.
Cognitive Impairment: Difficulty concentrating and memory problems can occur due to hormonal imbalances and anxiety.
Thyroid Crisis (Thyrotoxic Crisis/Storm): An extreme form of untreated hyperthyroidism leading to a sudden surge in symptoms, including very high body temperature, cardiovascular collapse, and neurological dysfunction.
Pregnancy Complications: Hyperthyroidism during pregnancy increases risks for both mother and baby, including premature birth, low birth weight, and maternal heart problems.
Liver and Kidney Dysfunction: Long-term hyperthyroidism can affect liver and kidney function due to increased metabolic demands and organ strain.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowRelated Topics
Medical Conditions Affecting the Endocrine System
- Applied Anatomy and Physiology of the Endocrine System
- Acromegaly/Gigantism (Hyperpituitarism)
- Dwarfism (Panhypopituitarism)
- Addison’s Disease (Adrenal Insufficiency)
- Pheochromocytoma
- Cushing’s Syndrome
- Hyperaldosteronism
- Thyrotoxicosis
- Diabetes Mellitus
Conditions Affecting the Nervous System
- Applied Anatomy and Physiology of the Nervous System
- Trigeminal Neuralgia
- Bell’s Palsy
- Parkinson’s Disease
- Spinal Cord Compression
- Transverse Myelitis
Medical Diseases Affecting the Renal System
- Anatomy and Physiology of the Renal System
- Renal Disorders
- Urinary Tract Infections (UTIs)
- Cystitis
- Renal Failure (Acute and Chronic)Nephrotic Syndrome
- Polycystic Kidney Disease (PKD)
- Kidney Stones (Nephrolithiasis)
Conditions of the Lymphatic System
- Anatomy and Physiology of the Lymphatic System
- Lymphedema
- Lymphangitis and Lymphadenitis
- Hodgkin’s Disease
Conditions of the Musculo-Skeletal System
- Anatomy and Physiology of the Musculo-Skeletal System
- Tendonitis
- Rheumatoid Arthritis
- Osteoarthritis
- Gout
- Bursitis
- Ankylosing Spondylitis
- Osteoporosis
- Paget’s Disease
Skin Conditions (Dermatology)
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

