Obstetric Anatomy and Physiology
Gametogenesis (Oogenesis and Spermatogenesis)
Table of Contents
Introduction to Gametogenesis
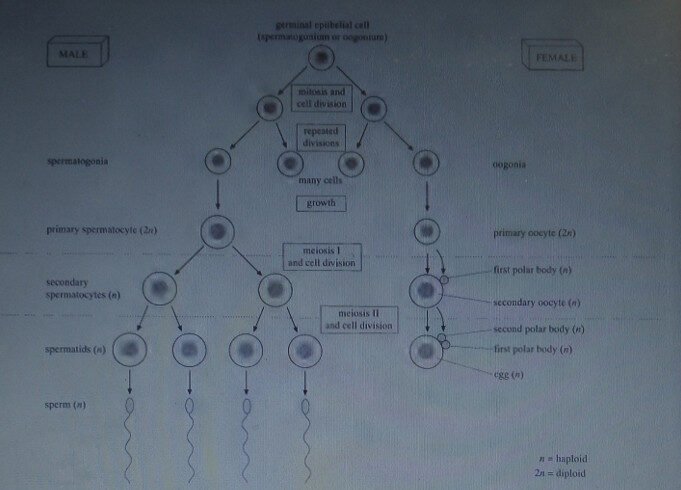
There are three main stages to reproduction: gametogenesis, fertilization, and the development of the embryo. Gametogenesis is the production of gametes, which is divided into spermatogenesis (production of sperm) and oogenesis (production of eggs).
Both processes take place in the gonads (testes in the male and ovaries in the female) and both involve meiosis, the nuclear division that halves the number of chromosomes from two sets (diploid condition) to one set (haploid condition). The cells which undergo meiosis are called mother cells (spermatocytes and oocytes).
Diagrammatic summary of spermatogenesis and oogenesis which emphasizes the main similarities and differences between the two processes.
Stages of Gametogenesis
Both spermatogenesis and oogenesis start with cells in the outer layer of the gonad, known as the germinal epithelium. Both processes involve three stages:
Multiplication Stage: Repeated mitotic divisions produce many spermatogonia and oogonia.
Growth Stage: A period of growth in preparation for the first meiotic division and cell division.
Maturation Stage: The first and second meiotic divisions occur, followed by the formation of mature haploid gametes.
The gametes produced will show variation as a result of independent assortment of chromosomes and crossing over during meiosis.
SPERMATOGENESIS
Sperm Development in Seminiferous Tubules
Sperm are produced in the seminiferous tubule of the testis at a rate of about 120 million per day, with the production of a given sperm taking about 70 days. The wall of the tubule has an outer layer of germinal epithelial cells and successive layers representing different developmental stages:
The first divisions of the germinal epithelial cells give rise to many spermatogonia.
Spermatogonia increase in size to form primary spermatocytes.
Primary spermatocytes undergo meiosis I to form haploid secondary spermatocytes.
Secondary spermatocytes undergo meiosis II to form spermatids.
Role of Sertoli Cells
Sertoli cells stretch from the outer layer of the tubule to the lumen (central space). They are essential because they:
Carry out the remoulding of spermatids to form mature sperm.
Facilitate the exchange of nutrients, oxygen, and waste substances between the developing sperm and the blood vessels.
Secrete the fluid carrying sperm through the tubules.
Spermatocytes become embedded in the infoldings of the Sertoli cell membranes and develop into spermatids before becoming mature sperm in the lumen. The entire process from spermatogonia to sperm takes about two months.
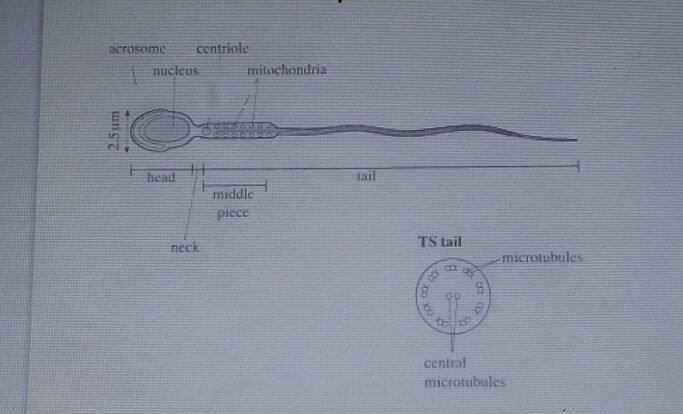
Microscopic Structure of the Sperm
Sperm are extremely small cells (about 50$\mu\text{m}$ long).
Part | Components and Function |
|---|---|
Head | Contains the nucleus (haploid chromosomes) and the acrosome. The acrosome is a large lysosome containing hydrolytic enzymes for penetrating the egg layers before fertilization. |
Neck | Contains a pair of centrioles. One centriole’s microtubules elongate to form the axial filament of the tail. |
Middle Piece | Enlarged by many mitochondria arranged in a spiral. They carry out aerobic respiration to produce ATP for the tail’s beating movements. |
The beating of the tail allows the sperm to swim at about 1-4mm per minute. Activation of the tail takes place in the vagina. The main function of the tail is to enable sperm to cluster around the oocyte, orientate themselves, and help in penetration.
HORMONAL CONTROL OF SPERMATOGENESIS
Overview of Control
Spermatogenesis is controlled by the hypothalamus and the anterior pituitary gland working together. The hypothalamus secretes gonadotropin-releasing hormone (GnRH), which travels to the anterior pituitary gland, stimulating it to secrete two gonadotropins (FSH and LH).
Roles of Gonadotropins and Testosterone
FSH (Follicle Stimulating Hormone): Stimulates Sertoli cells to complete the development of spermatozoa from spermatids.
LH (Luteinizing Hormone) / ICSH (Interstitial Cell Stimulating Hormone): Stimulates the synthesis of the steroid hormone Testosterone by the Leydig cells (interstitial cells) of the testis.
Testosterone: Stimulates the growth and development of the germinal epithelial cells (spermatogonia) and works with FSH on the Sertoli cells.
Negative Feedback
A negative feedback mechanism operates to regulate these hormones:
An increase in the level of Testosterone results in a decrease in secretion of GnRH from the hypothalamus (and possibly reduces LH secretion directly from the pituitary).
Inhibin, a glycoprotein hormone produced by the Sertoli cells, forms a second feedback inhibition system. If spermatogenesis proceeds too rapidly, Inhibin is released to reduce the secretion of FSH by the anterior pituitary gland.
Role of Cyclic AMP
Both FSH and LH act by causing the release of cyclic AMP (adenosine monophosphate) within the cells they stimulate. Cyclic AMP is known as the ‘second messenger’ system. It stimulates the synthesis of enzymes (e.g., enzymes for testosterone synthesis) inside the nucleus.
Secondary Sexual Characteristics
Testosterone is the main male sex hormone and controls the development and maintenance of secondary sexual characteristics that develop at puberty. These include:
Development and enlargement of the testes, penis, and reproductive tract glands.
Increased muscle development.
Enlargement of the larynx, causing deepening of the voice.
Growth of pubic, facial, armpit, and chest hair.
Changes in behavior associated with courtship and mating.
OOGENESIS
Development of Eggs
The production of eggs begins before birth (unlike sperm production).
During fetal development, oogonia undergo mitosis to form primary oocytes.
These primary oocytes halt development at prophase of meiosis I throughout childhood.
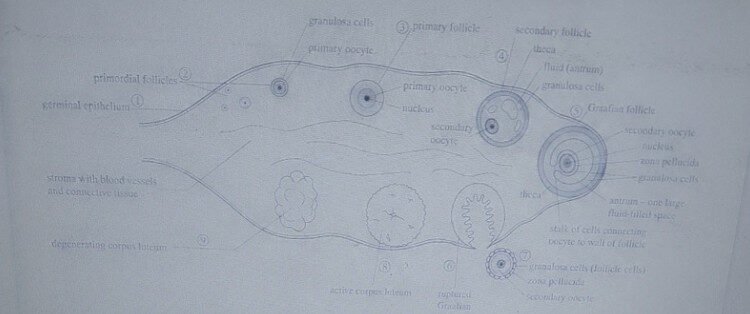
They are surrounded by a single layer of granulosa cells (or follicle cells), forming primordial follicles.
About two million primordial follicles exist just before birth, but only about 450 ever develop into the secondary oocytes that are released.
Follicle Development and Maturation
During a woman’s fertile years, one primordial follicle per month develops into a mature Graafian follicle in response to the hormone FSH.
The primordial follicle becomes a primary follicle as the granulosa cells multiply.
Cells from the ovary stroma form outer layers called the theca. The inner theca and granulosa cells secrete female sex hormones.
A fluid containing oestrogen is secreted by the granulosa cells, creating a fluid-filled space called the antrum (now a secondary follicle).
The follicle matures into a Graafian follicle (about 1 cm in diameter).
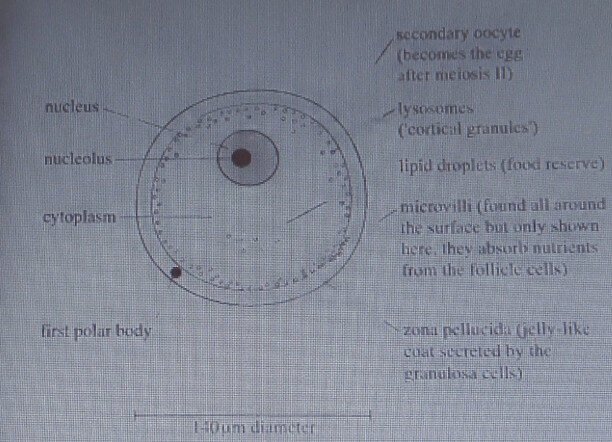
The primary oocyte divides by meiosis I, producing a secondary oocyte (haploid) and the first polar body.
The secondary oocyte arrests at metaphase of meiosis II until fertilization.
At fertilization, the secondary oocyte completes meiosis II, producing the large mature ovum and a second polar body. All polar bodies eventually degenerate.
Hormonal Control of Oogenesis
Control is centered in the hypothalamus and the pituitary gland.
The hypothalamus secretes GnRH, which stimulates the release of FSH and LH from the pituitary gland.
In the female, these hormones are secreted in cycles (menstrual cycle, lasting about 28 days), not constantly.
FSH stimulates the development of the primordial follicle each month.
Normally, only one egg is produced per cycle. The cycle begins on the first day of menstruation.
Structure of a secondary oocyte.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowWe are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

