Specialized Nursing Care
Subtopic:
Medication Administration
Table of Contents

A medication is a chemical substance given in a regulated dose for the purpose of diagnosing, curing, treating, or preventing disease. Medications can also be prescribed to produce specific therapeutic effects in the body. Administering medications safely and accurately is a critical responsibility for healthcare professionals.
The Rights of Medication Administration
To ensure patient safety and medication effectiveness, the following “Rights” should always be observed:
Right Patient: Verify the patient’s identity using at least two identifiers (e.g., name, date of birth).
Right Medication: Double-check the medication name and ensure it matches the prescription.
Right Dose: Confirm the correct dosage, including the strength and amount to be administered.
Right Route: Administer the medication via the prescribed route (e.g., oral, intravenous, intramuscular).
Right Time: Give the medication at the correct time and frequency.
Right Storage: Store the medication appropriately according to its specific requirements (e.g., refrigeration, protection from light).
Right Formulation: Ensure the medication is in the correct form (e.g., tablet, liquid, injection).
Right Disposal: Dispose of any unused or expired medication and related supplies properly.
Right Site: For injections and topical applications, administer at the correct site on the body.
Right Equipment: Use the appropriate equipment for medication administration (e.g., syringes, needles, IV tubing).
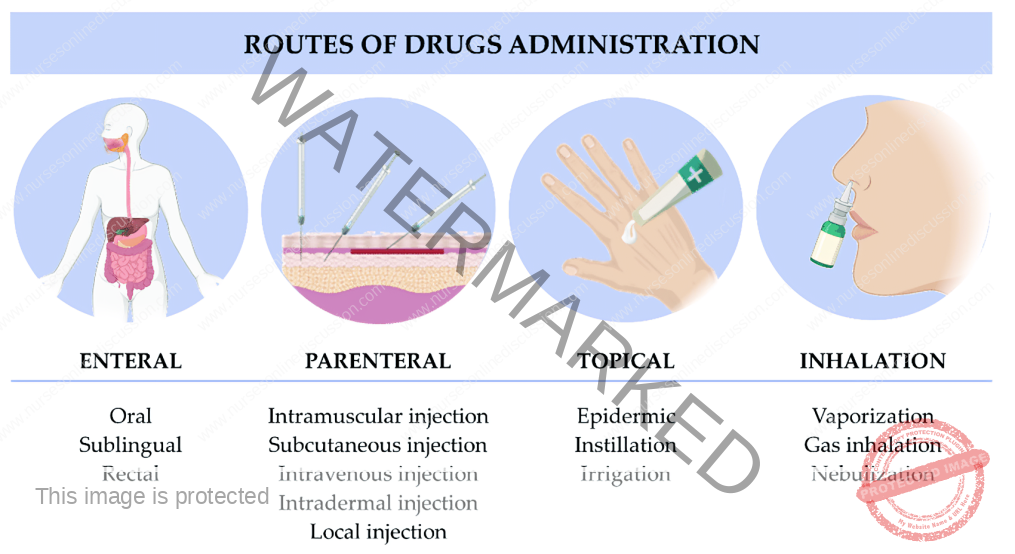
Routes of Medication Administration
Medications can be administered via various routes, broadly categorized as systemic (affecting the whole body) or local (targeting a specific area).
I. Systemic Routes
A. Enteral Route (through the gastrointestinal tract):
Oral: Medications taken by mouth (e.g., tablets, capsules, liquids) and absorbed through the stomach or intestinal lining.
Sublingual: Medications placed under the tongue, where they dissolve and are rapidly absorbed into the bloodstream.
Buccal: Medications placed between the cheek and gum, where they dissolve and are absorbed through the buccal mucosa.
Rectal: Medications administered rectally (e.g., suppositories, enemas) and absorbed through the rectal mucosa.
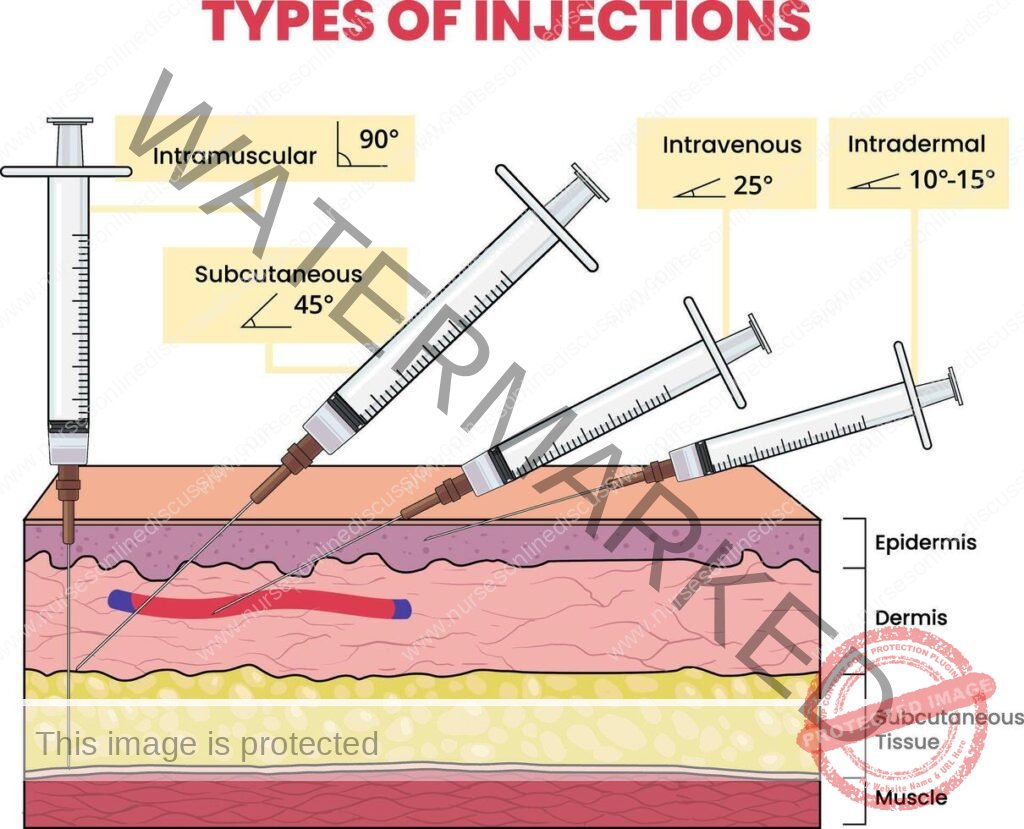
B. Parenteral Route (by injection):
Intravenous (IV): Injection directly into a vein, providing rapid and complete drug delivery to the bloodstream.
Intramuscular (IM): Injection into a muscle, allowing for gradual absorption into the bloodstream.
Subcutaneous (SC): Injection into the fatty tissue beneath the skin, providing slower absorption than IM.
Intra-arterial: Injection directly into an artery, used rarely for specific diagnostic or therapeutic purposes.
Intra-articular: Injection into a joint space, providing localized treatment for joint conditions.
Intrathecal: Injection into the cerebrospinal fluid surrounding the spinal cord, used for spinal anesthesia and certain medications.
Intradermal: Injection into the dermis (the layer of skin just below the epidermis), often used for allergy testing and tuberculosis screening.
Epidural: Injection into the epidural space surrounding the spinal cord, commonly used for pain management.
Intraperitoneal: Injection into the peritoneal cavity (abdominal cavity), sometimes used for chemotherapy.
Intracardiac: Injection directly into the heart muscle, used in emergencies like cardiac arrest (rarely used).
Intraosseous: Injection directly into the bone marrow, used in emergency situations when intravenous access is difficult or impossible to obtain quickly.
Intralymphatic: Injection into the lymphatic system, used in certain types of cancer treatment and for some vaccines.
II. Local Routes
Topical (Skin): Application of creams, ointments, gels, or lotions to the skin for localized treatment.
Intranasal: Administration of sprays or drops into the nasal passages for local (e.g., nasal decongestants) or systemic effects.
Ocular (Eye): Administration of drops or ointments into the eye to treat local conditions.
Otic (Ear): Administration of drops into the ear canal to treat local ear conditions.
Transdermal: Application of patches or gels to the skin for slow, continuous drug release and systemic absorption.
Mucosal:
Throat: Lozenges, sprays, or gargles for local treatment of throat conditions.
Vaginal: Creams, tablets, or rings inserted into the vagina for local treatment.
Urethral: Medications administered through the urethra.
Rectal: Suppositories or enemas for local treatment of rectal conditions.
Intrapleural: Injection into the pleural space surrounding the lungs, used for treating pleural effusions and certain cancers.
Inhalation: Administration of medications as a gas, vapor, or fine mist that is breathed in, allowing for rapid absorption through the lungs.
INHALATION
Inhalation involves breathing in a gas, vapor, or fine mist of medication into the lungs.
Types of Inhalation:
Dry Inhalation:
Oxygen Administration: Used when respiratory capacity is compromised, such as in chest injuries, pneumonia, and heart failure.
Moist/Steam Inhalation: Used to deliver moisture and often medication to the respiratory tract.
Indications:
To warm and moisten inhaled air and relieve irritation (e.g., in bronchitis, after tracheotomy).
To relieve inflammation and coughing (e.g., in colds).
To relieve congestion and edema (e.g., in sinusitis, acute laryngitis).
Nebulizer: A device that converts liquid medication into a fine mist that can be inhaled.
Indications for Nebulizer Use:
Respiratory diseases (e.g., asthma, pneumonia)
Airway obstruction
Nasal congestion
Nasal bleeding
Chest injuries
Cardiac failure
To relieve bronchospasm (e.g. in asthma) or chest pain (e.g. in angina pectoris)
Forms of Medications

Medications are available in various forms, broadly categorized as liquids, solids, and semisolids.
Liquids:
Solutions: Medications dissolved completely in a liquid, usually water.
Syrups: Medications dissolved in a sugar and water solution, often used to mask unpleasant tastes.
Mixtures: Medications combined with a liquid but not fully dissolved (may require shaking before use).
Milks: White, opaque mixtures of a medicinal substance in water.
Emulsions: Mixtures of oil and water, often containing a medication.
Elixirs: Medications dissolved in a sweetened, flavored, alcohol-containing solution.
Tinctures: Medications dissolved in alcohol or a mixture of alcohol and water.
Fluidextracts: Concentrated liquid extracts of medicinal plants, prepared by boiling and evaporation, and typically dissolved in alcohol.
Liniments: Medications mixed with oil, soap, or alcohol for external use only (applied to the skin).
Lotions: Liquid preparations, often water-based, for external application to the skin.
Solids and Semisolids:
Capsules: Gelatin shells containing medication in liquid, powder, or oil form.
Powders: Finely ground medications, either for internal or external use.
Pills: Round, solid dosage forms, often sugar-coated.
Tablets: Compressed solid dosage forms of various shapes, sizes, and weights.
Enteric-Coated Tablets: Tablets with a special coating that prevents them from dissolving in the stomach, allowing them to be absorbed in the small intestine.
Lozenges (Troches): Hard, disk-shaped medications designed to dissolve slowly in the mouth for local treatment of the mouth or throat.
Ointments: Medications mixed with a fatty or oily base for external application.
Pastes: Ointments with added powders for a thicker consistency.
Suppositories: Medications mixed with a firm base that melts at body temperature, designed for insertion into a body cavity (e.g., rectum, vagina).
Ampoules: Sealed glass containers typically containing a single dose of liquid or powdered medication for injection.
Vials: Glass containers with rubber stoppers, containing either single or multiple doses of liquid or powdered medication for injection.
Common Medication Administration Times
Four Hourly (q4h): Six times in 24 hours (e.g., 6 AM, 10 AM, 2 PM, 6 PM, 10 PM, 2 AM).
Six Hourly (q6h): Four times in 24 hours (e.g., 6 AM, 12 PM, 6 PM, 12 AM).
Eight Hourly (q8h): Three times in 24 hours (e.g., 6 AM, 2 PM, 10 PM).
Twelve Hourly (q12h) or Twice Daily (BID): Two times in 24 hours (e.g., 6 AM and 6 PM).
Note: these are typical examples, actual administration times may vary based on specific orders and patient needs.
Abbreviations Used in Prescriptions
Aa.: of each
Ad lib.: as much as desired
B.i.d. or b.d.: twice a day
t.d.s. or t.i.d.: three times a day
a.c.: before
P.c.: after
g.: gram
Gr.: grain
Gutt.: a drop
Mane: in the morning
Mist.: a mixture
Nocte: at night
q.h.: every hour
o.m.: every morning
o.n.: every night
p.r.n.:whenever necessary
q.4h: every 4 hours
s.o.s.: if necessary in an
emergency
Stat: immediately
q.i.d.: 4 times a day/every 6 hours
o.d.: once a day.
GENERAL RULES OF DRUG ADMINISTRATION
1. Read the instructions carefully and incase of any doubt ask the Doctor or ward in charge.
2. Never give a drug from a container or a bottle which is not clearly labeled.
3. Check the label against the instructions 3 times .The 1 st time before having the container, 2nd time before the drug is drawn, 3rd time before the drug
is administered to the patient.
4. Give the drug following 10Rs i.e -right patient, right time, right dose, right route, right drug/medication, right formulation, right disposal, right storage, right
equipment and right site.
5. Once a drug is drawn from its container it shouldn’t be returned.
6. Always identify the drug by reading its label on the container not by its color, smell, shape and size.
7. Do not transfer drugs to another container when the old label is still on.
8. Ask for clarification if any order regarding the dose is not readable.
9. Watch all patients for drug reactions, especially parental drugs.
10. If any drug changes its color, it should not be administered.
11. Liquid preparations should always be shaken before drawing from the bottles.
12. Never use a drug which has been left in an unlabeled container.
13. Always measure the dose of the drug in good light.
14. Observe strictly the time of administration of medication.
ORAL ADMINISTRATION
Essential Equipment
Medication Trolley:
Top Level:
Oral Liquid Medications: Assorted mixtures ready for dispensing.
Solid Oral Medications: Tablets and capsules in original containers/packaging.
Dosing Devices: Medicine cups for accurate liquid measurement.
Utensils for Crushing (if needed): Teaspoon, mortar and pestle for tablet manipulation.
Hydration Supplies: Jug of fresh drinking water, milk or fruit juice to aid swallowing.
Drinking Vessels: Glasses for patient fluid intake.
Medication Records: Patient-specific medication charts.
Small Tray: Dedicated tray to organise medications for individual patients.
Scissors: For opening medication packaging.
Waste Receptacle: Kidney dish for disposal.
Bottom Level:
Cleaning Solution: Bowl containing soapy water for equipment hygiene.
Patient Bedside:
Hand Hygiene Station: Equipment for hand washing (soap, water, paper towels or sanitiser).
Oral Medication Administration Procedure

PARENTERAL ROUTE (INJECTION)
Essential Supplies
Medication Trolley
Top Shelf:
Small Organising Tray: For efficient arrangement of items.
Sterile Injection Equipment: Syringes and needles in various sizes and capacities, appropriately selected for different injections.
Sterile Medications: Prescribed injectable drugs in sealed ampoules or vials.
Patient Documentation: Patient-specific medical charts and medication lists.
Swab Container: Gallipot holding sterile swabs.
Antiseptic Solution: Gallipot containing skin disinfectant.
Ampoule Opener: File for safely opening glass ampoules.
Sterile Diluent: Water for injection to reconstitute medications if needed.
Injection Trays/Dishes: Sterile trays to hold prepared syringes.
Tourniquet: To distend veins for intravenous access.
IV Cannula (if required): Appropriately sized cannula for intravenous injections/infusions.
Securement Dressing: Strapping or tape to secure dressings or cannulas.
Scissors: For dressing or tape manipulation.
Clean Gloves: For maintaining aseptic technique.
Bottom Shelf:
- Sharps Disposal Container: Safety box for immediate disposal of needles and sharps.
- Waste Container for Soiled Items: Receiver for used swabs and dressings.
- Waste Container for Used Gloves: Receiver specifically for disposable gloves.
- Arm Support: Small pillow to comfortably position the patient’s arm.
- Waterproof Sheet & Protective Layer: Macintosh and towel to protect bedding
Bedside Supplies
Privacy Screen: For patient modesty.
Hand Hygiene Station: Equipment for hand washing (soap, water, paper towels or sanitiser).
Procedure
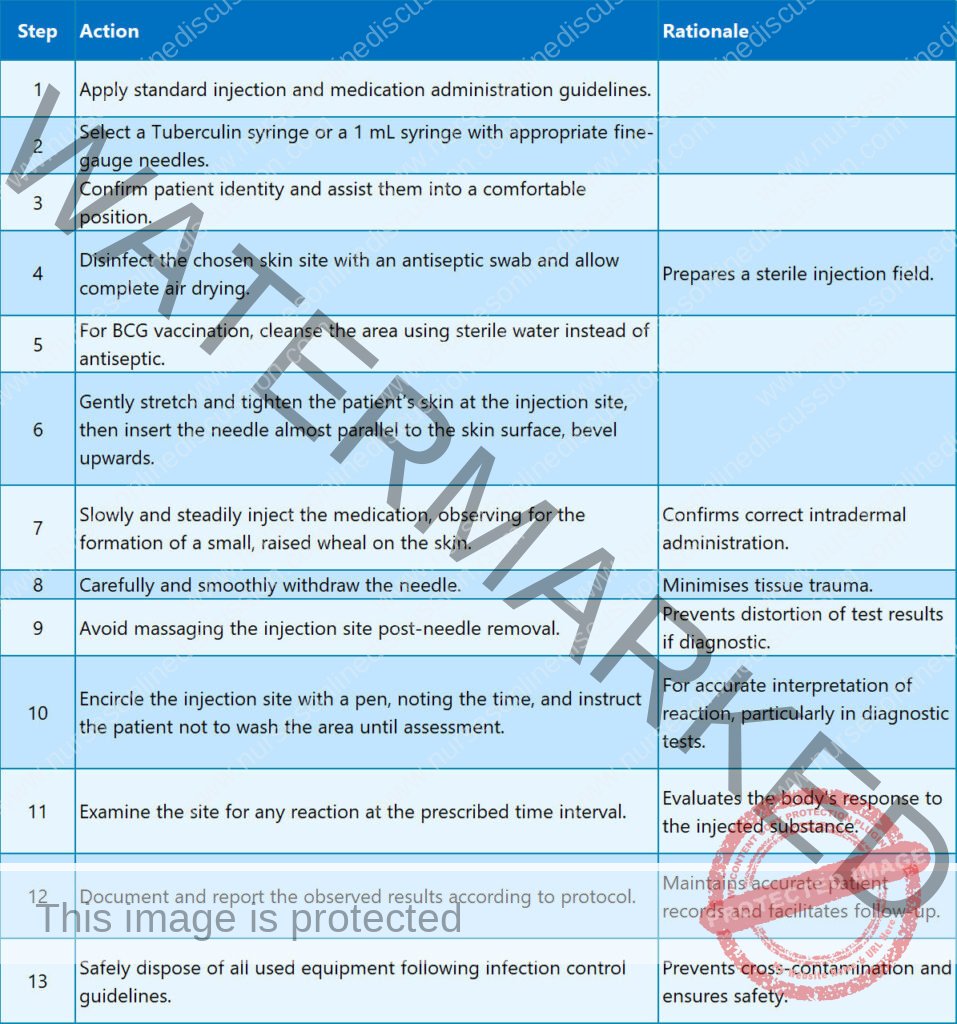
A. Intradermal or Intracutaneous Injection
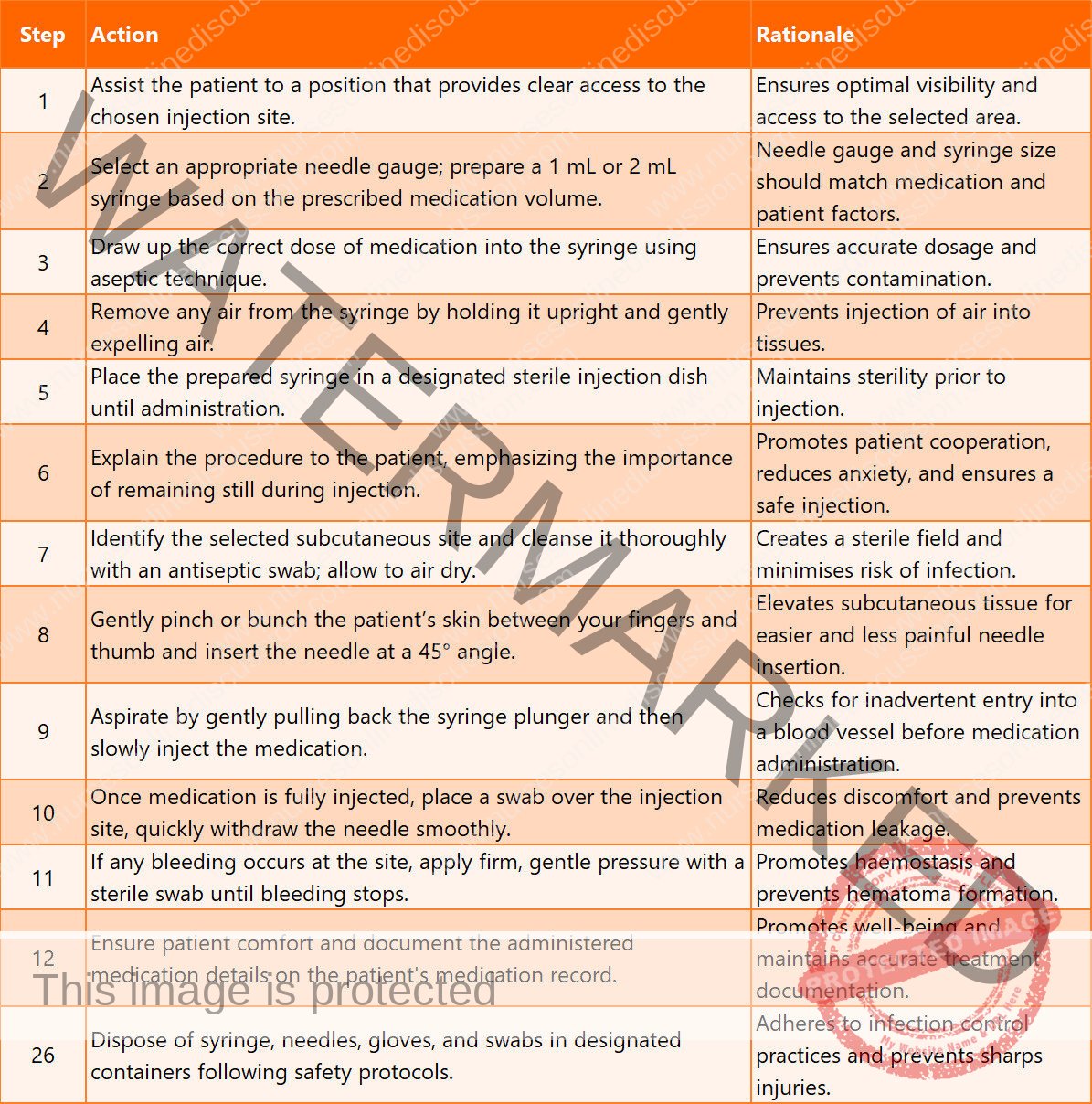
B. Subcutaneous Injection or Hypodermic
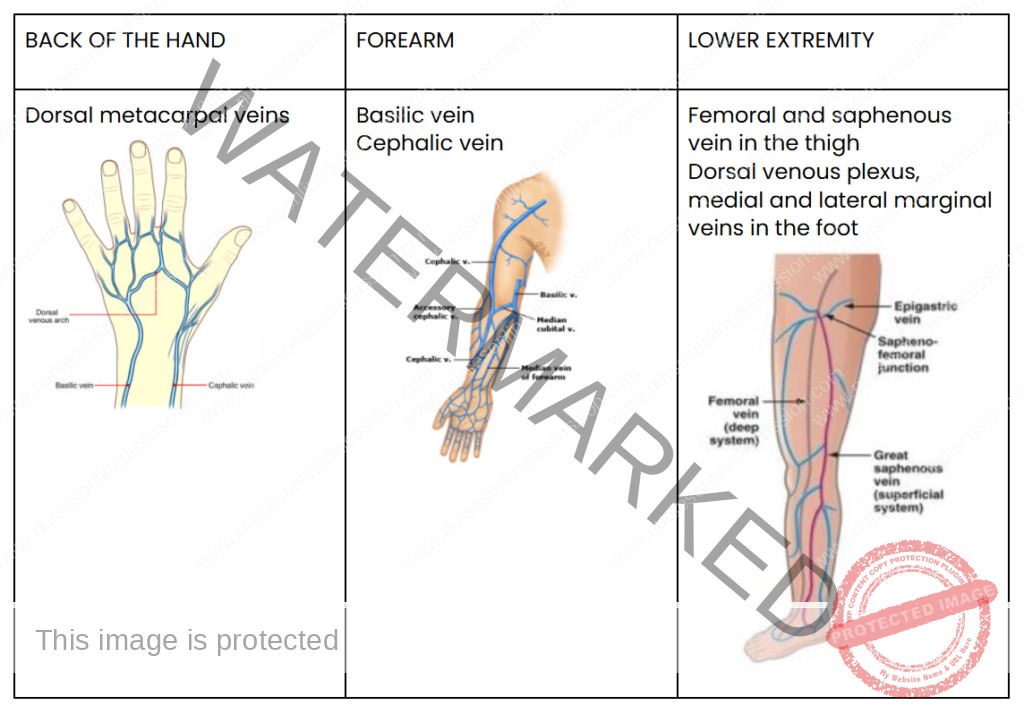
SOME OF THE RECOMMENDED VEINS FOR INTRAVENOUS INFUSION
COMPLICATIONS OF INTRAVENOUS INJECTIONS
Incorrect IV Placement: Accidental insertion of the IV catheter into an unintended vessel, such as an artery instead of a vein, can have serious negative health consequences.
Medication Administration Errors: Mistakes in drug identification, incorrect dosage calculation, or mixing incompatible medications can lead to significant adverse reactions in patients.
Rapid Infusion & Adverse Reactions: Delivering intravenous medications too quickly can overwhelm the body, potentially causing issues like low blood pressure (hypotension), irregular heartbeats (cardiac arrhythmias), allergic responses, and fluid overload.
Thrombophlebitis: Inflammation of the vein wall, frequently accompanied by blood clot formation, can arise from repeated IV access, poor insertion technique, or irritation from certain medications.
Fluid Overload (Circulatory Overload): Administering excessive intravenous fluids or infusing them too rapidly can overwhelm the circulatory system, leading to fluid accumulation and stress on the heart and lungs.
Embolism: Blockage of a blood vessel by a moving clot, air bubble, or foreign material. This can be a consequence of thrombophlebitis, improper IV insertion, or air entering the IV line.
Shock: A critical condition marked by severely reduced blood flow to vital organs, potentially triggered by severe allergic reactions, significant blood loss, or overwhelming infection (sepsis).
Infiltration/Extravasation: Leakage of IV fluids or medications out of the vein and into the surrounding tissues, causing localised pain, swelling, and possible tissue damage.
Phlebitis: Inflammation of a vein without clot formation, often caused by mechanical or chemical irritation from the IV catheter itself or the infused medication.
Air Embolism: Introduction of air into the bloodstream via the IV line, which can travel to the heart or lungs and create a blockage, possibly leading to breathing difficulties or cardiac arrest.
Catheter-Related Bloodstream Infection (CRBSI): A severe infection where bacteria gain entry to the bloodstream through the IV catheter, resulting in symptoms like fever, chills and potentially progressing to sepsis.
Nerve Injury: Damage to nearby nerves due to incorrect IV catheter placement can result in symptoms such as pain, numbness, or muscle weakness in the affected area.
Hematoma: Collection of blood in the tissues surrounding the IV puncture site, presenting as bruising or swelling.
Phlebosclerosis: Hardening or thickening of the vein wall due to repeated intravenous punctures or irritation from the indwelling catheter.
Common Sites for Intramuscular Injections
Gluteal Muscle (Buttock): The upper outer quadrant of the buttock is considered the safest location due to its distance from the sciatic nerve and major blood vessels.
Thigh Muscles (Vastus Lateralis/Rectus Femoris): The upper outer region of the thigh muscles provides a suitable site, especially in adults and children.
Deltoid Muscle (Upper Arm): The deltoid muscle in the upper arm can be used for smaller volume injections (up to 2 mL) only if the muscle is adequately developed. This site carries a higher risk of nerve injury and is generally avoided when other sites are available.
COMPLICATIONS OF INTRAMUSCULAR INJECTIONS
Abscess Formation: Development of a pus-filled cavity at the injection site, typically caused by non-sterile technique or when certain medications are not injected deeply enough into muscle tissue.
Prevention: Strict adherence to sterile procedures, proper needle selection for depth, and ensuring oily solutions are injected into deep muscle layers are critical preventive measures.
Nerve Injury: Damage to nerves in proximity to the injection site due to improper needle placement, potentially causing pain, sensory loss (numbness), weakness, or paralysis.
Prevention: Comprehensive understanding of anatomy, accurate identification of anatomical landmarks, and careful needle insertion techniques are essential to prevent nerve damage.
Tissue Damage/Necrosis: Injury and death of tissue cells at the injection site resulting from injecting excessive volumes of medication, using irritating substances, or repeated injections in the same area.
Prevention: Administering appropriate medication volumes, selecting less irritating formulations where possible, and consistently rotating injection sites can minimise tissue damage.
Hematoma: Formation of a bruise or swelling due to blood leakage into surrounding tissues from the injection site.
Prevention: Applying direct pressure to the injection site immediately after injection is a key step in preventing hematoma formation.
Pain and Discomfort: Intramuscular injections can cause pain, particularly if the medication is irritating or if the injection technique is not performed correctly.
Prevention: Employing proper injection technique, selecting an appropriate needle size, and allowing cold medications to warm to room temperature before injection can help reduce pain.
Allergic Reactions: Adverse immune responses to the injected medication or components of the medication solution.
Prevention: Thoroughly reviewing patient allergy history, performing allergy testing when indicated, and closely monitoring for any signs of allergic reaction after injection are crucial safety measures.
Injection into a Blood Vessel: Unintentional entry of the needle into a blood vessel during intramuscular injection, potentially leading to rapid drug absorption and complications like overdose or embolism.
Prevention: Aspirating (pulling back on the syringe plunger) before injecting is a standard practice to verify that the needle is not positioned within a blood vessel.
Delayed-Onset Muscle Soreness: Muscle pain, tenderness, or stiffness that may develop hours or even days after an intramuscular injection, often depending on the medication.
Prevention: There is no specific prevention, but advising patients to stay well-hydrated and avoid strenuous activity immediately following injection may be beneficial.
Infection: Infection at the injection site due to breaches in sterile technique during the injection process.
Prevention: Strict adherence to aseptic technique throughout the preparation and administration of intramuscular injections is paramount to prevent infection.
Air Embolism: Though rare, the introduction of air into the bloodstream during intramuscular injection can lead to serious complications such as respiratory distress or cardiac arrest.
Prevention: Using meticulous technique to ensure no air is drawn into the syringe or needle during medication preparation is essential to prevent air embolism.

Formula for Calculating Intravenous Drip Rate
To determine the intravenous (IV) drip rate, the following calculation is used:
Drip Rate (drops per minute) = (Total Volume in mL × Drop Factor) / Total Time in minutes
Example Calculation:
A physician orders 1200 mL of normal saline solution to be administered over 12 hours. The IV administration set has a drop factor of 15 drops per mL. Calculate the required drip rate in drops per minute.
Solution:
Total Volume: 1200 mL
Drop Factor: 15 drops/mL
Total Time in minutes: 12 hours × 60 minutes/hour = 720 minutes
Calculation:
Drip Rate = (1200 mL × 15 drops/mL) / 720 minutes
Drip Rate = 18000 drops / 720 minutes
Drip Rate ≈ 25 drops per minute
Therefore, the IV infusion should be regulated to approximately 25 drops per minute.
Factors Influencing Intravenous Infusion Flow Rate
Several factors can alter the intended flow rate of an intravenous infusion:
Infusion Solution Container Height: Elevating the IV fluid bag or bottle will increase the gravitational pressure, thus speeding up the infusion rate. Conversely, lowering the container will decrease the flow rate.
Infusion Set and Cannula Patency: Obstructions within the IV tubing or cannula, such as a blood clot formation, can significantly reduce or halt the infusion. This is more likely to occur if there are delays in replacing an empty fluid bag.
Tubing Kinks and Cannula Position: Bending or twisting of the IV tubing can impede flow. Similarly, if the cannula tip is positioned against the vein wall or has migrated out of the vein, the flow may be affected.
External Pressure (Tight Restraints): Applying external pressure, such as a tight bandage or splint situated above or at the IV insertion site, can compress the vein and restrict the infusion rate.
Air Vent Obstruction: If the air vent of the IV container is blocked, it creates a closed system and prevents air from entering as the fluid drains. This vacuum effect will stop the IV infusion.
Patient Care During Intravenous Infusion
Continuous monitoring and careful management are essential for patients receiving intravenous infusions:
Precise Documentation: Maintain a detailed record of the IV therapy. This includes noting the initiation time, the specific type of intravenous fluid, the total volume infused, and the prescribed infusion rate. This detailed record is crucial for tracking fluid balance and therapy progression.
Regular Patient Observation: Conduct frequent assessments of the patient’s condition to detect any adverse reactions or complications. Monitor for indicators such as pain at the insertion site, excessive sweating, restlessness or agitation, or any changes in vital signs that may suggest a problem. Prompt identification of issues is key to timely intervention.
Routine Insertion Site Examination: Regularly check the intravenous (IV) insertion site for any indications of fluid leakage into surrounding tissue (infiltration). Look for signs like swelling, coolness to touch, pain, or redness at the site, which may suggest fluid is not flowing correctly within the vein.
Consistent Patient Status Monitoring: Frequently assess and document the patient’s overall condition. This includes regularly measuring and recording vital signs (like heart rate, blood pressure, temperature, and respiratory rate), as well as observing for any new symptoms or changes in their general well-being. This ongoing monitoring helps to detect any complications or responses to the IV therapy.
Daily Site Hygiene: For prolonged intravenous infusions lasting multiple days, perform daily cleansing of the skin area surrounding the IV insertion point. Use sterile gauze and an appropriate antiseptic solution, following established protocols, to maintain cleanliness and reduce the risk of infection at the site.
Related Topics
- Wound dressing
- Colostomy Care
- Abdominal Paracentesis(Abdominal Tapping)
- Vulva Toilet/ Swabbing
- Oxygen Administration
- Lumbar Puncture
- Nasogastric tube to feed patients
- Gastrostomy Feeding
- Gastric Lavage
- Catheterization
- Tracheostomy Care
- Caring for patients in traction
- Prepare for application of orthopaedic splints
- Bandaging
- Nursing Process
- Take History of the patient
- Perform a physical examination of the Patient
- Making a Nursing Care Plan
- Admission of a patient
- Drug administration
- Transfer Patients
- Discharge of patients
- Last Office
We are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

