Specialized Nursing Care
Subtopic:
Wound Dressing
Table of Contents

Wound Dressing
Wound dressing is defined as a method of carrying out surgical dressing and operative treatment with the primary aim of preventing the entry of microorganisms into the wound.
The purposes of dressing a wound include:
- To protect the wound from further injury or infection.
- To absorb exudates such as pus or serum.
- To immobilize and support the injured part.
- To apply pressure on the wound to control bleeding or approximate the wound.
- To provide psychological and physical comfort for the patient.
- To hold medications applied locally in place.
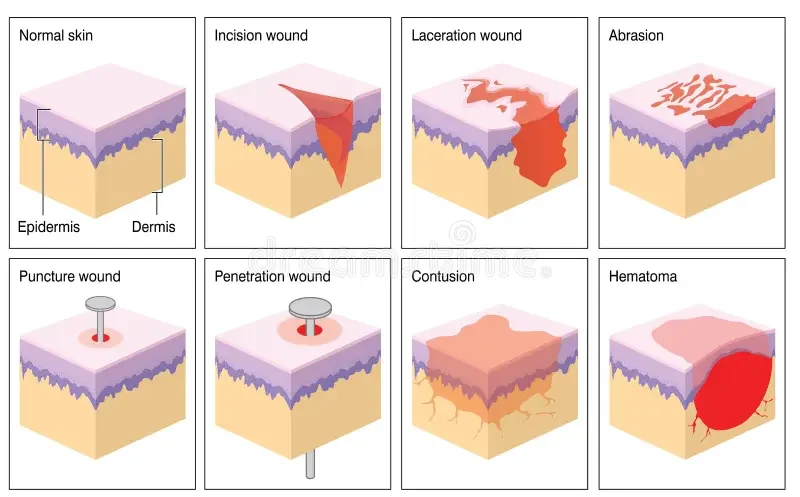
Definition and Classification of Wounds
A wound is a cut or break in the normal continuity of the skin or body structure, either internally or externally. Wounds can be classified based on their manner of production, bacterial content, extent, and time.
- Classification by Manner of Production:
- Abraded Wound (Abrasion): Caused by friction that removes the superficial layer of the skin. Commonly occurs due to falls on rough surfaces like sand or concrete.
- Incised Wound: Results from a sharp cutting instrument, producing a clean and well-defined separation of tissue. Examples include surgical incisions or cuts from a sharp knife.
- Contused Wound: Caused by a blunt object, leading to significant injury to the soft tissue, characterized by bruising (hemorrhage) and swelling. Examples include injuries from a blow or impact from a falling object.
- Lacerated Wound: Involves tearing of tissue, resulting in irregular and ragged wound edges. Commonly caused by glass, metal, machinery accidents, or animal bites.
- Penetrating Wound: Pierces through deep tissues and may enter a body cavity or organ. Examples include stab wounds or gunshot injuries.
- Punctured Wound: Made by a sharp, narrow, and pointed object, usually deep with a small entry point, increasing the risk of infection. Examples include injuries from nails or splinters.
- Classification by Bacterial Content:
- Clean Wound: Contains no pathogenic organisms and is made under sterile conditions, such as surgical wounds with aseptic techniques. Some microbial presence is inevitable on the skin, but the immune system prevents infection.
- Contaminated Wound: Contains a significant number of microorganisms. All accidental wounds fall into this category as they occur in uncontrolled environments without aseptic precautions.
- Septic (Infected) Wound: A wound infected by pathogenic microorganisms that lead to tissue destruction and pus formation. A previously clean or contaminated wound can become septic due to unsterile techniques or immune response failure.
- Classification by Extent:
- Open Wound: There is a break in the skin or mucous membrane, exposing underlying tissue to external contaminants. These wounds pose a higher risk of infection. Examples include incisions, abrasions, lacerations, and puncture wounds.
- Closed Wound: The skin remains intact, but underlying tissue is damaged. Internal bleeding, swelling, or bruising (hematoma) may occur. An example is contusions (bruises) from blunt trauma.
- Classification by Time:
- Acute Wound: A wound that heals within four weeks. Includes surgical wounds, minor cuts, and abrasions that heal without complications.
- Chronic Wound: A wound that fails to heal within four weeks and remains in the inflammatory phase of healing. These may be associated with conditions like diabetes, poor circulation, or infection. Examples include pressure ulcers, diabetic foot ulcers, and venous leg ulcers.
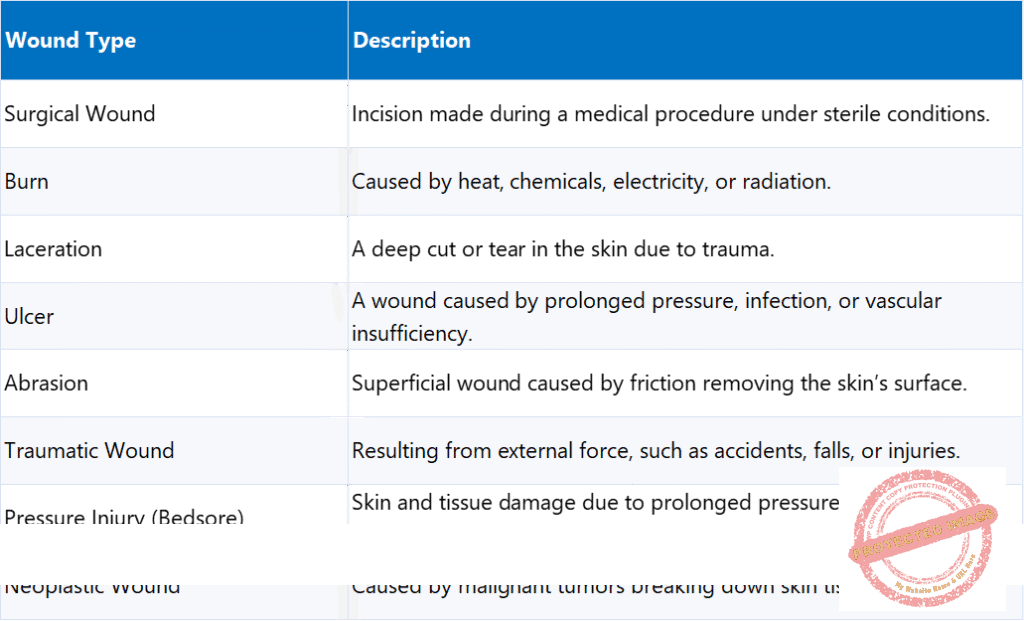
Wound types
Wound Healing
Wound healing refers to the body’s natural process of replacing destroyed tissue with new, living tissue. This complex biological process involves multiple phases and can be influenced by various internal and external factors.
Factors Affecting Wound Healing:
- Age: Younger individuals tend to heal faster due as they have higher cellular activity and collagen production, whereas elderly individuals may experience delayed healing due to reduced skin elasticity, lower immune response, and slower cell regeneration.
- Nutritional Status: Proper nutrition is essential, and deficiencies in proteins, carbohydrates, lipids, vitamins (especially A, C, and E), and minerals (such as zinc and iron) can delay healing. Proteins are crucial for cell growth and tissue repair, and Vitamin C is essential for collagen formation, while Vitamin A aids in immune function and epithelial cell formation.
- Type of Wound: Clean surgical wounds heal faster than contaminated or infected wounds, and deep wounds with tissue loss take longer to heal than superficial wounds.
- Blood Supply to the Affected Area: Adequate blood circulation ensures oxygen and nutrient delivery, promoting faster healing. Conditions like diabetes, peripheral artery disease, and smoking can impair circulation and slow healing.
- Presence of Foreign Bodies: Dirt, debris, sutures, or other foreign materials in the wound can delay healing and increase infection risk.
- Infection: Infections introduce bacteria into the wound, causing inflammation, pus formation, and delayed healing. Bacteria prevent new tissue from forming properly.
- Lack of Rest of the Affected Part: Continuous movement or strain on a wound can prevent proper tissue formation and delay healing; immobilization and rest allow new cells to regenerate effectively.
- Hemorrhage (Excessive Bleeding): Uncontrolled bleeding can prevent clot formation, delaying the healing process. Blood loss reduces oxygen supply to the wound, which is crucial for tissue repair.
- Presence of Dead Space in the Wound: Dead space refers to empty spaces between tissues where fluid can accumulate, increasing infection risk. Proper wound closure techniques help eliminate dead spaces.
- Malnutrition: An inadequate supply of proteins, carbohydrates, lipids, vitamins, and trace elements can slow down all phases of wound healing.
- Medications: Certain medications can impair healing, such as NSAIDs, chemotherapy and immunosuppressive drugs, and corticosteroids.
- Stress, Anxiety, and Depression: Emotional and psychological stress can negatively affect immune function and hormone balance, leading to slower wound healing.
- Underlying Diseases: Conditions like diabetes, autoimmune disorders, anemia, and cancer can impair wound healing by reducing immune function, circulation, and tissue regeneration.
Types of Wound Healing (Wound Closure):
- Healing by Primary Intention (First Intention): The wound edges are brought together (approximated) using sutures, staples, or adhesive strips. This occurs in clean wounds with minimal tissue loss, such as surgical incisions, resulting in quick healing with minimal scarring.
- Healing by Secondary Intention (Granulation Healing): Occurs when there is significant tissue damage or infection, preventing the wound edges from being approximated. The wound heals from the bottom up, filling with granulation tissue (new connective tissue and blood vessels). This process requires daily wound dressing due to infection risk, has a longer healing time, and results in more prominent scarring.
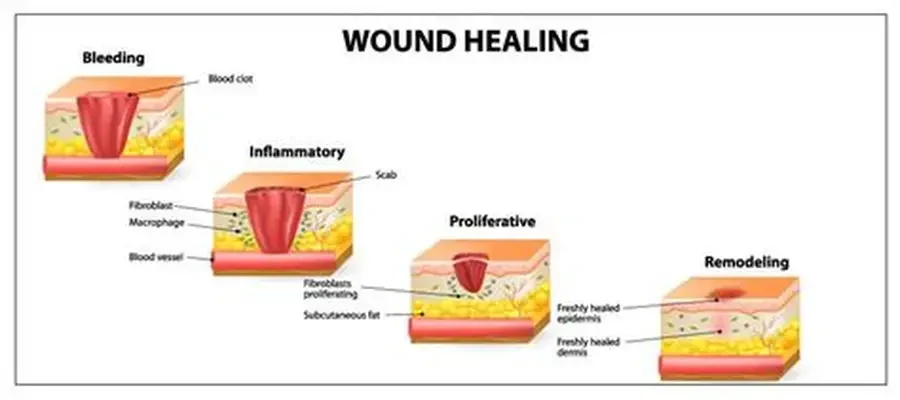
Phases of Wound Healing
The wound healing process consists of four overlapping phases, often called the “cascade of healing”:
- Hemostasis Phase (Bleeding Control Phase): This is the immediate response to physical injury, ensuring bleeding is controlled. It includes vasoconstriction, platelet response forming a clot, and a biochemical response releasing clotting factors.
- Inflammatory Phase: Damaged cells release cytokines that attract white blood cells to fight infection. Key events include temporary blood vessel constriction followed by dilation, allowing immune cells to reach the wound. Neutrophils arrive within 24 hours to remove bacteria and dead tissue.
- Proliferative Phase: Begins once neutrophils have cleared cellular debris. Fibroblasts migrate to the wound and produce collagen (Type III initially) for structural support, and angiogenesis (formation of new blood vessels) starts within 48 hours. Wound strength significantly increases during this phase, which lasts up to 3 weeks.
- Maturation (Remodeling) Phase: Begins around week 3 and continues for 9 to 12 months. During this phase, Collagen Type III is replaced with Collagen Type I, increasing tensile strength up to 80% of normal skin, and the wound contracts as scar tissue forms.
Care of Wounds Dressing Methods:
- Dressing Method: Covers the wound to promote healing.
- Non-Dressing Method: Leaves the wound open to air for healing.
Advantages of Dressing:
- Absorbs wound drainage.
- Protects from contamination (feces, urine, vomit, etc.).
- Provides immobilization and prevents mechanical injuries.
- Helps with hemostasis (prevents bleeding).
- Provides psychological and physical comfort for the patient.
Advantages of Non-Dressing Method:
- Prevents bacterial growth by eliminating warmth and moisture.
- Allows better observation of the wound.
- Facilitates bathing without disrupting healing.
- Avoids allergic reactions from adhesive tapes.
- More economical and comfortable for the patient.
Disadvantages of Non-Dressing Method:
- Exposure of large wounds may cause anxiety for some patients.
- Increased risk of contamination in an unclean environment.
Qualities of a Good Dressing:
- Sterile: Free from microorganisms.
- Lightweight: Comfortable and non-bulky.
- Porous: Allows air circulation to prevent moisture buildup.
Types of Dressings:
- Dry Dressing: Used for clean wounds. Typically made of 4 to 8 layers of gauze, applied after antiseptic treatment.
- Wet Dressing: Used for infected wounds with pus, softening discharge and promoting drainage. Made of moistened antiseptic gauze with multiple layers.
- Pressure Dressing: Applied with firm bandages to control bleeding and reduce oozing. Commonly used for trauma or post-surgical wounds.
Sources of Wound Infection in the Ward:
- Airborne Contaminants: Dust particles or infected droplets from the nose and mouth of patients, visitors, and medical staff.
- Hands of Healthcare Providers: Bacteria and pathogens from nurses, doctors, and other staff may transfer to wounds if proper hand hygiene is not followed.
- Improper Dressing Techniques: Inadequate sterilization and incorrect handling of wounds can introduce infections.
- Use of Unsterile Instruments: Dressing materials and instruments that are not properly sterilized can be a source of infection.
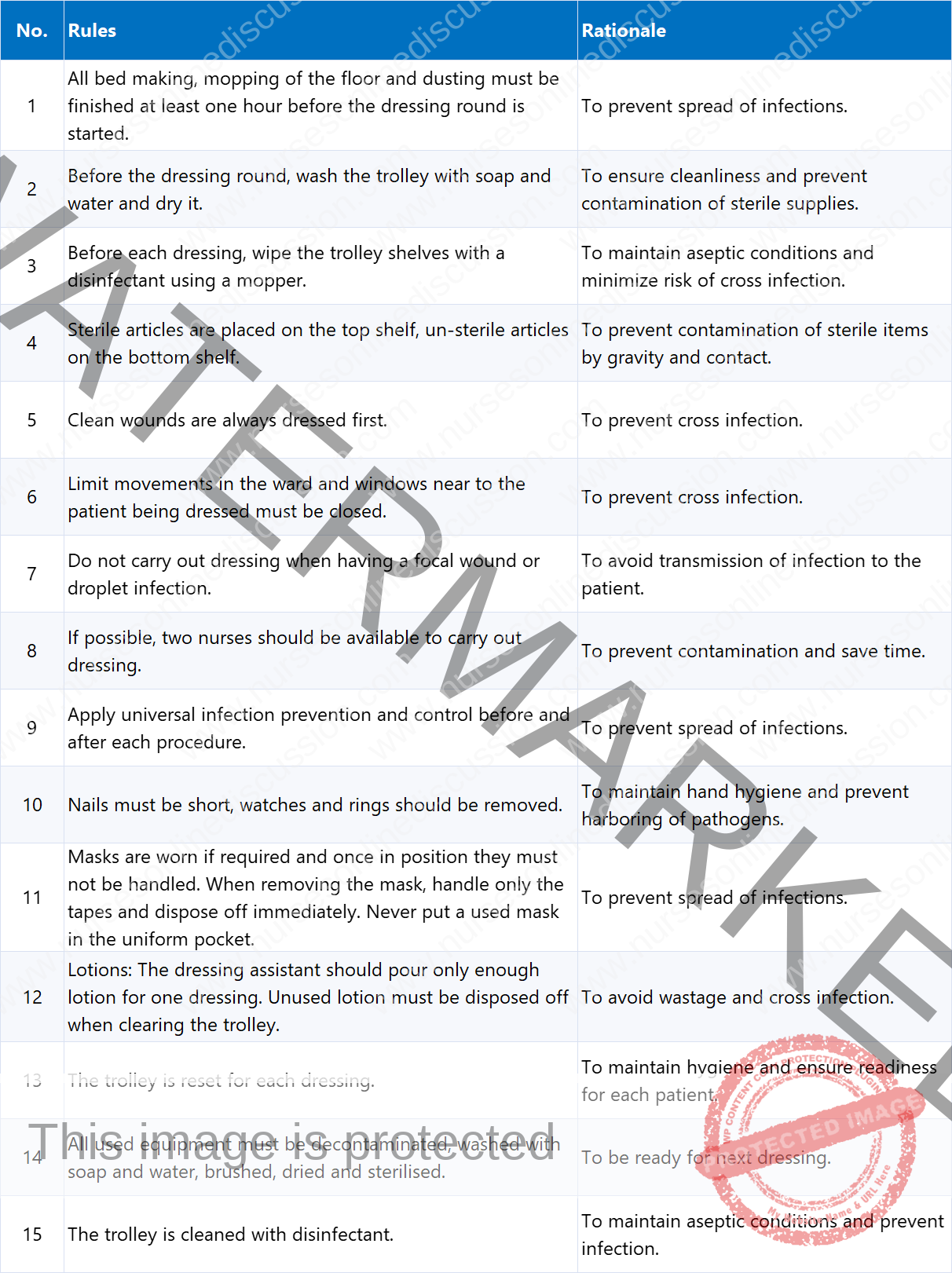
General Rules for Wound Dressing
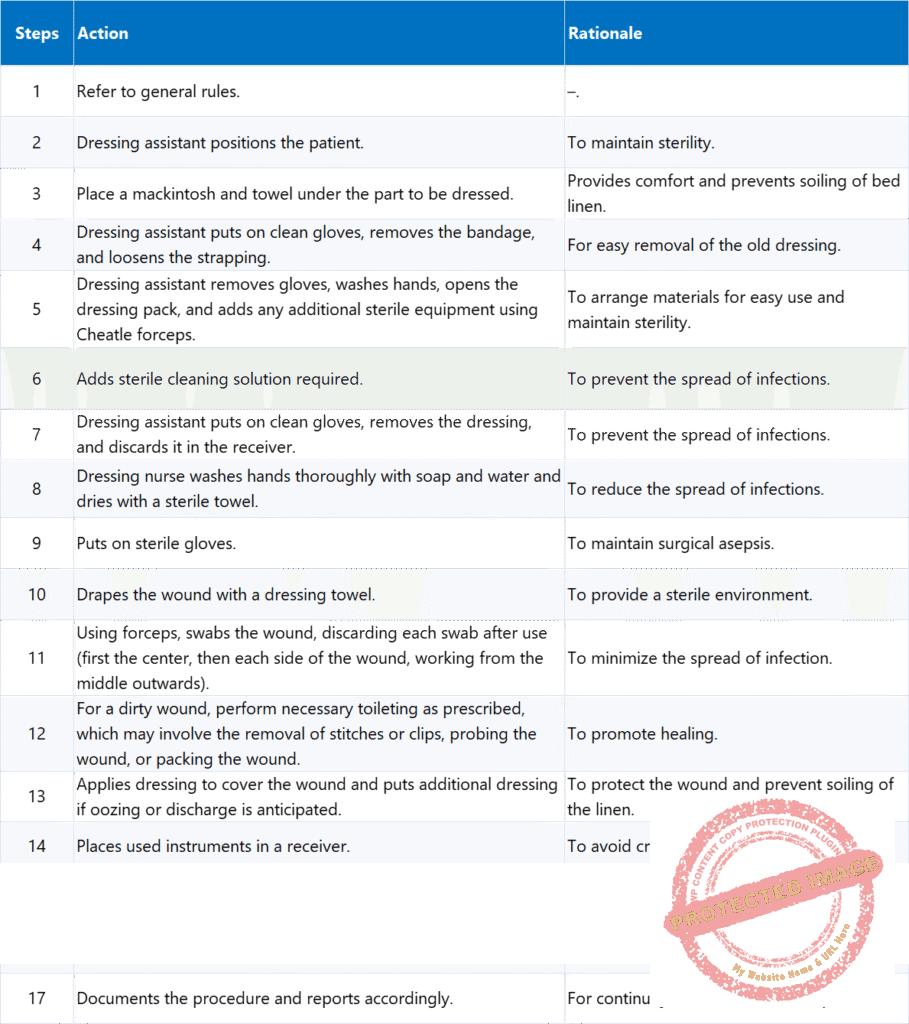
Wound Dressing Procedures
Dressing a Clean Wound A clean wound is a superficial wound caused by uncontaminated sharp objects. It may occur electively (e.g., surgical incision) or accidentally (e.g., cuts from broken glass or sharp metal).
Purpose of Dressing a Clean Wound
- To keep the wound clean and free from infection.
- To prevent the wound from further injury and contamination.
- To hold medications applied locally in place.
- To immobilize the wound edges, promoting faster healing.
- To apply pressure, minimizing bleeding and swelling.
Requirements for Clean Wounds
Top Shelf
Sterile Dressing Pack Containing:
- 2 dressing towels
- 2 non-toothed dissecting forceps
- 2 dressing forceps
- 3 gallipots:
- 1 for swabs
- 1 for lotion
- 1 for gauze dressing
A pair of stitch scissors or a clip remover (if required)
Additional Items:
- Probe
- Sinus forceps
Bottom Shelf
- Dressing mackintosh and towel
- Receiver for soiled dressings
- Receiver for used instruments
- Bottle of antiseptic lotion
- Drum for dressing
- Drum for swabs
- Tray containing:
- Bandages
- Scissors
- Safety pins
- Strapping
- Container of Cheatle forceps
- A pair of gloves and a pair of clean gloves
- Bowl
- Hydrogen peroxide
- Pus swab
- Laboratory form
- Hypotonic saline
Bedside
- Hand washing equipment
- Pedal bin
Extra Requirements for Dirty Wounds
- Probe
- Sinus forceps
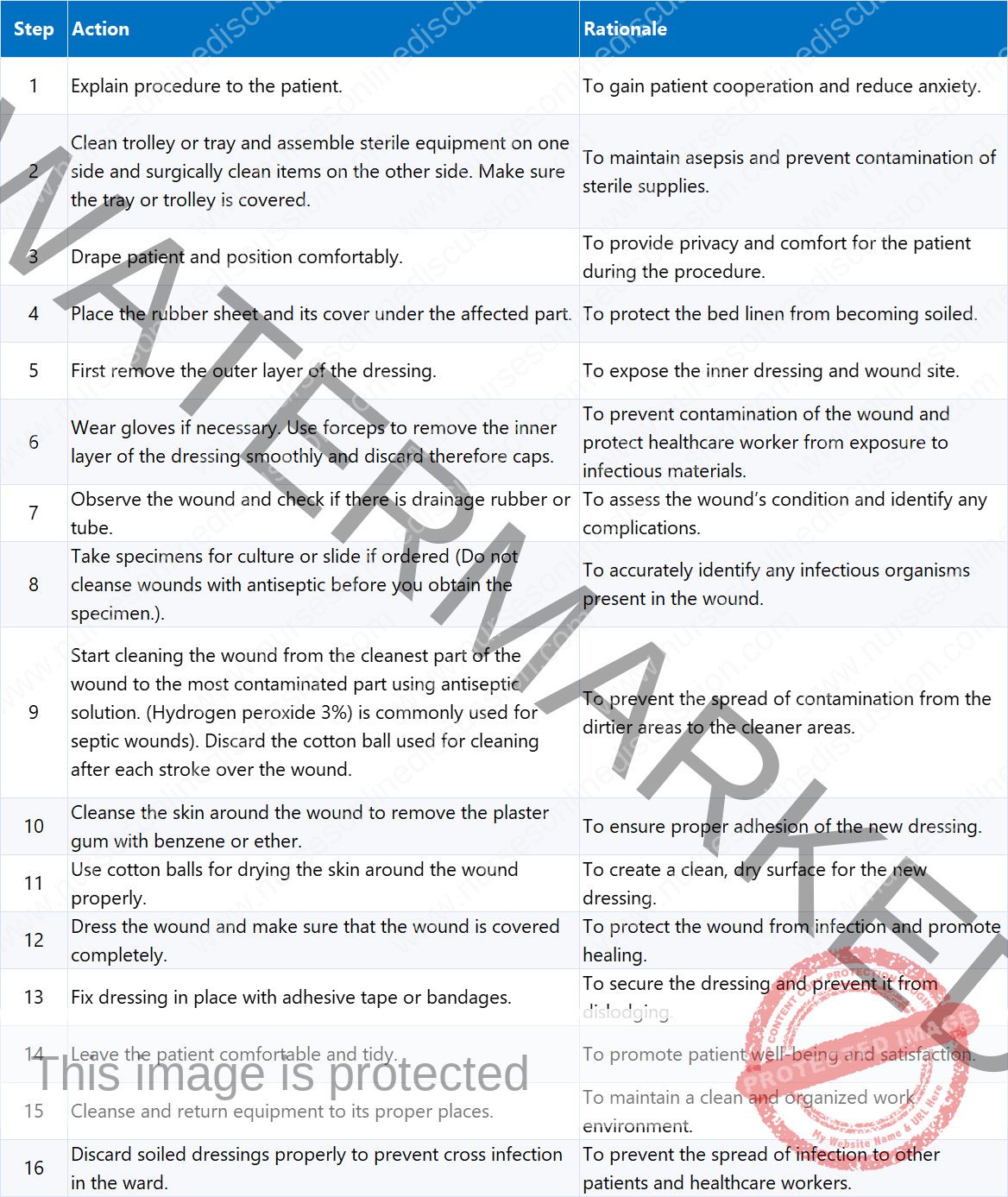
Procedure for Dressing a Clean Wound
Dressing of Septic Wound
A septic wound is characterized by the presence of pus, dead skin, and offensive odour in the wound. Septic wounds may need irrigation.
Purpose of Dressing a Septic Wound
- To absorb discharge from the wound.
- To apply pressure and prevent excessive fluid buildup.
- To apply local medications for infection control.
- To reduce pain, swelling, and further tissue injury.
Additional Items (Top Shelf) for Septic Wound Dressing with Irrigation:
- Bowl containing irrigation lotion (e.g., hydrogen peroxide).
- Saline 0.9% solution.
- Receiver containing large syringe and fine catheter.
- Receiver for used lotion.
- Probe, Sinus forceps, Pus swab, Laboratory form, Hypotonic saline, Pedal bin.
Procedure for Dressing a Septic Wound
Note: If sterile forceps are not available, use sterile gloves. Immerse used instruments in strong antiseptic solution before cleansing. In a big ward, prioritize clean wounds before septic wounds to lessen cross-infection risk. Provide privacy for the patient. Wounds should not be too tightly packed as this may delay healing.
Wound Irrigation
Wound irrigation is the process of removing foreign materials, reducing bacterial contamination, and clearing cellular debris or exudate from the wound surface. It is a critical step in wound management, helping to maintain a clean environment that promotes optimal healing. The procedure must be vigorous enough for effective cleansing but gentle enough to prevent additional tissue trauma or the unintentional spread of bacteria deeper into the wound. Since wound irrigation involves bodily fluids, splashing and spraying can occur due to the use of pressure; therefore, proper personal protective equipment (PPE) such as gloves, masks, eye protection, and gowns must be worn.
Essential Steps of Wound Irrigation:
- Assessing the Wound: Evaluate the wound’s size, depth, level of contamination, and presence of infection.
- Wound Anesthesia: If necessary, provide local anesthesia to minimize patient discomfort.
- Wound Periphery Cleansing: Clean the skin around the wound using antiseptic solutions to prevent external contamination.
- Irrigation with Solution Under Pressure: Flush the wound using an appropriate solution with controlled pressure to remove debris and bacteria effectively.
Indications for Wound Irrigation: Wound irrigation is recommended for both acute and chronic wounds, especially when:
- The wound is contaminated with debris or foreign materials.
- The wound will undergo suturing, surgical repair, or debridement.
- The wound has exudate buildup, which may delay healing.
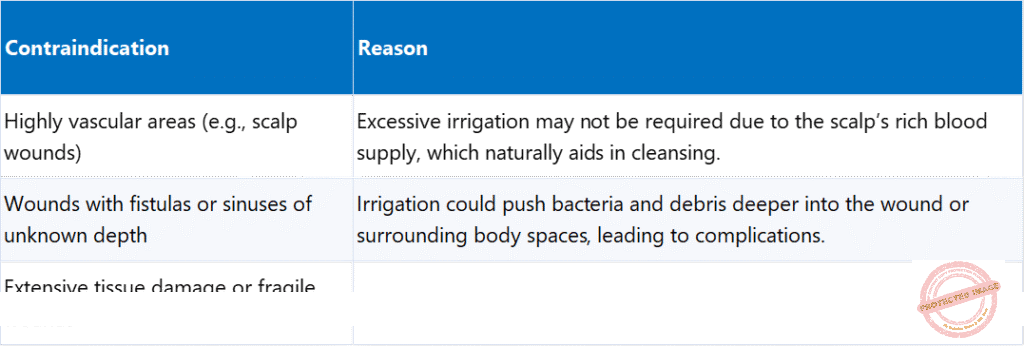
Contraindications for Wound Irrigation:
- Highly vascular areas (e.g., scalp wounds): Excessive irrigation may not be required due to the scalp’s rich blood supply, which naturally aids in cleansing.
- Wounds with fistulas or sinuses of unknown depth: Irrigation could push bacteria and debris deeper into the wound or surrounding body spaces, leading to complications.
- Extensive tissue damage or fragile wounds: Excessive irrigation pressure can worsen tissue injury.
- Actively bleeding wounds: Irrigation should be avoided as it can disrupt clot formation and exacerbate hemorrhage.
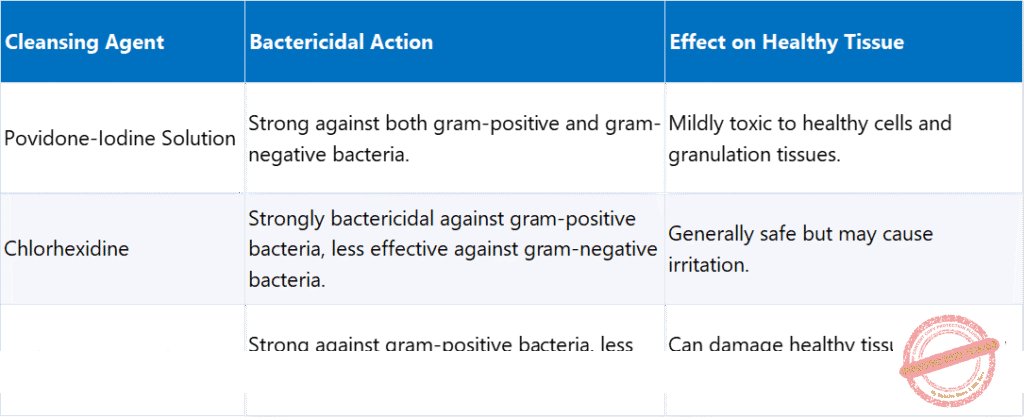
Wound Cleansing Agents:
- Povidone-Iodine Solution: Strong against both gram-positive and gram-negative bacteria, but mildly toxic to healthy cells and granulation tissues.
- Chlorhexidine: Strongly bactericidal against gram-positive bacteria, less effective against gram-negative bacteria, and generally safe but may cause irritation.
- Hydrogen Peroxide: Strong against gram-positive bacteria, less effective against gram-negative bacteria, but can damage healthy tissue and delay healing
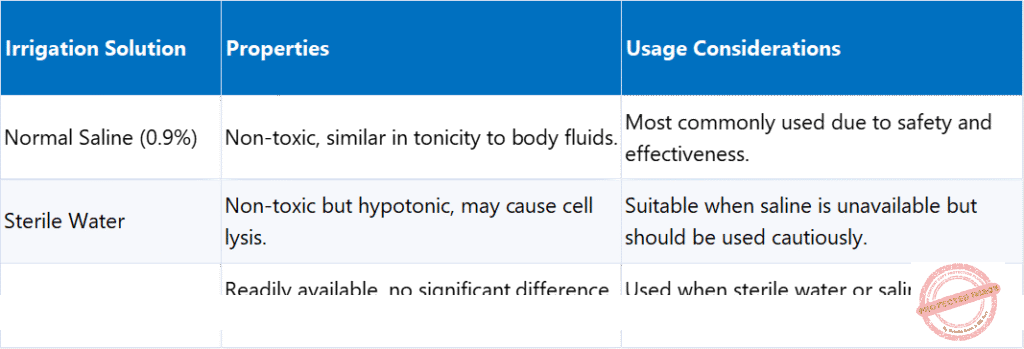
Irrigation Solutions for Wound Cleansing:
- Normal Saline (0.9%): Non-toxic, similar in tonicity to body fluids, and most commonly used due to safety and effectiveness.
- Sterile Water: Non-toxic but hypotonic, may cause cell lysis. Suitable when saline is unavailable but should be used cautiously.
- Potable Water: Readily available, no significant difference from sterile water in infection rates. Used when sterile water or saline is unavailable.
Requirements for Wound Irrigation:
- 2 Receivers.
- Rubber sheet and its cover.
- Solutions (Hydrogen Peroxide or Normal Saline).
- Adhesive tape or bandage, bandage scissors.
- Sterile Syringe (with desired amount of solution) and Catheter.
- Sterile Forceps (2).
Procedure for Wound Irrigation

Complications of Incomplete or Inadequate Wound Irrigation:
- Persistent Debris: Increases the risk of infection and delayed healing.
- Sinus Formation: In abscesses, can lead to chronic sinus tract formation.
- Infection: Retained bacteria and contaminants can promote local or systemic infection.
- Cytotoxicity: Excessive use or direct instillation of povidone-iodine into deep wounds can be cytotoxic, impairing healing; it should be used carefully, primarily on wound edges, and avoided in large quantities within the wound.
Wound Assessment
Wound assessment is a critical process in wound management that allows healthcare professionals to determine the appropriate treatment plan and monitor healing progression. It involves evaluating the type, severity, and condition of the wound, along with assessing for signs of infection, complications, or delayed healing. Both initial and ongoing wound assessments should be conducted systematically in collaboration with the treating team.
Key Factors in a Comprehensive Wound Assessment:
- Type of Wound: Categorized as acute or chronic based on duration and healing progression. Examples include surgical wounds, lacerations, ulcers, burns, abrasions, traumatic injuries, pressure injuries, and neoplastic wounds.
- Aetiology (Cause of Wound): Understanding the cause informs treatment.
- Wound Location & Surrounding Skin: Important for understanding healing potential and impact on mobility/function.
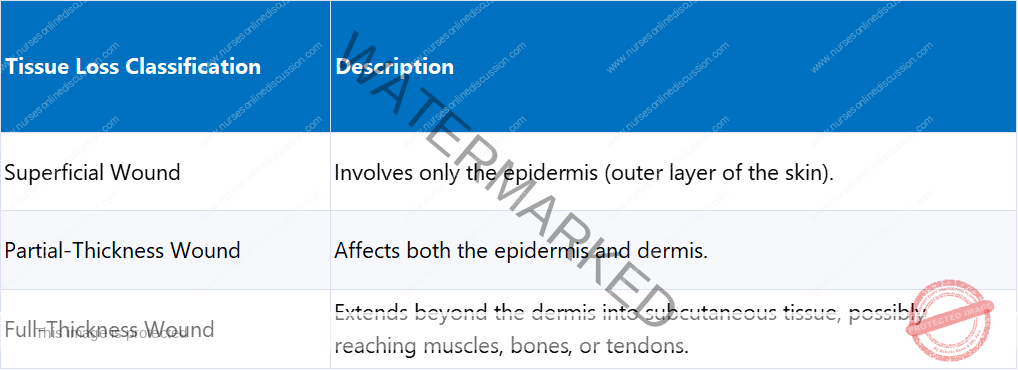
- Tissue Loss: Determines whether the wound is superficial (only epidermis), partial-thickness (epidermis and dermis), or full-thickness (extends beyond dermis into subcutaneous tissue, possibly muscles, bones, or tendons).
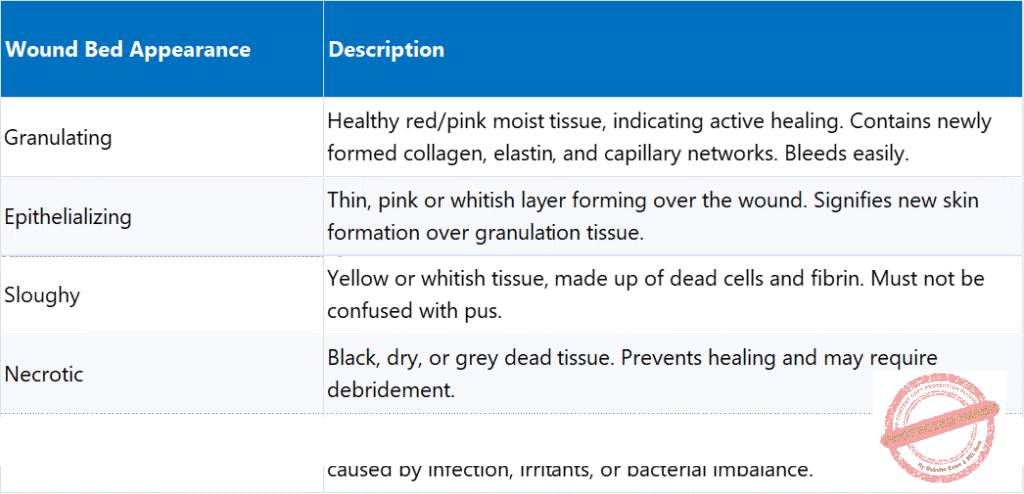
- Clinical Appearance of Wound Bed: Indicates the stage of healing and tissue viability.
- Granulating: Healthy red/pink moist tissue, indicating active healing with newly formed collagen, elastin, and capillaries. Bleeds easily.
- Epithelializing: Thin, pink or whitish layer forming over the wound, signifying new skin formation.
- Sloughy: Yellow or whitish tissue, made up of dead cells and fibrin, not to be confused with pus.
- Necrotic: Black, dry, or grey dead tissue that prevents healing and may require debridement.
- Hypergranulating: Excess granulation tissue, extending beyond wound margins, often caused by infection, irritants, or bacterial imbalance.
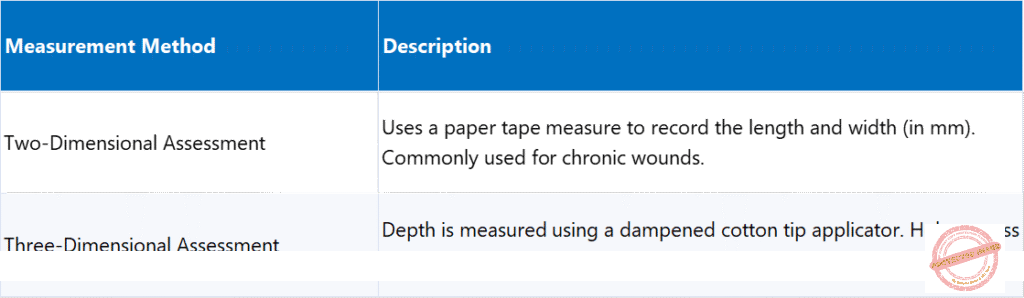
- Measurement & Dimensions: Includes both two-dimensional (length and width in mm using paper tape, common for chronic wounds) and three-dimensional (depth measured with dampened cotton tip applicator, helps assess cavity or tunneling wounds) assessments.
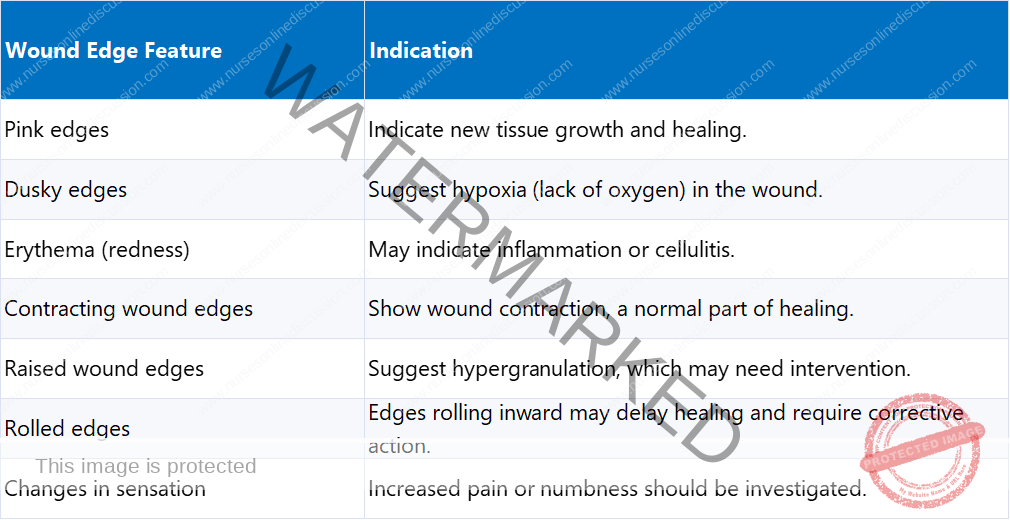
- Wound Edges: Assessed for color, contraction, elevation, and rolling, all of which impact healing.
- Pink edges: Indicate new tissue growth and healing.
- Dusky edges: Suggest hypoxia (lack of oxygen).
- Erythema (redness): May indicate inflammation or cellulitis.
- Contracting wound edges: Show normal wound contraction.
- Raised wound edges: Suggest hypergranulation, which may need intervention.
- Rolled edges: Edges rolling inward may delay healing and require corrective action.
- Changes in sensation: Increased pain or numbness should be investigated.
- Exudate (Wound Drainage): Evaluated for quantity, color, consistency, and odor to detect infection or complications.
- Functions of Exudate: Provides nutrients and growth factors, contains white blood cells to fight infection, cleanses the wound by flushing out bacteria and debris, maintains moisture balance, and promotes epithelialization.
- Complications Related to Exudate: Excess exudate causes maceration (breakdown of surrounding skin), insufficient exudate leads to wound dryness and slowed healing, and odorous, thick exudate indicates infection or necrosis.
- Presence of Infection: Identified by local or systemic indicators of bacterial overgrowth. A wound infection occurs when bacteria multiply beyond the body’s ability to control them, leading to delayed healing, tissue destruction, or systemic illness.
- Local Signs of Infection: Redness (Erythema or Cellulitis), purulent or increased exudate, foul odor, localized pain, localized heat, and swelling (Oedema).
- Systemic Signs of Infection: Fever or chills, increased heart rate, fatigue or malaise, and spreading redness beyond the wound area.
- Previous Wound Management: Important for evaluating treatment effectiveness and necessary modifications.
1) Type of Wound (in Wound Assessment)
Wounds are classified based on their cause and general healing characteristics.
2) Tissue Loss (in Wound Assessment)
The depth of a wound determines the level of tissue loss
3) Clinical Appearance of the Wound Bed (in Wound Assessment)
This indicates the stage of healing and tissue viability. Different tissue types provide insight into the healing process and the need for intervention.
4) Wound Measurement (in Wound Assessment)
Accurate measurement of a wound’s size and depth is essential
5) Wound Edges (in Wound Assessment)
The edges of the wound provide valuable insight into healing progress. They are assessed for color, contraction, elevation, and rolling, all of which impact healing.
6) Exudate (Wound Drainage)
Exudate plays a critical role in healing but requires careful monitoring. It is evaluated for quantity, color, consistency, and odor to detect infection or complications.
Functions of Exudate in Healing:
- Provides nutrients and growth factors for cell metabolism.
- Contains white blood cells to fight infection.
- Cleanses the wound by flushing out bacteria and debris.
- Maintains moisture balance, preventing wound desiccation.
- Promotes epithelialization, aiding tissue regeneration.
Complications Related to Exudate:
- Excess exudate can cause maceration (breakdown of surrounding skin).
- Insufficient exudate leads to wound dryness, slowing healing.
- Odorous, thick exudate indicates infection or necrosis.
7) Surrounding Skin Condition
The surrounding skin should be examined for:
- Signs of maceration (excess moisture causing soft, broken skin).
- Erythema (redness indicating inflammation or infection).
- Dryness or cracking, which may slow healing.
- Skin integrity changes, requiring protection measures.
8) Presence of Infection
A wound infection occurs when bacteria multiply beyond the body’s ability to control them, leading to delayed healing, tissue destruction, or systemic illness. Infection is identified by local or systemic indicators of bacterial overgrowth.
Local Signs of Infection:
- Redness (Erythema or Cellulitis): Surrounding skin appears inflamed.
- Exudate Changes: Purulent (pus-like) or increased drainage.
- Foul Odor: A strong smell may indicate bacterial growth.
- Localized Pain: Increased pain in or around the wound.
- Localized Heat: Warmer than surrounding tissue.
- Swelling (Oedema): Fluid accumulation around the wound.
Systemic Signs of Infection (Indicating worsening condition)
- Fever or chills.
- Increased heart rate.
- Fatigue or malaise.
- Spreading redness beyond the wound area.
Related Topics
- Wound dressing
- Colostomy Care
- Abdominal Paracentesis(Abdominal Tapping)
- Vulva Toilet/ Swabbing
- Oxygen Administration
- Lumbar Puncture
- Nasogastric tube to feed patients
- Gastrostomy Feeding
- Gastric Lavage
- Catheterization
- Tracheostomy Care
- Caring for patients in traction
- Prepare for application of orthopaedic splints
- Bandaging
- Nursing Process
- Take History of the patient
- Perform a physical examination of the Patient
- Making a Nursing Care Plan
- Admission of a patient
- Drug administration
- Transfer Patients
- Discharge of patients
- Last Office
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

