Anatomy & Physiology I
Subtopic:
Cardiovascular System

Learning Objectives
🫀 Cardiovascular System Overview
- Identify the three components of the cardiovascular system: blood, heart, and blood vessels.
- Explain the heart’s structure and location, including layers (endocardium, myocardium, epicardium).
🫁 Heart Chambers & Valves
- Describe the internal anatomy of the heart, including septa, atria, ventricles, and valve function.
- Differentiate between atrioventricular and semilunar valves, including flow direction and valve mechanics.
🔁 Cardiac Physiology
- Trace the cardiac conduction system, identifying nodes and conduction pathways.
- Explain the cardiac cycle, including systole and diastole phases and timing.
- Define cardiac output and stroke volume, and relate them to physiological function.
🔊 Heart Sounds & Arrhythmias
- Identify normal heart sounds (lubb-dupp) and describe types of murmurs.
- Define and distinguish bradycardia, tachycardia, and arrhythmias.
🩺 Vital Signs: Pulse & Blood Pressure
- Describe pulse characteristics (rate, rhythm, volume, tension), terminology, and measurement sites.
- Define blood pressure and list factors influencing it (e.g., viscosity, contraction force).
🧠 Blood Vessel Structure & Classification
- Classify blood vessels by function, including arteries, veins, capillaries, arterioles, and venules.
- Describe the structural differences among vessels, including layers, valves, and muscle thickness.
THE BLOOD
Blood is classified as a connective tissue, since nearly half of it is made up of cells. However, it differs from other connective tissues in that its cells are not fixed in position, instead they move freely in the liquid portion of the blood, the plasma.
Blood is a viscous (thick) fluid that varies in colour from bright to dark red, depending on how much oxygen it is carrying. Its quantity differs with the size of the person; the average adult male, weighing 70 kg has about 5-6 litres of blood.
This volume accounts for about 8% of the total body weight. It is carried through a closed system of vessels pumped by the heart. The circulating blood is of fundamental importance in maintaining the internal environment in a constant state (homeaostasis).
Characteristics of Blood
- Colour: bright red is well oxygenated eg that from the artery. Dark red when de-oxygenated eg that from the vein.
- Quantity. Approximately 7% of body weight.
- Erythrocyte Sedimentation rate (ESR); Separation of blood from plasma Rages from 4-10m/hr
- Reaction (PH) slightly alkaline 7.35-7.
Functions of the Blood
Transportation
- Oxygen- from inhaled air diffuses into the blood through the thin lung membranes and is carried to all the tissue of the body. Carbon dioxide, a waste product of cell metabolism, is carried from the tissues to the lungs, where it is breathed out.
- The blood transports foods and other needed substances such as minerals and vitamins, to the cells. These materials may inter the blood from the digestive system or may be released into the blood from body stores.
- The blood transports waste products from the cells to the sites from which they are released. The kidney removes excess water, minerals, and urea from protein metabolism and maintains the acid-base balance of the blood. The liver removes bile pigments and drugs.
- The blood carries hormones from their sites of origin to the organs they affect.
Regulation
- Buffers in the blood help keep the PH of body fluids at about 7.4
- The blood serves to regulate the amount of fluid in the tissues by means of substances (mainly proteins) that maintain the proper osmotic pressure
- The blood transports heat that is generated in the muscles to other parts of the body thus aiding in the regulation of body temperature by the blood, thus aiding in the regulation of body temperature.
Protection
- The blood carries the cells that are among the body’s defenders against pathogens. It also contains substances (antibodies) that are concerned with immunity to disease.
- The blood contains factors that protect against blood loss.
Composition of Blood
The blood is composed of two prime elements: the liquid element is called plasma; the cells and fragments of cells are called formed elements or corpuscles
Plasma making 55% of blood, Cells suspended in plasma consists of 45% of blood.
The formed elements are classified as follows:
- Erythrocytes, from erythro, meaning “red,” are the red blood cells, which transport oxygen.
- Leukocytes, from leuko, meaning “white,” are the several types of white blood cells, which protect against infection.
- Platelets, also called thrombocytes, are cell fragments that participate in blood clotting
BLOOD PLASMA
Over half of the total volume of blood is plasma. The plasma itself is 90% water. Many different substances dissolved or suspended in the water, make up the other 10%. The plasma content varies somewhat, since the substances carried by the blood to and from the organs get used and added to. However, the body tends to maintain a fairly constant level of these substances. For example, the level of glucose, a simple sugar, is maintained at a remarkably constant level of about a 10nth of a 1% solution.
After water, the next largest percentage of material in the plasma is protein. Proteins are the principal constituents of cytoplasm and are essential to the growth and the rebuilding of body tissues.
Plasma proteins
These make up about 7% of plasma, are normally retained within blood, because they are too big to escape through the capillary pores into the tissues.
Functions
- They are largely responsible for creating the osmotic pressure of blood, which keeps plasma fluid within circulation.
- If plasma protein levels fall, because of either reduced production or loss from the blood vessels, osmotic pressure is also reduced, and fluid moves into the tissues (oedema) and body cavities.
- Plasma visconsity (thickens) is due to plasma proteins, mainly albumin and fibrinogen.
- Alblumins: These are the most abundant plasma proteins (about 60% of total). Their main function is to maintain normal plasma osmotic pressure
- They also act as carrier molecules for free falty acids, some drugs and stevoid hormones.
- Albumin, the most abundant protein in plasma, is important for maintaining the osmotic pressure of the blood. This protein is manufactured in the liver.
- The antibodies combat infection.
- The blood clotting factors are also manufactured in the liver.
- A system of enzymes made of several proteins, collectively known as complement, helps antibodies in their fight against pathogens.
Nutrients also found in the plasma:
carbohydrates. The principal form of carbohydrate found in the plasma is glucose, which is absorbed by the capillaries of the intestine following digestion. Glucose is stored mainly in the liver as glycogen and released as needed to supply energy.
Amino acids, the products of protein digestion, are also found in the plasma. These are also absorbed into the blood through the intestinal capillaries.
Lipids constitute a small percentage of blood plasma. Lipids include fats. They may be stored as fat for reserve energy or carried to the cells as a source of energy.
The mineral salts in the plasma appear primarily as chloride, carbonate, or phosphate salts of sodium, potassium, and magnesium. These salts have a variety of functions, including the formation of bone (calcium and phosphorus), the production of hormones by certain glands (iodine for the production of thyroid hormone), the transportation of the gases oxygen and carbon dioxide (iron), and the maintenance of the acid base balance (sodium and potassium carbonates and phosphates).
Small amounts of other elements also help maintain homeostasis: Many other materials, such as waste products and hormones, are also transported in the plasma.
THE FORMED ELEMENTS (cellular part of blood)
Erythrocytes
Erythrocytes, the red cells, are tiny, disk-shaped bodies with a central area that is thinner than the edges. They are different from other cells in that the mature form found in the circulating blood does not have a nucleus. These cells, like almost all the blood cells, live a much shorter time (120 days) than most other cells in the body, some of which last a lifetime. One purpose of the red cells is to carry oxygen from the lungs to the tissues. The oxygen is bound in the red cells to haemoglobin, a protein that contains iron.
Haemoglobin combined with oxygen gives the blood its characteristic red color. The more oxygen carried by the haemoglobin, the brighter is the red color of the blood.
Therefore, the blood that goes from the lungs to the tissues is a bright red because it carries a great supply of oxygen; in contrast, the blood that returns to the lings is a much darker red, since it has given up much of its oxygen to the tissues.
Haemoglobin that has given up its oxygen is able to carry hydrogen ions; in this way, haemoglobin acts as a buffer and plays an important role in acid-base balance. The red cells also carry a small amount of carbon dioxide from the tissues to the tlings for elimination in exhalation.
Carbon monoxide is a harmful gas that combines with haemoglobin to form a stable compound. It displaces the oxygen that is normally carried by the haemoglobin and reduces the oxygen-carrying ability of the blood. Carbon monoxide may be produced by the incomplete burning of various fuels, such as gasoline, coal, wood, and other carbon containing materials. It also occurs in automobile exhaust fumes and in cigarette smoke.
The erythrocytes are by far the most numerous of the corpuscles, averaging from 4.5 to 5 million per cubic millimeter of blood.
Leukocytes
The leukocytes, or white blood cells, are very different from the erythrocytes in appearance, quantity, and function. They contain nuclei of varying shapes and sizes; the cells themselves are round. Leukocytes are outnumbered by red cells by 700 to 1, numbering 5,000 to 10,000 per cubic millimetre of blood.
Whereas the red cells have a definite color, the leukocytes tend to be colorless.
The different types of white blood cells are identified by their size, the shape of the nucleus, and the appearance of granules in the cytoplasm when the cells are stained, usually with Wright’s blood stain.
Granulocytes include neutrophils, which show lavender granules; eosinophils, which have beadlike, bright pink granules; and basophils, which have large, dark blue granules that often obscure the nucleus.
The neutrophils are the most numerous of the white cells, constituting up to 60% of all leukocytes.
Because the nuclei of the nuclei of the neutrophils are of various shapes, they are also called polymorphs (meaning “many forms”)
The agranulocytes, so named because they lack easily visible granules, are the lymphocytes and monocytes.
The most important function of the leukocytes is to destroy pathogens. Whenever pathogens enter the tissues, as through a wound, certain white blood cells (neutrophils and monocytes) are attracted to that area. They leave the blood vessels and proceed by ameboid or ameba-like motion to the area of infection.
There they engulf the invaders by a process called phagocytosis. If the pathogens are extremely strong or numerous, they may destroy the leukocytes.
A collection of dead and living leukocytes, forms pus. A collection of pus localized in one area is known as abscess.
The Lymphocytes destroy foreign invaders by attacking the cells directly or by producing antibodies that circulate in the blood and help destroy the cells.
Platelets
Of all the formed elements, the blood platelets (thrombocytes) are the smallest (Figure 9-1). These tiny structures are not cells in themselves, but fragments of cells. The number of platelets in the circulating blood has been estimated at 200, 000 to 400,000 per cubic millimeter. Platelets are essential to blood coagulation (clotting). When, as a result of injury, blood comes in contact with any tissue other than the lining of the blood vessels, the platelets stick together and form a plug that seals the wound. They then release chemicals that take part in a series of reactions that eventually results in the formation of a clot. The last step in these reactions is the conversion of a plasma protein called fibrinogen into solid threads of fibrin, which form the clot.
Blood Clotting
Blood clotting, or coagulation, is a protective device that prevents blood loss when a blood vessel is ruptured by an injury. The many substances necessary for clotting are normally inactive in the blood stream. A balance is maintained between compounds that promote clotting, known as procoagulants, and those that prevent clotting known as anticoagulants. In addition, there are also chemicals in the circulation that act to dissolve clots. Under normal conditions the substances that prevent clotting prevail.
However, when an injury occurs, the procoagulants are activated and a clot is formed.
Basically, the clotting process consists of the following essential steps:
- The injured tissues release thromboplastin, a substance that triggers the clotting mechanism.
- Thromboplastin reacts with certain protein factors and calcium ions to form prothrombin activator, which in turn reacts with calcium ions to convert the prothrombin to thrombin.
- Thrombin, in turn, converts soluble fibrinogen into insoluble fibrin. Fibrin forms a network of threads that entraps red blood cells and platelets to form clot.
Formation of a clot.
Thromboplastin
Ca++
Prothrombin – Thrombin- Fibrinogen – Fibrin threads
+ Blood cells and plasma
Clot
ABO BLOOD GROUP SYSTEM
- If for some reason the amount of blood in the body is severely reduced, through haemorrhage or disease, the body cells suffer from lack of oxygen and food. The obvious measure to take in such an emergency is to inject blood from another person into the veins of the patient, a procedure called transfusion.
- The patient’s plasma may contain substances called antibodies that can cause the red cells of the donor’s blood to become clumped, a process called agglutination. Alternatively, donor’s red blood cells may rupture and release their haemoglobin; such cells are said to be haemolysed, and the resulting condition can be very dangerous.
- These reactions are determined largely by certain proteins, called antigens, on the surface membrane of the red blood cells.
- There are many types of these proteins but only two groups are particularly likely to cause a transfusion reaction, the so-called A and B antigens and the Rh factor.
- Four blood types involving the A and B antigens have been recognized: A, B, AB, and O. these letters indicate the types of antigen present on the red cells, with O indicating that neither A nor B antigen is present. It is these antigens to the donor’s red fells that react with the antibodiesin the patient’s plasma and cause a transfusion reaction.
- Blood serum containing antibodies that can agglutinate and destroy red cells that have A antigens on the surface is called anti-A serum; blood serum containing antibodies that can destroy red cells with B antigen on the surface is called anti-B serum. These sera are used to test for blood type.
- Persons with type O blood are said to be universal donors because they lack the AB red cell antigens and in an emergency their blood can be given to anyone. Type AB individuals are called universal recipients, since their blood contains no antibodies to agglutinate red cells and they can therefore receive blood from most donors.
- Usually a person can safely give blood to any person with the same blood type. However, because of other factors that may be present in the blood, determination of blood type must be accompanied by additional tests (cross matching) for compatibility before a transfusion is given.
The Rh factor
Rh factor is another red cell antigen that determines the blood group. Those individuals who possess this antigen in their red cell surface are said to be Rh positive. Those who lack this antigen are said to be Rh negative. If Rh positive blood is given to an Rh negative person, he or she may become sensitized to the protein in the Rh positive blood. The sensitized person’s blood cells may then produce antibodies to the “foreign” Rh antigens and destroy the transfused red cells.
A pregnant woman who is Rh negative may become sensitized by proteins from her Rh positive fetus (this factor having been inherited from the father) if these proteins enter the mother’s circulation before or during childbirth. During a subsequent pregnancy with an Rh positive fetus, some of the anti Rh antibodies may pass from the mother’s blood in to the blood of her fetus and cause destruction of the fetus’s red cells. This condition is called erythroblastosis fetalis, or hemolytic disease of the newborn.
Erythroblastosis fetalis may be prevented by administration of immune globulin Rho (D), ofr RhoGAM, to the mother shortly after delivery. This destroys the Rh-positive fetal cells in the mother’s blood and prevents her sensitization.
CARDIOVASCULAR SYSTEM
The cardiovascular system is the transport system of the body by which food, oxygen, water and all other essentials are carried to the tissue cells and their waste products are carried away. It consists of three parts:
- The blood, which is the fluid in which materials are carried to and from the tissue
- The heart, which is the driving force which propels the blood
- The blood vessels, the routes by which the blood travels to and through the tissues and back to the heart.
The Heart
The heart is a muscular pump that drives the blood through the blood vessels. Slightly bigger than a fist, this organ is located between the lungs in the center (mediastinum) and a bit to the left on the midline of the body.
Structure of the Heart
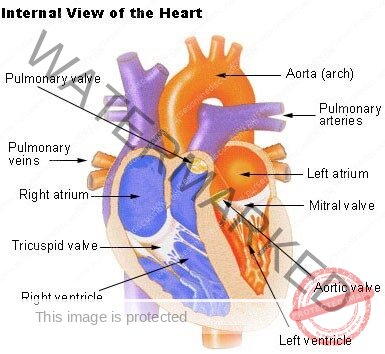
The heart is a hollow organ the walls of which are formed of three different layers. The heart wall has three tissue layers;
- The endocardium is a very thin smooth layer of cells that resembles squamous epithelium. This membrane lines the interior of the heart. The valves of the heart are formed by reinforced folds of this material.
- The myocardium, the muscle of the heart, is the thickest layer.
- The epicardium forms the thin outermost layer of the heart wall and is continuous with the serous lining of the fibrous sac that encloses the heart. These membranes together make up the pericardium. The serous lining of the pericardial sac is separated from the epicardium on the heart surface by a thin fluid- filled space.
Two Hearts and a Partition
Physicians often refer to the right heart and the left heart. This is because the human heart is really a double pump. The two sides are completely separated from each other by a partition called the septum. The upper part of this partition is called interatrial septum; while the larger the lower portion is called interventricular septum. The septum, like the heart wall, consists largely of myocardium.
On either side of the heart are two chambers, one a receiving chamber (atrium) and the other a pumping chamber (ventricle):
- The right atrium is a thin-walled chamber that receives the blood retuning from the body tissues. This blood, which is low in oxygen, is carried in the veins, the blood vessels leading to the heart from the body tissue.
- The right ventricle pumps the venous blood received from the right atrium and sends it to the lungs.
- The left atrium receives blood high in oxygen content as it returns from the lungs.
- The left ventricle, which has the thickest walls of all, pumps, oxygenated blood to all parts of the body. This blood goes through the arteries, the vessels that take blood from the heart to the tissues.
Four valves within the heart
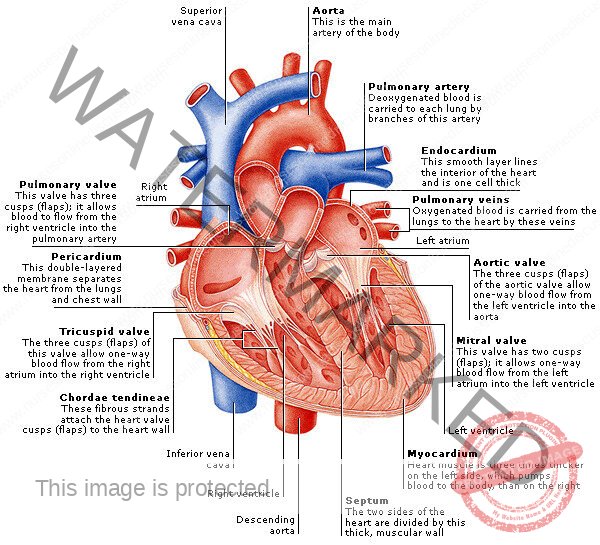
Since the ventricles are the pumping chambers, the valves, which are all one way, are located at the entrance and the exit of each ventricle. The entrances valves are the atrioventricular valves, while the exit valves are the semi lunar valves. Semilunar means “resembling a half moon.” Each valve has a specific name, as follows:
- The right atrioventricular valve also is known as the tricuspid valve, since it has three cusps, or flaps, that open and closes. When this valve is open, blood flows freely from the right atrium into the right ventricle. However, when the right ventricle begins to contract, the valve closes so that blood cannot return to the right atrium; this ensures forward flow into the pulmonary artery.
- The left atrioventricular valve is the bicuspid valve, but it is usually referred to as the mitral valve. It has two rather heavy cusps that permit blood to flow freely from the left atrium into the left ventricle. However, the cusps close when the left ventricle begins to contract; this prevents blood from returning to the left atrium and ensures the forward flow of blood into the aorta. Both the tricuspid and mitral valves are attached by means of thin fibrous threads to the wall of the ventricles. The function of these threads, called the chordae tendineae, is to keep the valve flaps from flipping up into the atria when the ventricles contract and thus causing a backflow of blood.
- The pulmonic (semilunar) valve is located between the right ventricle and the pulmonary artery that leads to the lungs. As soon as the right ventricle has finished emptying itself, the valve closes in order to prevent blood on its way to the lungs from returning to the ventricle.
- The aortic (semilunar) valve is located between the left ventricle and the aorta. Following contraction of the left ventricle, the aortic valve closes to prevent the flow of blood back from the aorta to the ventricle. (Diagram showing internal structures of the heart)
Blood Supply to the Myocardium (Coronary arteries and cardiac veins)
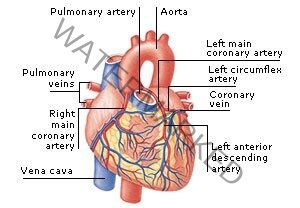
Although blood flows through the heart chambers, only the endocardium comes into contact with it. Therefore, the myocardium must have its own blood vessels to provide oxygen and nourishment and to remove waste products. The arteries that supply blood to the muscle of the heart are called the right and left coronary arteries. These arteries, which are the first branches of the aorta, arise just above the aortic semilunar valve. They receive blood when the heart relaxes. After passing through capillaries in the myocardium, blood drains into the cardiac veins and finally into the coronary (venous) sinus for return to the right atrium.
The Conduction System of the Heart (draw the diagram)
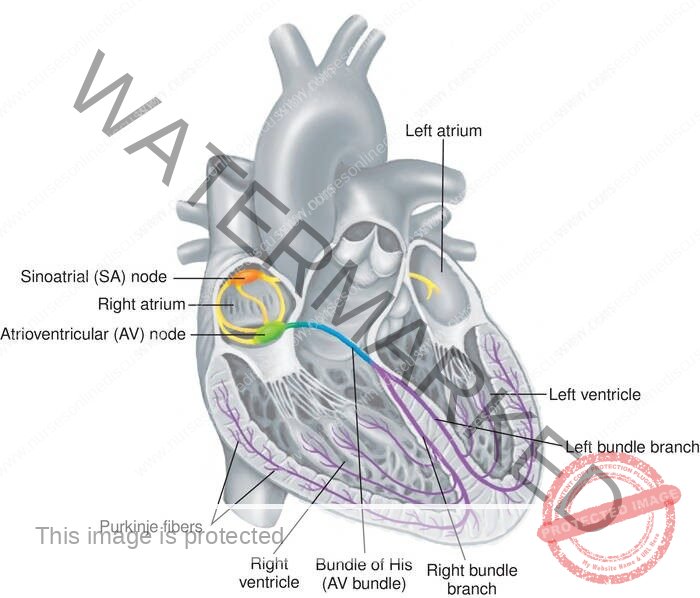
The cardiac cycle is regulated by specialized areas in the heart wall that forms the conduction system of the heart. Two of these areas are tissue mass called nodes; the third is a group of fibers called the atrioventricular bundle.
The sinoatrial node, which is located I the upper wall of the right atrium an initiates the heartbeat, is called the pacemaker. The second node, located in the interatrial septum at the bottom of the right atrium, is called the atrioventricular node. The atrioventricular bundle, also known as the bundle of His, is located at the top of the interventricular septum; it has branches that extend to all parts of the ventricle walls.
Fibers travel first down both sides of the interventricular septum in groups called the right and left bundle branches. Smaller Purkinje fibers then travel in a branching network throughout the myocardium of the ventricles.
The order in which the impulses travel is as follows:
- The sinoatrial node generates the electric impulse that begins the heart beat.
- The excitation wave travels throughout the muscle of each atrium, causing it to contract.
- The atrioventricular node is stimulated. The relatively slower conduction through this node allows time for the atria to contract and complete the filling of the ventricles.
- The excitation wave travels rapidly through the bundle of His and then throughout the ventricular walls by means of the bundle branches and Purkinje fibers. The entire musculature of the ventricle’s contracts practically at once.
Physiology of the Heart (The Work of the Heart)
- Although the right and left side of the heart are separated from each other, they work together. The blood is squeezed through the chambers by a contraction of heart muscle beginning in the thin-walled upper chambers, the atria, followed by a contraction of the thick muscle of the lower chambers, the ventricles. This active phase is called systole, and in each case, it is followed by a resting period known as diastole.
- The contraction of the walls of the atria is completed at the time the contraction of the ventricles begins. Thus, the resting phase (diastole) begins in the atria at the same time as the contraction (systole) begins in the ventricles.
- After the ventricles have emptied, both chambers are relaxed for a short period of time as they fill with blood. Then another beat begins with contraction of the ventricles. This sequence of heart relaxation and contraction is called the cardiac cycle. Each cycle takes an average of 0.8 seconds.
- Cardiac muscle tissue has several unique properties. One of these is the interconnection of the muscle fibers. The fibers are interwoven so the stimulation that causes the contraction of one fiber results in the contraction of the whole group. This plays an important role in the process of conduction and the working of the heart muscle.
- Another property of heart muscle is its ability to adjust contraction strength to the amount of blood received. When the heart chamber is filled and the wall stretched (within limits), the contraction is strong. As less blood enters the heart, the contraction becomes weaker. As more blood enters the heart, as occurs during exercise, the muscle contracts, with greater strength so push the larger volume of blood out into the blood vessels.
- The volume of blood pumped by each ventricle in 1 minute is termed the cardiac output. It is determined by the volume of blood ejected from the ventricle with each beat−the stroke volume−and the number of beats of the heart per minute−the heart rate. The cardiac output averages 5 liters/minute for an adult at rest
Control of the Heart Rate
Although the fundamental beat of the heart originates within the heart itself, the heart rate can be influenced by the nervous system and by other factors in the internal environment. Recall from chapter 7 that stimulation from the sympathetic nervous system increases the heart rate and the stimulation from the parasympathetic nervous system decreases the heart rate.
These influences allow the heart to meet changing need rapidly. The heart rate is also affected by such factors as hormones, ions, and drugs in the blood.
Heart Rates
- Bradycardia is a relatively slow heart rate of less than 60 beats/minute. During rest and sleep, the heart may beat less than 60 beats /minute but usually does not fall below 50 beats /minute.
- Tachycardia refers to a heart rate over 100 beats/minute.
- Sinus arrhythmia is a regular variation in heart rate due to changes in the rate and depth of breathing. It is normal phenomenon.
- Premature beats, also called extra systoles are beats that come in before the expected normal beats. They may occur in normal persons initiated by caffeine, nicotine, or psychological stresses. They are also common in persons with heart disease.
Heart Sounds and Murmurs
The normal heart sounds are usually described by the syllables “lubb” and “dupp.” The first is a longer, lower pitched sound that occurs at the start of ventricular systole. It is probably caused by a combination of things, including closure of the atrioventricular valves.
The second, or “dupp,” sound is shorter and sharper. It occurs at the beginning of ventricular relaxation and is due in large part to sudden closure of the semilunar valves.
Some abnormal sounds called murmurs are usually due to faulty action of the valves. For example, if the valves fail to close tightly and blood leaks back, a murmur is heard. Another condition giving rise to an abnormal sound is the narrowing (stenosis) of a valve opening.
The many conditions that can cause abnormal heart sounds include congenital defects, disease, and physiological variations. A murmur due to rapid filling of the ventricles is called a
Functional (flow) murmur; such a murmur is not abnormal.
An abnormal sound caused by any structural change in the heart or the vessels connected with the heart is called an organic murmur.
Blood pressure
Objectives: at the end of the session students should be able to:
- Define blood pressure
- Identify factors affecting blood pressure
- Identify requirements for measuring blood pressure
- Carry out blood pressure measurement
Definition
Blood pressure is the force exerted by blood on the walls of the arterial blood vessel.
Description of a sphygmanometer
This consists of a mercury manometer graduated in millitres. It has an inflatable arm band for compressing the brachial artery and a rubber bulb with a release valve for inflation and letting it down. the arm band is made up of non stretchable material containing a rubber bag from which lead two tubes, one going to the manometer and the other to the inflating bulb. The whole is contained in a long box which when opened, has mercury manometer in the lid.
Other types: aneroid-dial instead of column of mercury
Stethoscope: Consists of the ear piece, the diaphragm and the bell.
Factors affecting BP
- Force of ventricular contraction
- Arterial wall elasticity
- Peripheral vascular resistance
- Blood viscosity
- Position of the body
Definition of Pulse
Pulse is the expansion and recoil of the artery caused by the blood being pumped into it by the heart.
Normal ranges
- Adults: 60-90 beat per minute
- Children: 80- 130 b/min
- Infants: 80-140 b/min
- New born 120-160b/min
The pulse rate is the number of expansion and contraction (beats) per minute
Observation to be made
- Rate of the pulse-the number of beats counted in one minute
- The volume and force of the pulse-beat
- Rhythm of the pulse
- The tension of the resistance-indicating the strength of the arterial wall
Common sites for checking the pulse
- Temporal artery in front of the ear
- Facial artery 2.5cm in front of the angle of the jaw
- Carotid artery in the neck
- Radial artery at the thumbs side of the wrist
- Femoral artery in the groin
- Posterior tibial artery just below the internal medial malleolus
- Fontanelles in infants
Common terms relating to pulse
- Brandycardia: this is abnormally slow heart rate indicated by a slow pulse rate of less than 60b/min. this is usually accompanied by parasympathetic nervous system stimulation. For example in cerebral hemorrhage, heart block.
- Dicrotic: characterized by a double beat
- Tachycardia: this is a rapid heart action indicated by a rapid pulse rate- a rate above 100b/min. it accompanies sympathetic stimulation, emotional stress like anger, fear, anxiety, and certain medicines such as caffeine, heart conditions like congestive cardiac failure.
- Irregular: this is uneven time interval between beats for example, periods of regular rhythm interrupted by pauses, or premature beats. It may indicate cardiac irritability, hypoxia, and potassium imbalance.
Points to remember
- Avoid pressing the pulse deeply as it may disappear
- Learn to differentiate your pulse from that of the patient
Blood Vessels
Functional classification
The blood vessels, together with the four chambers of the heart, from a closed system for the flow of blood; only if there is an injury to some part of the wall of this system does any blood escape. On the basis of function, blood vessels may be classified into three groups:
- Arteries carry blood from the ventricles (pumping chambers) of the heart out to the capillaries in organs and tissue. The smallest arteries are called arterioles.
- Veins drain capillaries in the tissues and organs and return the blood to the heart. The smallest veins are the venules.
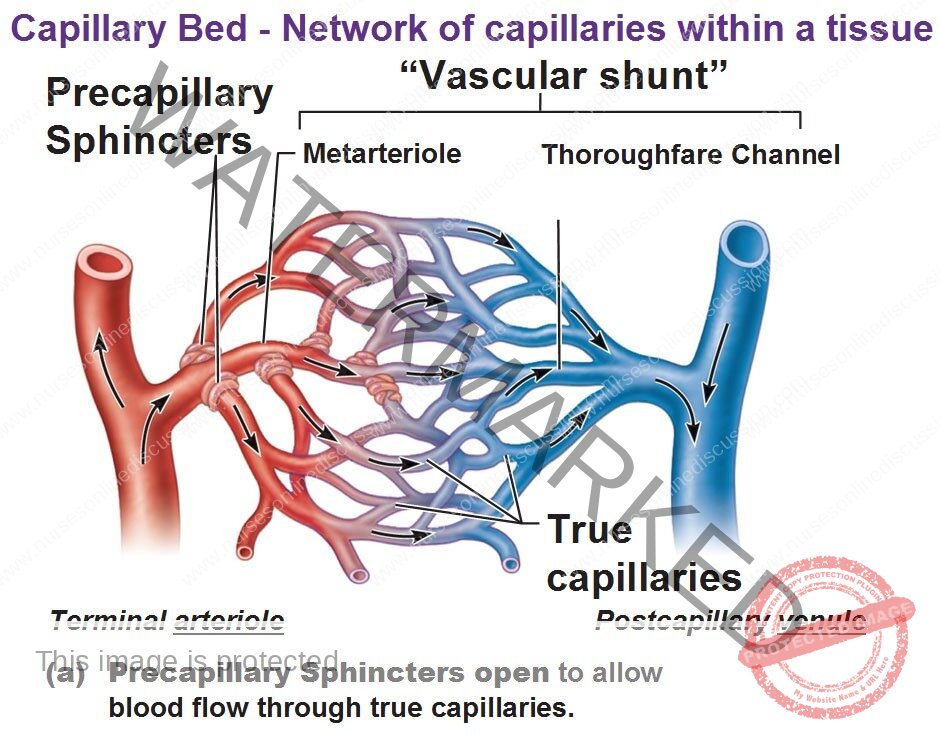
- Capillaries allow for exchanges between the blood and body cells, or between the blood and air in the lung tissues. The capillaries connect the arterioles and venules.
Structure of blood vessels
Arteries, veins and capillaries differ in structure. Three coats or layers are found in both arteries and veins . The outer most layer is called the tunica externa. Note smooth muscle is found in the middle layer or tunica media of arteries and veins. However, the muscle layer is much thicker in arteries than in veins. Why; because the thicker muscle layer in the artery wall is able to resist great pressures generated by ventricular systole. In arteries, the tunica media plays a critical role in maintaining blood pressure and controlling blood distribution in the body. This is a smooth muscle, so it is controlled by the autonomic nervous system.
A thin layer of elastic and white fibrous tissue covers an inner layer of endothelial cells called the tunica interna in arteries and veins. The tunica interna is actually a single layer of squamous epithelial cells called endothelium that lines the inner surface of the entire circulatory system. Veins have a unique structural feature not present in arteries. They are equipped with one way valves that prevent the backflow of blood. When a surgeon cuts into the body, only arteries, arterioles, veins, and venules can be seen.
Capillaries cannot be seen because they are microscopic. The most important structural feature of capillaries is their extreme thinness−only one layer of flat, endothelial cells composes the capillary membrane. Instead of three layers or coats, the capillary wall is composed of only one−the tunica interna. Substances such as glucose, oxygen, and wastes can quickly pass through it on their way to or from the cells. Smooth muscle cells that are called precapillary sphincters guard the entrance to the capillary and determine into which capillary blood will flow.
These have three distinct layers which include:
Tunica externa (adventitia, outer layer) – it is made up of fibrous connective tissue. Has collagen and elastin for support and elasticity of blood vessels.
Tunica media (thickest) – made up of smooth muscle fibers that encircle blood vessel. Involved in support and alter of diameter of blood vessels by contraction and relaxation.
Tunica internal (intima, inner layer) – forms inner lining of blood vessel. Made up of single layer of squamous epithelial cells (endothelium). Supported by a small layer of connective tissue that lies between it and smooth muscle fibers.
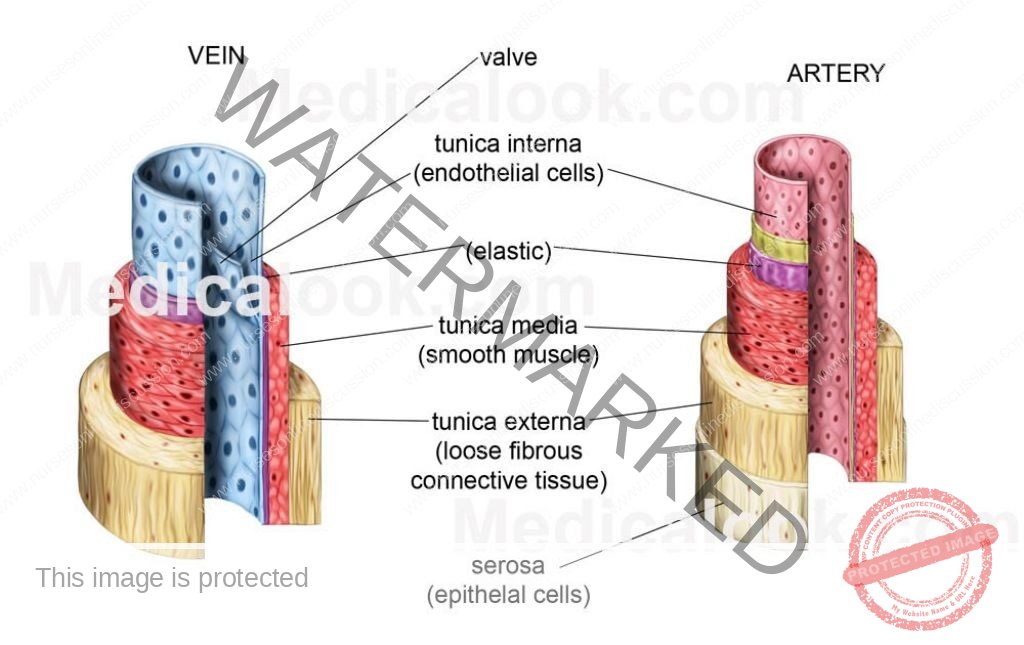
- Arteries and veins have same basic structure.
- Arterial walls contain more smooth muscle and elastic connective tissue as an adaptation to high pressure found in them.
- Veins have valves in the endothelium to prevent back flow of blood.
Arteries
Carry blood from the heart. Branch repeatedly into smaller and smaller arteries called arterioles (microscopic arteries). As more branching occurs, thickness of muscle layer decreases. Arterioles (smallest) consist of endothelium and few encircling smooth muscle fibers. Arterioles play important role in the control of blood flow and blood pressure. Major arteries of the heart include aorta and pulmonary artery.
Veins
Also called capacitance vessels because they can easily expand, have low pressure hence low resistance. Carry blood towards the heart. From the capillaries blood goes into the venules which are the smallest veins. Venules consist of endothelium and connective tissue. Large veins have smooth muscle tissue. When venules unite they form veins. Small veins connect to form large veins as blood is returned to the heart. Large veins especially those in the legs and arms contain valves to prevent back flow of blood with a aim of returning blood to the heart. 60% blood volume in the veins, store blood carried to areas in times of need. Major veins of the heart include vena cava and pulmonary vein.

Capillaries
These are the smallest blood vessels. They are also most numerous and are connected between arterioles and venules. Diameter is so small that red blood cells must pass in a single file. The walls have only endothelium (allow exchange of materials between blood and blood cells.) the distribution of capillaries varies with metabolic activity of tissue (active tissues like nerve and muscles, every cell is near a capillary).
They are less abundant in connective tissue and absent in some for example cartilage, epidermis and lens and cornea of the eye. Blood flow into the arteries is controlled by pre-capillary sphincters. (Smooth muscle fibers encircling bases of capillaries at the arteriole- capillary junctions). Blood within the capillaries depends on activity (diversion of blood from digestive system to skeletal system during exercise). Types of capillaries; classified as continuous, fenestrated or sinusoidal. Depends on diameter and permeability of the capillary
Continuous; these capillaries have a diameter of 7 micrometers. The walls exhibit no gaps between the endothelium. Less permeable to large molecules and usually found in muscles, nervous tissue and many other locations.
Fenestrated; have numerous fenestrae (windows) on endothelial cells. Fenestrae are areas approximately 70 to 100 micrometers in diameter. Cytoplasm is absent and the plasma membrane consists of a porous diaphragm that is thinner than normal thus highly permeable. Found in intestinal villi, ciliary process of eye, choroid plexuses of central nervous system, and glomeruli of kidneys.
Sinusoidal; they are larger than the rest. The fenestrae are larger. The basement membrane is less prominent. Found in endocrine glands where large molecules cross.
Sinusoids – these are larger diameter sinusoidal capillaries. The basement membrane is sparse often missing. The structure is in such a way that large molecules and cells can move readily across walls between endothelial cells. Common in liver and bone marrow
Venous sinuses are similar to sinusoidal capillaries but even larger (primarily in spleen). Large gaps within the endothelial cells make up their walls.
Walls of capillaries effectively permeable barriers because they don’t allow red blood cells and large water soluble molecules like proteins cannot readily pass through them
Location of common arteries and veins
Names of systemic arteries
The Aorta and Its Parts
The aorta is the largest artery in the body. It extends upward and to the right from the left ventricle. Then it curves backward and to the left. It continues down behind the heart just in front of the vertebral column, through the diaphragm, and into the abdomen. The aorta is one continuous artery, but it may be divided into sections:
- The ascending aorta is near the heart and inside pericardial sac.
- The aortic arch curves from the right to the left and also extends backward.
- The thoracic aorta lies just in front of the vertebral column behind the heart and in the space behind the pleura.
- The abdominal aorta is the longest section of the aorta, spanning the abdominal cavity.
The thoracic and abdominal aorta together makes up the descending aorta
Branches of the Ascending Aorta
The first, or ascending, part of the aorta has two branches near the heart, called the left and right coronary arteries that supply the heart muscle. These from a crown around the base of the heart and give off branches to all parts of the myocardium.
Branches of the Aortic Arch
The arch of aorta, located immediately beyond the ascending aorta, gives off three large branches.
- The brachiocephalic trunk is a short artery formerly called the innominate. Its name means that is supplies the head and the arm. After extending upward somewhat less than 5cm (2 inches), it divides into the right subclavian artery, which supplies the right side of the head and the neck.
- The left common carotid artery extends upward from the highest part of the aortic arch. It supplies the left side of the neck and the head.
- The left subclavian artery extends under the left collar bone (clavicle) and supplies the left upper extremity. This is the last branch of the aortic arch.
Branches of the Thoracic Aorta
The third part of the aorta supplies branches to the chest wall, to the esophagus, and to the bronchi and their treelike subdivisions in the lungs.
There are usually nine to ten pairs of intercostals arteries that extend between the ribs, sending branches to the muscles and other structures of the chest wall.
Branches of the Abdominal Aorta
As in the case of the thoracic aorta, there are unpaired branches extending forward and paired arteries extending toward the side.
The unpaired vessels are large arteries that supply the abdominal viscera. The most important of these visceral branches are listed below:
- The celiac trunk is a short artery about 1.25 cm long that subdivides into three branches: the left gastric artery goes to the stomach, the splenic artery goes to the spleen, and the hepatic artery carries oxygenated blood to the liver.
- The superior mesenteric artery, the largest of these branches, carries blood to most of the small intestine as well as to the first half of the large intestine.
- The much smaller inferior mesenteric artery, located below the superior mesenteric and near the end of the abdominal aorta, supplies the second one half of the large intestine.
- The lateral (paired) branches of the abdominal aorta include the following right and left divisions:
- The phrenic arteries supply the diaphragm.
- The suprarenal arteries supply the adrenal (suprarenal) glands.
- The renal arteries, the largest in this group, carry blood to the kidneys.
- The ovarian arteries in the female and testicular arteries in the male (formerly called the spermatic arteries), supply the sex glands.
- Four pairs of lumbar arteries extend into the musculature of the abdominal wall.
- The abdominal aorta finally divides into two common iliac arteries. Both of these vessels, about 5 cm long, extend into the pelvis, where each one subdivides into an internal and an external iliac artery.
The internal iliac vessels then send branches to the pelvic organs, including the urinary bladder, the rectum, and some of the reproductive organs.
The external iliac arteries continue into the thigh as the femoral arteries. These vessels give off branches in the thigh and then become the popliteal arteries, which subdivide below the knee. The subdivisions include the tibial arteries and dorsalis pedis, which supply the leg and the foot.
Other Subdivisions of Systemic Arteries
Just as the larger branches of a tree give off limbs of varying sizes, so the arterial tree has a multitude of subdivisions.
Hundreds of names might be included, but we shall mention only a few. For example, each common carotid artery gives off branches to the thyroid gland and other structures in the neck before dividing into the external and internal carotid artery, which supplies parts of the head.
The hand receives blood from the subclavian artery, which becomes the axillary in the axilla
(armpit).
The longest part of this vessel, the brachial artery, is in the arm proper. It subdivides into two branches near the elbow: the radial artery, which continues down the thumb side of the
forearm and wrist, and the ulnar artery, which extends along the medial or little finger side into the hand.
Anastomosis
A communication between two arteries is called an anastomosis. By this means, blood reaches vital organs by more than one route. Some examples of such unions of end arteries are described below:
- 1. The circle of Willis receives blood from the two internal carotid arteries as well as from the basilar artery, which is formed by the union of two vertebral arteries. This arterial circle lies just under the center of the brain and sends branches to the cerebrum and other parts of the brain.
- The volar arch is formed by the union of the radial and ulnar arteries in the hand. It sends branches to the hand and fingers.
- The mesenteric arches are made of communications between branches of the vessels that supply blood to the intestinal.
- Arterial arches are formed by the union of branches of the tibial arteries in the foot, and similar anastomoses are found in various parts of the body.
Arteiovenous anastomoses are found in a few parts of the body, including the external ears, the hands, and the feet. Vessels that have muscular walls connect arteries directly with veins and thus bypass the capillaries. This provides a more rapid flow and a greater volume of blood to these areas the elsewhere, thus protecting these exposed parts from freezing in cold weather
Names of Systemic Veins
Superficial Veins
Whereas most arteries are located in protected and rather deep areas of the body, many veins are found near the surface. The most important of these superficial veins are in the extremities.
These include the following:
- The veins on the back of the hand and at the front of the elbow. Those at the elbow are often used for removing blood samples for test purposes, as well as for intravenous injections. The largest of this group of veins are the cephalic, the basilic, and the median cubital veins.
- The saphenous veins of the lower extremities, which are the longest veins of the body. The great saphenous vein begins in the foot and extends up the medial side of the leg, the knee, and the thigh. It finally empties into the femoral vein near the groin.
Deep Veins
The deep veins tend to parallel arteries and usually have the same names as the corresponding arteries. Examples of these include the femoral and the iliac vessels of the lower part of the body and the brachial, axillary, and subclavian vessels of the upper extremities. However, exceptions are found in the veins of the head and the neck. The jugular veins drain the areas supplied by the carotid arteries.
Two brachiocephalic (innominate) veins are formed, one on each side, by the union of the subclavian and the jugular veins. (Remember there is only one brachiocephalic artery).
Superior Vena Cava
The veins of the head, neck, upper extremities, and chest all drain into the superior vena cava, which goes to the heart. It is formed by the union of the right and left brachiocephalic veins, which drain the head, neck, and upper extremities. The azygos vein drains the veins of the chest wall and empties into the superior vena cava just before the latter empties into the heart
Inferior Vena Cava
The inferior vena cava, which is much longer than the superior vena cava, returns the blood from the parts of the body below the diaphragm. It begins in the lower abdomen with the union of the two common iliac veins. It then ascends along the back wall of the abdomen, through a groove in the posterior part of the liver, through the diaphragm, and finally through the lower thorax to empty into the right atrium of the heart.
Principal veins
Drainage into the inferior vena cava is more complicated than drainage into the superior vena cava. The large veins below the diaphragm may be divided into two groups:
- The right and left veins that drain paired parts and organs.
They include the iliac veins from near the groin, four pairs of lumbar veins from the dorsal part of the trunk and from the spinal cord, the testicular veins from the testes of the male and the ovarian veins from the ovaries of the female, the renal and suprarenal veins from the kidneys and adrenal glands near the kidneys, and finally the large hepatic veins from the liver. For the most part, these vessels empty directly into the inferior vena cava. The left testicular in the male and the left ovarian in the female empty into the left renal vein, which then take this blood to the inferior venal cava; these veins thus constitute exceptions to the rule that the paired veins empty directly into vena cava.
- Unpaired veins that come from the spleen and from parts of the digestive tract (stomach and intestine) and empty into a vein called the portal vein. Unlike other veins, which empty into the inferior vena cava, the hepatic portal vein is part of a special system that enables blood to circulate through the liver before returning to the heart.
Circulatory Routes or Circuits
All the vessels together may be subdivided into two groups or circuits: pulmonary and systemic.
- Pulmonary circulation: carry blood to and from the lungs.
They in include the pulmonary artery and its branches to the capillaries in the lungs, as well as the veins that drain those capillaries. The pulmonary arteries carry blood low in oxygen from the right ventricle, while the pulmonary veins carry blood high in oxygen from the lungs into the left atrium. This circuit functions to eliminate carbon dioxide from the blood and replenish its supply of oxygen.
- Systemic circulation: it is the largest circulatory route. It takes oxygenated blood from the left ventricle through the aorta to all parts of the body, including some lung tissue (not air sac or alveolus) and returns the deoxygenated blood to the right atrium, through the systemic veins; the superior vena cava, the inferior vena cava, and the coronary sinus. It has several subdivisions. Two of the several subdivisions are the coronary circulation and the hepatic portal system or circulation.
Hepatic Portal System
Almost always, when blood leaves a capillary bed it returns directly to the heart. In a portal system, however, blood circulates through a second capillary bed, usually in a second organ, before returning to the heart. Thus, a portal system is a kind of detour in the pathway of venous return that can transport materials directly from one organ to another. The portal system between the hypothalamus and the anterior pituitary has already been described. The largest portal system in the body is the hepatic portal system, which carries blood from the abdominal organs to the liver.
The hepatic portal system includes the veins drains blood from capillaries in the spleen, stomach, pancreas, and intestine. Instead of emptying their blood directly into the inferior
Hepatic portal circulation vena cava, they deliver it by way of the hepatic portal vein to the
liver. The largest tributary of the portal vein is the superior mesenteric vein it is joined by the spleenic vein just under the liver. Other tributaries of the portal circulation are the gastric,
pancreatic, and inferior mesenteric veins.
Upon entering the liver, the portal vein divides and subdivides into ever smaller branches. Eventually, the portal blood flows
Into a vast network of sinus-like vessels called sinusoids. These are enlarged capillaries that serve as blood channels within the tissues of the liver, spleen, thyroid gland, and other structures.
After leaving the sinusoids, blood is finally collected by the hepatic veins, which empty into the inferior vena cava
The purpose of the portal system of veins is to the liver sinusoids so the liver cells can carry out their functions. For example, when food is digested, most of the end products are absorbed from the small intestine into the blood stream and transported to the liver by the portal system. In the liver, these nutrients are processed, stored, and released as needed into the general circulation.
Pulse and Blood Pressure
Pulse
The ventricles pump blood into the arteries regularly about 70 to 80 times a minute. The force of the ventricular contraction starts a wave of increased pressure that begins at the heart and travels along the arteries.
This wave, called the pulse, can be felt in any artery that is relatively close to the surface, particularly if the vessel can be pressed down against a bone. At the wrist the radial artery passes over the bone on the thumb side of the forearm, and the pulse is most commonly obtained here. Other vessels sometimes used for obtaining the pulse are the carotid artery in the neck and the dorsalis pedis on the top of the foot.
Normally, the pulse rate is the same as the heart rate. Only if a heartbeat is abnormally weak, or if the artery is obstructed, may the beat not be detected as a pule. In checking the pulse of another person, it is important to use your second or third finger.
If you use your thumb, you may find that you are getting your own pulse. When taking a pulse, it is important to gauge the strength as well as the regularity and the rate.
Various factors may influence the pulse rate, we will enumerate just a few:
- The pulse is somewhat faster in small persons than in large persons usually slightly faster in women than in men.
- In a new born infant the rate may be from 120 to 140 beats/minute. As the child grows, the rate tends to become slower.
- Muscular activity influences the pulse rate. During sleep the pulse may slow down to 60 a minute, while during strenuous exercise the rate may go up to well over 100 a minute. In a person in good condition, the pulse does not remain rapid despite continued exercise.
- Emotional disturbances may increase the pulse rate.
- In many infections, the pulse rate increases with the increase in temperature.
- An excessive amount of secretion from the thyroid gland may cause a rapid pulse. The pulse rate may serve as a partial guide for persons who must take thyroid extract.
Blood Pressure
Since the pressure inside the blood vessels varies with the condition of the heart, the blood, and the vessels, as well as with other factors, the measurement and careful interpretation of blood pressure may prove a valuable guide in the care and evaluation of a person’s health. Because blood pressure decreases as the blood flows from arteries into capillaries and finally into veins, measurements ordinarily are made of arterial pressure only. The instrument used is called a sphygmomanometer, and two variables are measured.
- Systolic pressure, which occurs during heart muscle contraction, averages around 120 and is expressed in millimeters of mercury (mm Hg).
- Diastolic pressure, which occurs during relaxation of the heart muscle, averages around 80 mm Hg.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowWe are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

