Paediatrics II
Septicemia in Newborns
Table of Contents
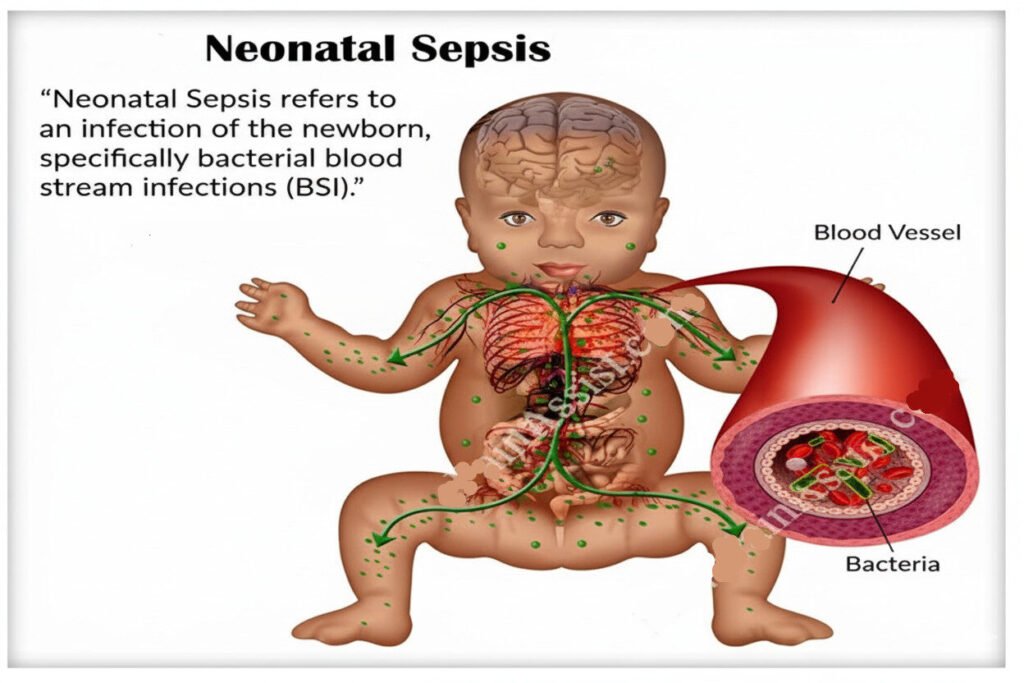
Definition
Septicemia, also known as neonatal sepsis, is a life-threatening condition characterized by the presence and multiplication of pathogenic microorganisms in the bloodstream, leading to the release of toxins that overwhelm the infant’s immature immune system. This can occur antenatally (before birth), intrapartum (during birth), or postnatally (after birth), and is a big contributor to neonatal mortality.
Causative Organisms Workflow
Pathogen Categories
- Gram-positive bacteria: Staphylococcus aureus, Streptococcus agalactiae (Group B Streptococcus), Listeria monocytogenes
- Gram-negative bacteria: Escherichia coli (E. coli), various other Enterobacteriaceae
- Other pathogens: Pneumococci (various Streptococcus pneumoniae serotypes) and other less common bacteria, fungi, or viruses.
Sites of Infection Workflow
Portals of Entry
Septicemia is often secondary to an initial infection at a specific site. Common portals of entry include:
- Broken Skin: Minor skin abrasions or lesions can provide easy access for bacteria.
- Umbilical Cord and Stump: The umbilical cord and its stump are particularly vulnerable to infection, especially with inadequate hygiene.
- Respiratory Tract: Pneumonia or other respiratory infections can lead to bloodstream invasion.
- Gastrointestinal Tract: Infections of the gut can disseminate bacteria into the circulation.
- Throat: Pharyngitis or other throat infections can serve as a source of bloodstream infection.
- Anus: Perianal infections can lead to septicemia.
Predisposing Factors Workflow
Risk Factors
Several factors increase the risk of neonatal septicemia:
- Prematurity: Premature infants have underdeveloped immune systems, making them highly susceptible to infections.
- Low Birth Weight: Infants with low birth weight are more vulnerable due to compromised immune function.
- Prolonged Rupture of Membranes: Prolonged rupture of the amniotic sac increases the risk of ascending infection.
- Chorioamnionitis: Infection of the amniotic fluid and placental membranes increases the risk of neonatal sepsis.
- Maternal Infections: Untreated maternal infections, such as urinary tract infections or sexually transmitted infections, can be transmitted to the newborn.
- Inadequate Hygiene: Poor hygiene practices during labor and delivery, and after birth, significantly increase the risk of infection.
- Use of Invasive Procedures: Procedures such as intubation or intravenous catheterization increase the risk of infection.
Signs and Symptoms Workflow
Clinical Manifestations
- Lethargy and Poor Feeding: The infant appears unusually sleepy, lethargic, and unwilling or unable to feed effectively.
- Temperature Instability: Temperature may be subnormal (hypothermia), normal, or elevated (pyrexia). Fluctuations are common.
- Irritability and Restlessness: The baby may be unusually fussy, irritable, and difficult to console.
- Gastrointestinal Disturbances: Vomiting and diarrhea can be present.
- Respiratory Distress: Rapid breathing, grunting, or nasal flaring may indicate respiratory involvement.
- Cyanosis: Bluish discoloration of the skin, particularly around the mouth and extremities, signifies low blood oxygen levels.
- Jaundice: Yellow discoloration of the skin and whites of the eyes indicates elevated bilirubin levels. This may or may not be related to the sepsis itself.
- Convulsions/Seizures: Seizures may occur in severe cases.
- Failure to Thrive: The infant fails to gain weight appropriately.
- Apnea: Episodes of cessation of breathing.
- Cold Extremities: Cool or mottled skin in the extremities may be present.
- Pus from the Umbilical Cord: Purulent discharge from the umbilical cord is a significant warning sign.
Management Workflow
Initial Management (Maternity Center)
While definitive management of septicemia requires hospitalization, immediate steps at the maternity center include:
- Temporary Admission and Isolation: Isolate the infant to prevent transmission to other newborns.
- Detailed History: Obtain a thorough maternal and neonatal history, including mode of delivery, onset of symptoms, and any known maternal infections.
- Initial Assessment: Record vital signs (temperature, pulse, respiration, blood pressure – TPRBP), and conduct a comprehensive physical examination, looking for signs of dehydration, anemia, jaundice, and umbilical cord infection.
- Supportive Care: Provide supportive care, including tepid sponging for fever, cleaning of the umbilical cord with normal saline (if indicated), and reassurance to the mother.
- Immediate Referral: Urgent referral to a hospital with neonatal intensive care capabilities is required.
- Empirical Antibiotics: Administer empirical antibiotic therapy, such as ampicillin or ceftriaxone (Give x-pen 25,000 units per kg / body weight 6 hourly or ampicillin until when the baby is taken to hospital), until the infant can receive appropriate care in a hospital.
Hospital Management
- Admission to Isolation Unit: The infant is admitted to an isolation unit to prevent further spread of infection.
- Detailed History and Examination: Complete the detailed history and conduct a thorough physical examination.
- Notification of Physician: Immediately inform the attending neonatologist or physician.
- Investigations: Order a range of laboratory investigations, including:
- Blood Cultures: At least two blood cultures are essential for identifying the causative organism.
- Complete Blood Count (CBC): To assess for anemia and infection.
- Blood Gases: To evaluate oxygenation and acid-base balance.
- Urineweek Culture: To rule out urinary tract infection.
- Umbilical Cord Culture: To identify potential pathogens.
- Nasopharyngeal and Throat Cultures: To detect upper respiratory tract infections.
- Cerebrospinal Fluid (CSF) Analysis: A lumbar puncture (LP) may be necessary to rule out meningitis.
- Other Investigations: Further imaging or tests may be needed depending on the clinical presentation.
- Definitive Antibiotic Therapy: Once the causative organism is identified (via culture and sensitivity testing), definitive antibiotic therapy is initiated.
- For Group B Streptococcus and E. coli: A typical course might involve ampicillin (50 mg/kg IV every 6 hours for 5-7 days) in combination with gentamicin (5 mg/kg/day IV once daily for 5-7 days).
- For Staphylococcus aureus: Cloxacillin (dosage adjusted to body weight and administered intravenously) is often prescribed.
- Broad-spectrum coverage: Ceftriaxone (dosage adjusted to body weight and administered intravenously) may be used for broader coverage, especially initially, while awaiting culture results.
- Ampicillin: Effective against many gram-positive and some gram-negative bacteria.
- Gentamicin: Effective against gram-negative bacteria.
- Cefotaxime or Ceftriaxone: Broad-spectrum antibiotics effective against a wide range of bacteria.
- Vancomycin: Used for serious infections caused by methicillin-resistant Staphylococcus aureus (MRSA) The duration of antibiotic therapy is usually 7-10 days. However, treatment may be shortened to 5 days if the infant remains afebrile (without fever) and shows clinical improvement.
- Supportive Care:
- Fluid Management: Intravenous fluids (e.g., half-strength Darrow’s solution) are administered to correct dehydration.
- Respiratory Support: Oxygen therapy or mechanical ventilation may be necessary for respiratory distress.
- Nutritional Support: Parenteral nutrition or nasogastric tube feeding may be required if the infant cannot feed orally.
- Anticonvulsants: Anticonvulsant medications may be necessary to control seizures.
- Blood Transfusions: Blood transfusions are given if anemia is present.
Nursing Care Workflow
Comprehensive Nursing Interventions
Comprehensive nursing care is vital in managing neonatal septicemia:
- Strict Bed Rest: Maintain the infant on strict bed rest.
- Nasogastric Tube Feeding: Provide nutritional support through nasogastric tube feeding with expressed breast milk (EBM) if oral feeding is impossible.
- Strict Hygiene: Maintain meticulous hygiene practices, including frequent handwashing and careful cleaning of the umbilical cord.
- Vital Signs Monitoring: Closely monitor vital signs regularly (at least every 2-4 hours).
- Fluid and Electrolyte Balance: Monitor fluid intake and output closely.
- Oxygen Saturation: Monitor oxygen saturation levels.
- Daily Assessments: Conduct daily physical assessments, noting any changes in condition.
- Skin Care: Ensure appropriate skin care to prevent breakdown.
- Parental Support: Provide emotional support and education to the parents.
Prognosis Workflow
Outcome Factors
The prognosis for neonatal septicemia depends on several factors, including the causative organism, the timeliness of diagnosis and treatment, and the infant’s overall health status. Early diagnosis and appropriate treatment significantly improve survival rates. Delayed treatment and inadequate supportive care are associated with increased mortality and morbidity.
Prevention Workflow
Multi-Pronged Prevention Approach
Prevention of neonatal septicemia requires a multi-pronged approach focusing on maternal and neonatal care:
Antenatal Care
- Regular antenatal check-ups are crucial for early detection and management of maternal infections, such as urinary tract infections, sexually transmitted infections, and chorioamnionitis. This includes appropriate testing and treatment as needed.
Intrapartum Care
- Appropriate Hygiene: Strict adherence to hygienic practices during labor and delivery is paramount. This includes handwashing by healthcare providers, proper cleaning and disinfection of equipment, and maintaining a clean birthing environment.
- Prophylactic Antibiotics: In cases of prolonged rupture of membranes or suspected chorioamnionitis, prophylactic antibiotics may be administered to the mother to reduce the risk of transmission to the newborn.
- Careful Monitoring: Close monitoring of the mother and fetus during labor and delivery helps to identify any signs of infection early.
- Timing of Delivery: Appropriate timing of delivery (e.g., cesarean section in cases of severe maternal infection) can help prevent neonatal sepsis.
Postnatal Care
- Umbilical Cord Care: Meticulous umbilical cord care is essential to prevent infection. This includes keeping the area clean and dry, and avoiding the use of antiseptic solutions that may delay healing.
- Breastfeeding: Breastfeeding provides passive immunity through colostrum and breast milk, helping to protect the newborn from infections. Proper latch techniques help prevent nipple trauma and subsequent infection.
- Hand Hygiene: Strict hand hygiene practices are crucial for everyone caring for the newborn.
- Early Detection and Treatment of Infections: Prompt recognition and treatment of any signs of infection in the newborn are crucial for preventing sepsis. Any signs of lethargy, poor feeding, temperature instability, or other concerning symptoms should be reported immediately to a healthcare provider.
- Skin Care: Maintaining the integrity of the skin is important to prevent entry of pathogens.
Immunizations and Education
- Immunizations: Maternal immunization against certain infections, such as influenza and pertussis, can help protect the newborn from these pathogens.
- Education: Educating parents and healthcare providers about the risk factors, signs, and symptoms of neonatal septicemia is crucial for early detection and intervention. Emphasis should be placed on the importance of antenatal care, hygienic practices, and timely medical attention.
Discharge and Complications Workflow
Discharge Criteria
Before discharge, the infant should meet several criteria indicating resolution of septicemia and stability:
- Resolution of Clinical Symptoms: The infant should be clinically well, with resolution of fever, lethargy, poor feeding, and other symptoms. This often requires several days of symptom-free observation.
- Negative Blood Cultures: At least two consecutive negative blood cultures are typically required, taken 24 hours apart after antibiotic therapy has begun.
- Stable Vital Signs: Vital signs (temperature, heart rate, respiratory rate, blood pressure) should be within the normal range for the infant’s age and gestational age.
- Adequate Feeding: The infant should be feeding well, either orally or via other methods as needed. Weight gain should be progressing appropriately.
- Absence of Organ Dysfunction: Evidence of organ dysfunction (e.g., respiratory distress, jaundice, seizures) should have resolved.
- No Evidence of Ongoing Infection: There should be no evidence of any ongoing infection at the site of initial infection (e.g., umbilical cord, skin).
Potential Complications
Short-Term Complications
- Respiratory Distress Syndrome (RDS): Sepsis can lead to respiratory failure requiring supplemental oxygen or mechanical ventilation.
- Apnea: Periods of cessation of breathing.
- Meningitis: Infection of the meninges (protective membranes surrounding the brain and spinal cord).
- Disseminated Intravascular Coagulation (DIC): A serious clotting disorder.
- Gastrointestinal Bleeding: Bleeding from the gastrointestinal tract.
- Hypotension: Low blood pressure.
- Shock: A life-threatening condition characterized by inadequate blood flow to the body’s tissues.
- Death: In severe cases, despite treatment, septicemia can be fatal.
Long-Term Complications
- Developmental Delay: Sepsis can cause developmental delays in cognitive, motor, and language skills.
- Hearing Loss: Hearing impairment may occur as a result of meningitis or other complications.
- Cerebral Palsy: In severe cases, cerebral palsy may develop due to brain damage from the infection.
- Blindness: Severe cases can lead to visual impairment.
- Neurological Deficits: A range of neurological problems can occur, including seizures, intellectual disability, and behavioral issues.
Nursing Care Plan Workflow
Assessment Data
Subjective Data
- Parents report that the baby appears lethargic
- Feeding difficulties
- Mother reports baby is not feeding well
- Parents express concern about the baby’s condition
Objective Data
- Poor sucking reflex
- Lethargy and irritability
- Fever or hypothermia
- Respiratory distress (tachypnea, grunting)
- Hypotension
- Jaundice or pallor
- Poor feeding
- Weight loss or failure to gain weight
- Pale skin and mucous membranes
- Prolonged capillary refill
- Low urine output (oliguria)
- Respiratory distress (tachypnea, grunting, nasal flaring)
- Cyanosis
- Parents appear anxious and ask frequent questions
Nursing Diagnosis: Infection
Infection related to immature immune system and exposure to pathogens as evidenced by lethargy, feeding difficulties, and temperature instability
Goals/Expected Outcomes
The neonate will demonstrate signs of infection control, such as stable temperature, improved feeding, and decreased lethargy within 48 hours of intervention
Interventions
- Administer prescribed antibiotics based on blood culture results
- Monitor vital signs, especially temperature and respiratory rate, every 2-4 hours
- Assess feeding patterns and encourage frequent feedings
- Perform hand hygiene before and after handling the neonate
- Isolate the neonate if necessary to prevent cross-infection
Rationale
- Antibiotics target the causative organism
- Regular monitoring detects early signs of deterioration or improvement
- Encouraging feeding helps maintain nutrition and hydration
- Hand hygiene prevents the spread of infection
- Isolation protects the neonate from further exposure to pathogens
Evaluation
The neonate shows stable vital signs, improved feeding, and decreased lethargy, indicating effective infection control
Nursing Diagnosis: Imbalanced Nutrition
Imbalanced Nutrition: Less Than Body Requirements related to infection and poor feeding as evidenced by poor sucking reflex and weight loss
Goals/Expected Outcomes
The neonate will achieve adequate nutrition as evidenced by regular feedings and weight gain within 72 hours of intervention
Interventions
- Monitor daily weight and record intake/output
- Encourage breastfeeding or administer expressed breast milk
- Administer IV fluids or parenteral nutrition if oral intake is insufficient
- Provide a quiet and calm environment during feedings
Rationale
- Monitoring weight and intake/output assesses nutritional status
- Breast milk provides essential nutrients and immune protection
- IV fluids prevent dehydration and maintain electrolyte balance
- A calm environment promotes successful feeding
Evaluation
The neonate shows improved feeding patterns, weight gain, and stabilized intake/output levels
Nursing Diagnosis: Decreased Cardiac Output
Decreased Cardiac Output related to septic shock as evidenced by hypotension, oliguria, and prolonged capillary refill
Goals/Expected Outcomes
The neonate will maintain adequate tissue perfusion as evidenced by improved urine output, normal capillary refill, and stable blood pressure
Interventions
- Administer IV fluids and vasopressors as prescribed
- Monitor urine output, ensuring it is >1mL/kg/hour
- Monitor capillary refill, pulse, and blood pressure every 2 hours
- Assess for signs of fluid overload
Rationale
- IV fluids and vasopressors increase cardiac output and tissue perfusion
- Monitoring urine output assesses kidney function and fluid balance
- Regular assessment of capillary refill and vital signs detects signs of improved perfusion or shock
- Monitoring for fluid overload prevents complications of excessive fluid therapy
Evaluation
The neonate shows improved urine output, capillary refill within 2 seconds, and stable blood pressure, indicating improved tissue perfusion
Nursing Diagnosis: Ineffective Breathing Pattern
Ineffective Breathing Pattern related to infection and sepsis as evidenced by tachypnea and grunting
Goals/Expected Outcomes
The neonate will demonstrate an effective breathing pattern with a respiratory rate within the normal range and no signs of respiratory distress within 24 hours
Interventions
- Administer oxygen therapy via nasal cannula or CPAP as prescribed
- Monitor respiratory rate, effort, and oxygen saturation every 2 hours
- Position the neonate in a semi-Fowler’s position to ease breathing
- Suction secretions as needed to maintain a clear airway
Rationale
- Oxygen therapy improves oxygenation and prevents hypoxia
- Frequent monitoring of respiratory parameters detects changes in condition
- Proper positioning facilitates lung expansion and eases breathing
- Suctioning removes secretions that may obstruct the airway
Evaluation
The neonate demonstrates a normal respiratory rate, improved oxygen saturation, and no signs of respiratory distress
Nursing Diagnosis: Anxiety (Parental)
Anxiety (Parental) related to the critical condition of the neonate as evidenced by
Goals/Expected Outcomes
Parents will verbalize reduced anxiety and demonstrate understanding of the neonate’s condition and treatment plan within 24 hours
Interventions
- Provide clear information about the neonate’s condition and treatment plan
- Offer emotional support and answer questions
- Encourage parents to participate in the neonate’s care
- Refer parents to support groups if needed
Rationale
- Information helps reduce anxiety by providing clarity
- Emotional support reassures the parents and helps them cope
- Involving parents in care gives them a sense of control and strengthens bonding
- Support groups provide additional emotional resources
Evaluation
Parents verbalize understanding of the neonate’s condition, express reduced anxiety, and participate in care
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowWe are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

