Anatomy & Physiology
Subtopic:
The Skeletal System
Learning Objectives
Understand the structure and function of the skeletal system.
Identify and classify types of bones and their anatomical features.
Describe the development, growth, and healing processes of bone tissue.
Explain the role of bone cells (osteoblasts, osteoclasts, osteocytes, osteogenic cells).
Compare compact vs. spongy bone structure and function.
Recognize the bones of the axial and appendicular skeleton.
Distinguish between male and female skeletal differences.
Describe the structure and function of joints, including types and movements.
Understand the influence of hormones, diet, and exercise on bone health.
Identify bones of the skull, vertebral column, thoracic cage, and limbs.
Introduction to Skeletal system
- The human skeleton begins as cartilage and fibrous membranes. By age 25, the skeleton is completely hardened. The adult skeleton consists of 206 bones, which are 20% of body mass:
- 80 bones in the axial skeleton.
- 126 bones in the appendicular skeleton.
- The skeletal system includes bones and structures connecting them to other tissues, such as ligaments, tendons, and cartilages.
- A skeleton (the word skeleton came from a Greek word skeleton meaning “dried up”
- It’s strong yet light adopted for its function of body protection and motion.
- The skeletal system includes bones, cartilages, joints and ligaments. The joints give the body flexibility and allow movements to occur but from structural point of view the human skeleton consists of two main types of supportive connective tissue hat is bone and Cartilage.
- The human skeleton begins as cartilage and fibrous membranes. By age 25, the skeleton is completely hardened. The adult skeleton consists of 206 bones, which are 20% of body mass:
Functions of the skeletal system
- Shape/frame work, Protection, Support, Flexibility
- Movement
- Storage
- Blood cell formation
- Forming boundaries
- Support: It forms the internal frame work that supports and anchors soft organs.
- Protection: Bones protect soft body organs.
- Movement: Skeletal muscles attached to the skeletal system use the bones to move the body and its parts.
- Storage: Fats, blood cells are stored in the internal cavities of bones. It is also a store house of minerals e.g calcium and phosphate.
- Blood cell formation: It occurs within the bone marrow cavities of long bones.
Bone
- A bone/osseous is a specialized connective tissue that has the strength of cat iron and the lightness of pine wood.
- Living bone is not dry, brittle or dead. It is a moist, changing, productive tissue that is continually resorbed, reformed and remolded.
Types of Bones
- Long bone: femur, tibia, fibula
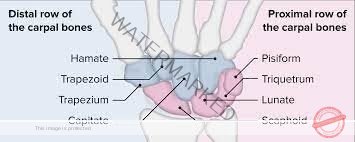
- Short bone: carpals. (Wrist)
- Flat bone: ribs, sternum
- Sesamoid bone: patella (Knee cap, pisform carpel bone
- Irregular bones: vertebrae, some skull bones.
BONE STRUCTURE
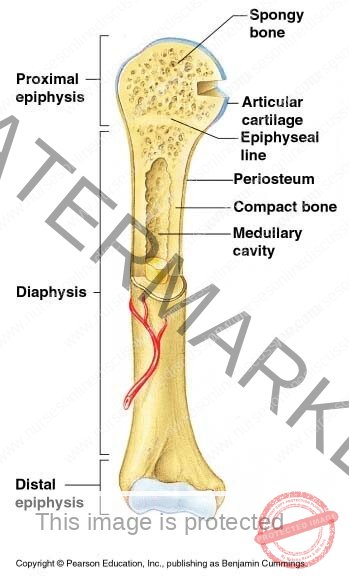
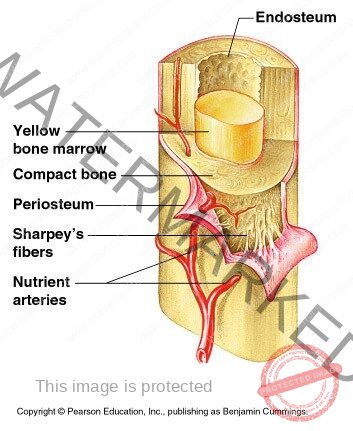
- It has the Diaphysis and two epiphysis or extremities. The Diaphysis is composed of compact bone and a hollow cyclindrical walls containing (filled-with) yellow bone marrow. The epiphysis consists of an outer covering of compact bone with spongy or cancellous bone inside.
- The two parts are separated by epiphyseal /cartilage which ossify when growth is complete
- Long bones are almost completely covered by a vascular membrane the periosteum which has two layers. The outer layer is tough and fibrous, and protects the bone underneath.
- The inner layer contains osteoblasts (bone cells) and osteoclasts responsible for bone production and break down, and is important in repair and remolding of the bone.
- The periosteum covers the whole bone except the parts that form the joints where it is replaced by articular/bone cartilages.
BONE TISSUE
- It is composed of cells embedded in the matrix of ground substance or fibres.
- It is more rigid than other tissues because it contains organic salts mainly calcium phosphate and calcium carbonate. Cap04 & caco3. A net work of collagenous fibres in the matrix gives bone tissue ,its strength and flexibility.
- Most bones have an outer sheath of compact bone tissue enclosing an interior spongy bone tissue.
COMPACT BONE TISSUE
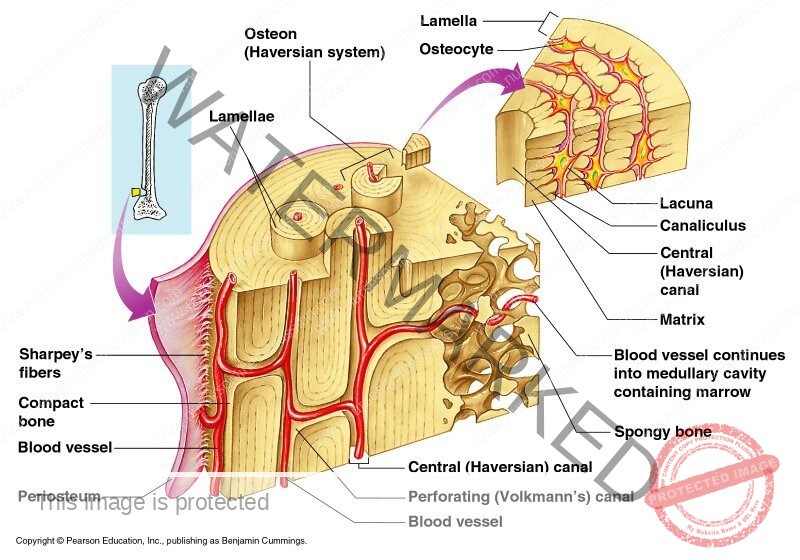
- It is found in the outer sheath of the bone. It is very hard and dense. It appears to a naked eye to be solid but is not. It contains cylinders of calcified cells called Osteon (Harversian system).
- Osteons are made of concentric layers called lamellae which are arranged seemingly in a wider and wider seeming straws.
- In the center of the osteons are central canal (Haversian canal) which is longitudinal canals that contain blood vessels, nerves, and lymphatic vessels.
- Central canals usually have canals called perforating canals that run at right and to the central canal extending the system \of nerves and vessels out ward to periosteum.
LACUNAE. (Little spaces)
- These house bone cells ( osteocytes) and are contained in the lamellae radiating from each lacuna are tiny canaliculi connecting (osteocytes) where nutrients and wastes can pass to and from the central canal.
SPONGY (CANCELLOUS) BONE
- It looks like a honey comb using the naked eye. Microcopic examination reveals a frame work formed from trabeculae, meaning little beams. Trabeculae are tiny spikes of bone tissue sorounded by bone matrix that are calicified.
- The spaces between the trubeculae contain Redbone marrow in addition spongy bone is lighter than compact bone reducing the weight of the skeleton.
DEVELOPMENT OF A BONE TISSUE
- This is called ossification or osteogenesis. This begins before birth and is not complete until about the 21 year of life.
- Long, short and irregular bones develop in the feotus from rods of cartilage (cartilage model).
- Flat bones develop from membrane model. Ribs, stemum sesamoid bones from tendon model eg Patella.
- During the process of bone development, osteoblasts secrete osteoid which gradually replaces the initial model. This osteoid is progressively calcified, as the bone grows the osteoblasts mature and become osteocytes.
Diagram
In mature bone, definite balance of osteoblast and osteoclast activity maintains normal bone structure. If osteoclast activity exceeds osteoblast activity, the bone becomes weaker. On the other hand, if osteoblast activity outstrips osteoclast activity, the bone becomes stronger and heavier.
DEVELOPMENT OF LONG BONES
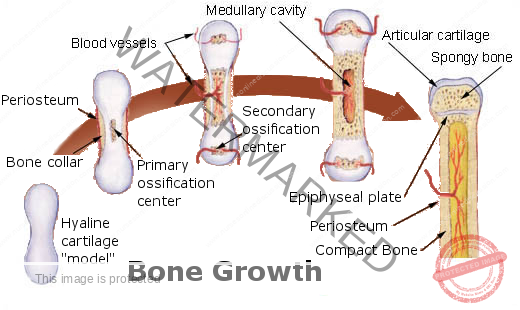
- In long bones the focal points from which ossification begins are small areas of osteogenic cells or centers of ossification in the cartilage model. This is accompanied by development of a bone collar at about 8 weeks of gestation.
- Later the blood supply develops and bone tissue replaces cartilage as osteoblasts secrete osteoid in the shaft. The bone lengthens as ossification continues and spreads to the epiphyses. Around birth, \secondly centers of ossification develop in the epiphyses, and the medullary canal forms when osteoclasts break down the central bone tissue in the middle of the shaft. During childhood, long bones continue to lengthen because the epiphyseal plate at each end of the bone, which is made of cartilage, continues to produce new cartilage on is diaphyseal surface (the surface facing the shaft of the bone).
- This cartilage is then turned to bone. As long as cartilage production matches the rate of ossification, the bone continues to lengthen, at puberty, under the influence of sex hormones, the epiphyseal plate growth slows down and is overtaken by bone deposition. Once the whole epiphyseal plate is turned to bone, no further lengthening of the bone is possible.
Hormonal regulation of bone growth
Hormones that regulate the growth, size and shape of bones include the following.
growth hormone and the thyroid hormones, thyroxine and tri- iodothyronine, are especially important during infancy and child hood; deficient or excessive secretion of these results in abnormal development of the skeleton.
Testosterone & estrogens influence the physical changes that occur at puberty and help maintain bone structure throughout life. Rising levels of these hormones are responsible of the epithyseal plates. So that bone growth length ways stops (although bones can grow in thickness throughout life. Average adult male height is usually greater than female, because male puberty tends to occur at a later age than female puberty, giving a male child bone longer to keep growing. Oestrogens are responsible for the wider female pelvis that develops during puberty, and maintaining bone mass in adult female. Falling estrogen levels after menopause can put postmenopausal women at higher risk of bone fracture (osteoporosis).
Calcitonin & parathyroid hormone
Control blood levels of calcium by regulating its uptake into and release from bone. Calcitonin increases calcium uptake into bone (reducing blood calcium), and parathemone decreases it (increasing blood calcium). Although the length and shape of bones does not normally change after ossification is complete, bone tissue is continually being remoulded and replaced when damaged. Osteoblasts continue to lay down osteoid and osteoclasts reabsorb it. The rate in different bone varies eg the distal part of the femur is replaced over a period of 5 to 6 months.
Exercise and bone
Although bone growth lengthways permanently ceases once the epiphyseal plate have ossified, thickening of bone is possible throughout life. This involves the laying down of new osteons at the periphery of the bones through the action of osteoblasts in the inne r layer of the periosteum. Weight bearing exercise stimulates thickening of bone, strenghthening it and making it less liable to fracture. Lack of exercise reverses the changes, leading to lighter, weaker bones.
Diet & bone
Healthy bone tissue requires adequate dietary calcium and vitamins A, C, and D calcium and smaller amounts of other minerals such as phosphate, iron, and manganesium, is essential for adequate mineralization of bone. Vitamin A is needed for osteoblast activity. Vitamin C is used in collagen synthesis and vitamin D is required for calcium and phosphate absorption from the intestinal tract.
BONE MARKINGS
Most bones have rough surfaces, raised protuberances and ridges that give attachment to muscle tendons and ligaments. These are not included in the following descriptions of individual bones unless they are of particular note, but many are marked on illustrations. Bone makings and related terminology are defined in table.
Anatomical terminology related to bones.
- Terms meaning
- Articulating surface: The part of the bone that enters into the formation of a joint
- Articulation: A joint between two or more bones.
- Bony sinus: A hollow cavity within bone.
- Border: A ridge of bone separating two surfaces.
- Condyle: A smooth rounded projection of bone that forms part
- of a joint.
- Facet: A small, generally rather flat, articulating surface.
- cleft: A narrow slit
- Foramen (Plural: Foramina); A hole in a structure.
- Fossa (Plural: Fossae); A hollow or depression.
- Meatus: A tube – shaped cavity within a bone.
- Septum: A partition separating two cavities.
- Spinous process or crest: a sharp ridge of bone. Styloid processes, a sharp downward projection of bone that gives attachment to muscles and ligaments.
- Suture; An immovable joint eg; between the bones of the skull.
- Trochanter, tuberosity; Roughened bony projections, usually for attachment of muscles or ligaments. The different names are used according to the size to the size of the projection. Trochanters are the largest and tubercles the smallest.
BONE CELLS
The bone contains 5 types of cells
Osteogenic cells: These are small spindle shaped cells. They are found mostly in the deepest layer of periosteum. They have a high mitotic potential and can be transformed into bone forming cells. (Osteoblasts).
Osteoblasts (Bone farming cells): These are bone forming cells. They secrete both organic and inorganic components of the bone. (Calcium phosphate)
They are found in places;
- In the deeper layers of periosteum
- In the centre of ossification of immature bone.
- At the ends of the diaphysis adjacent to the epiphyseal cartilage of the long bone.
- At the site of a fracture
Osteocytes: Are the main cells of fully developed cells mature bone cells? They have a cell that occupies the lacuna Osteocytes are derived from osteoblasts. They monitor and maintain bone tissue. They are nourished by tissue fluid in the canaliculi that radiate from the central canal.
Osteoclasts: These are multi nuclear giant cells which are found where bone is resorbed during its normal growth (resorption of bone tissue). Osteoclasts are derived from white blood cells called monocytes. They are mainly found under the periosteum to maintain the shape of bones during growth and to remove excess callus formed during healing of fractures.
HEALING OF BONE
There are a number of terms used to classify bone fractures including: –
- SIMPLE: The bone ends do not protrude through the skin
- COMPOUND: The bone ends protrude through the skin.
- PATHOLOGICAL: Fracture of a bone weakened by disease.
Following a fracture, the broken ends of bone are joined by the deposition of new bone. This occurs in several stages.
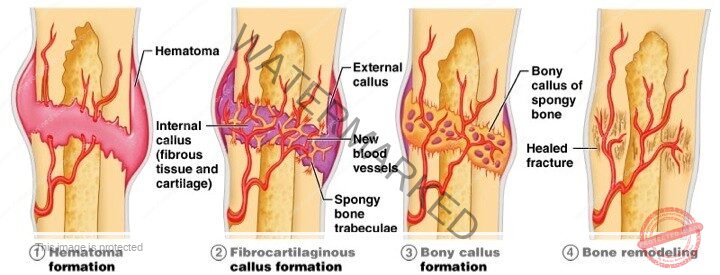
- A haematoma – (collection of clotted blood) forms between the ends of bone and in surrounding oft tissues.
- There follows development of acute inflammations and accumulation of inflammatory exodate, containing macrophages that phagocytose the haematoma and small dead fragments of bone (this takes about 5 days) Fibroblasts migrate to the site, granulation tissue and new capillaries develop.
- New bone forms as large numbers of osteoblasts secrete spongy bone which unites the broken ends and is protected by an outer layer of bone and cartilage, the new deposits of bone and cartilage is- called a callus. Over the next few weeks, the callus matures, and the cartilage is gradually replaced with new bone.
- Reshaping of the bone continues and gradually the medullary canal is reopened through the callus (in weeks or months). In time the bone heals completely with the callus tissue completely replaced with mature compact bone. Often the bone is thicker and stronger the repair site than originally, and a second fracture is more likely to occur at a different
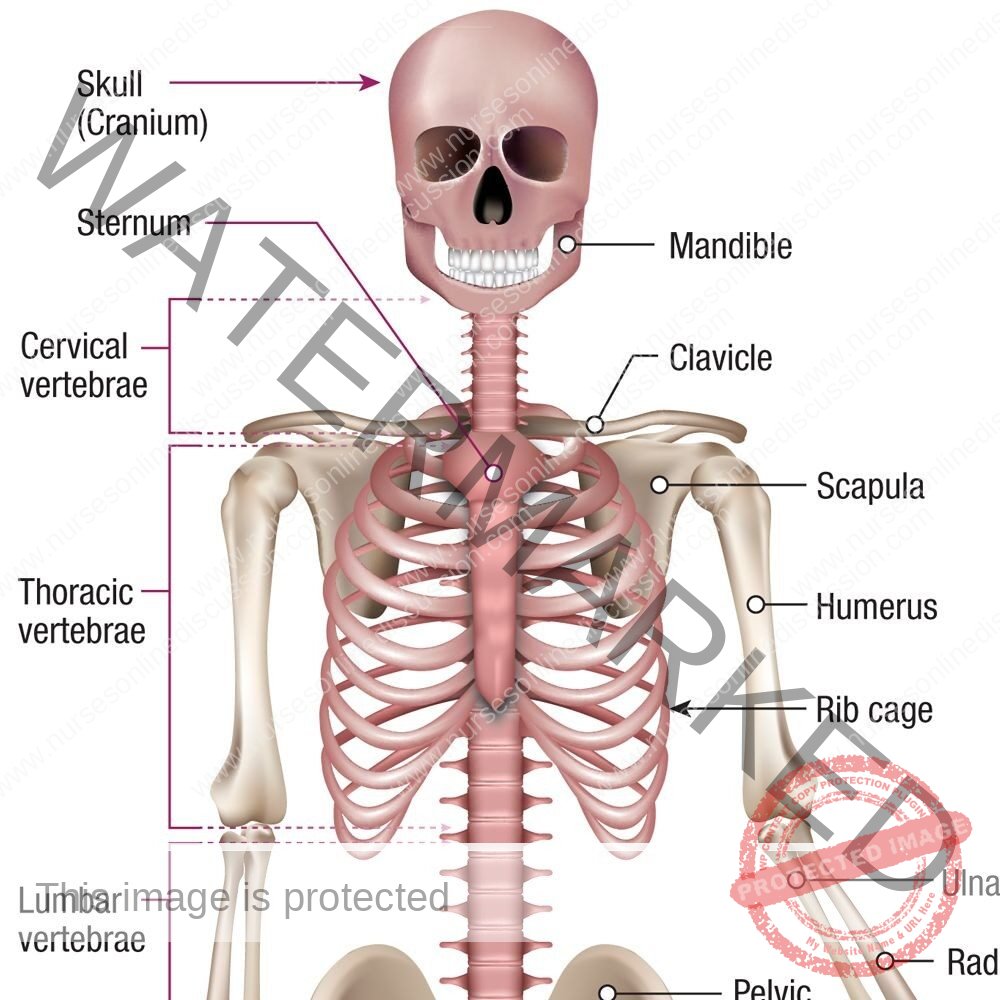
- The adult human skeleton has 206 names bones that are grouped into two principal parts.
- The axial and appendicular skeleton:
- The axial skeleton consists of bones that lie around the axis they include skull, vertebral column, ribs, sternum. Together the bones forming these structures constitute the centre core of the body (the axis).
- The appendicular skeleton consists of bone of the body out of the axial group. These are the appendages/attachments. It consists of: the shoulder girdle with upper limbs, the pelvic girdle with lower limbs.
SKULL
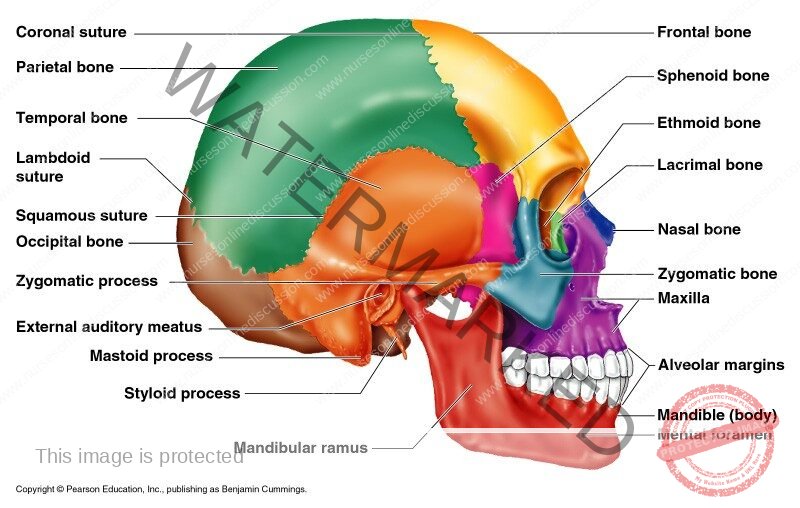
It has 29 bones. It is dividing into two parts. The Skull rests on the upper end of the vertebral column and its bony structure is divided into two parts the cranium and the face.
The bones of the skull and their suture:
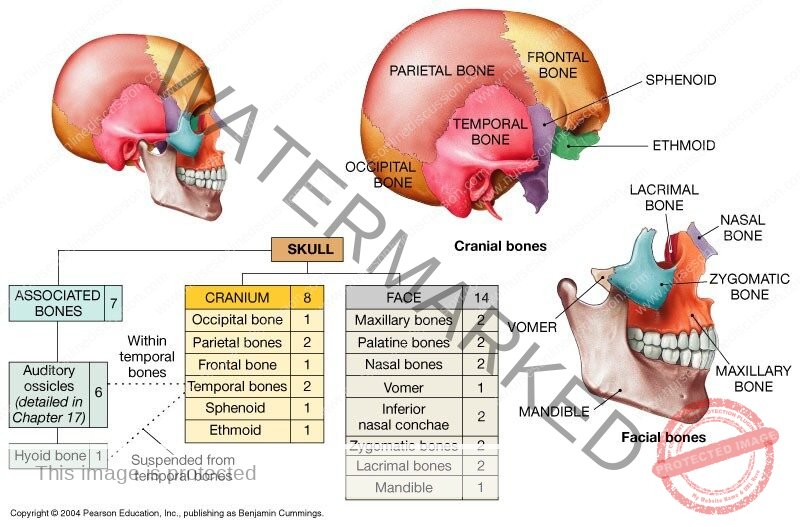
CRANIUM
- The cranium is formed by a number of that and irregular bones that provide a bony protection to the brain.
- It has a base upon which the brain rest and covers the brain.
- The periosteum lining the inner surface of the skull bones forms the outer layer of the diameter.
- In a mature skull the joints (sutures) between the bones are immovable (fibrous).
- The bones of the cranium are eight in number and include: 2 parietal bones, 2 temporal bones , 1 Ethimoid bone, 1 Sphenoid bone, 1 Ocupital bone, 1 frontal bone
FRONTAL BONE
- This is the bone of the forehead. It forms part of the orbital cavities/eye sockets) and prominent rides above the eyes called the (supraorbital margins).
- Just above the supraorbital margins within the bone cavities (sinuses) lined with epithelial mucus membrane and this opens into the nosal cavity.
- The coronal suture joins the frontal bone to the two parietal bones.
PARIETAL BONES
These bones from the sides and roof of the skull: They articulate with each other at the sagittal suture with the frontal bone at the coronal suture with the occipital bone at the lambdoidal suture and on the temporal bone at the squamous suture.
The inner surface is concave and is grounded, to accommodate the brain and blood vessels.
TEMPORAL BONES
- These lie on each side of the head. They articulate with the parietal, occipital and sphenoid and zygomatic bone.
- The squamous part; It is a thin f shaped area that articulate with the parietal bones.
- The zygomatic process; It articulates with zygomatic bone to form the zygomatic arch (cheek bone)
- The temporal bone articulates with the mandate at the temporomandibular joint: The only movable joint of the skull.
OCCIPITAL BONE
This bone forms the back of the heard and part of the base of the skull. It has immovable joints between the parietal, temporal and sphenoid bones, its inner is deeply concave and this concavity is occupied by the parts of the brain called cerebrum. The occipital bone has two articular condyles that form condyloid joint with the first bone of the vertebral column called atlas. This joints permits nodding movement of the head. Between the condyles is the faramen magnum (large hole) through which the spinal cord passes into the cranial cavity.
SPHENOID BONE
This bone the middle portion of the base of the skull and it articulates with the occipital, temporal parietal and frontal bones. On the superior surface in the middle of the bone is a little saddle shaped depression, the hypophyseal fossa where the pituitary gland is found. This bone contains fairly large air sinuses lined with ciliated mucus membrane which open into the nosal cavity.
ETHMOID BONE
It occupies the anterior part of the base of the skull and helps to form the orbital cavity, the nasal septum and the lateral walls of the nasal cavity. It is a very delicate bone containing many air sinuses. The horizontal flattened part (the cribriform plate) forms the roof of the nasal cavity and has numerous small foramina through which nerve fibres of the olfactory nerve (sense of smell) pass upwards from the nosal cavity to the brain.
FACE
face :13 bones from the face; 2 Zygomatic (check bones), 1 maxilla, 2 nosal bones, 2 lacrimal bones, 1 vomer, 2 palatine bones, 2 inferior conchae , 1 mandible
ZYGOMATIC (check bones)
- They originate as two bones that fuse before birth. They form the prominences of the checks, part of the floor and lateral walls of the orbital cavities.
MAXILLA (upper jaw bone)
- They originate as two bones but fusion takes place before birth. It forms the upper jaw, the anterior part of the roof of the mouth, the lateral walls of the nosal cavity and part of the floor of orbital cavities.
- The alveolar ridge or process carries the upper teeth and on each sides it contains air sinuses ( the maxillary sinus).
NASAL BONES
There are two small flat bones that form the greater part of the lateral and superior surface of the ridge of the nose.
LACRIMAL BONES: There two small bones posterior and lateral to the nosal bones and form part of the medial walls of the orbital cavities. Each is pierced by a foramen for the passage of the nasal lacrimal dust that carries the tears from the eyes to the nosal cavity.
VOMER: The vomer bone is a thin flat bone that extends upwards from the middle of the hard palate to form most of the inferior part of the nasal septum.
PALATINE BONES: They are two L-shape bones. The horizontal part unite to form the posterior part of the hard palate and the perpendicular parts project upwards to form part of the lateral walls of the nasal cavity.
INFERIOR CONCHAE: Each concha is a scroll – shaped bone, which forms part of the lateral wall of the nasal cavity. The superior and middle conchaa are parts of the ethmoid bone. The conchae collectively increase the surface area in the nasal cavity allowing inspired air to be warmed and humidified more effectively.
MANDIBLE (lower jaw bone): It is the only movable bone of the skull they originate as two but unite at the middline before birth. Each half consists of two main parts;
- A curved body with alveolar ridge containing the lower teeth.
- This projects upwards at right angles to the posterior ends of the body.
The condylar process which articulates with the temporal bone to form the temporomandibular joint.
The coronoid process which gives attachment to moscles and ligaments that closes the jaw. The point where the ramus joins the body is the angle of the jaw.
Diagram
HYOD BONE : It is an isolated horse shoe- shaped bone lying in the soft tissues of the neck just above the larynx and below the mandible.
It does not articulate with any other bone, but is attached to the styloid process of the temporal bone by ligaments. It supports the larynx and gives attachment to the base of the tongue.
SINUSES
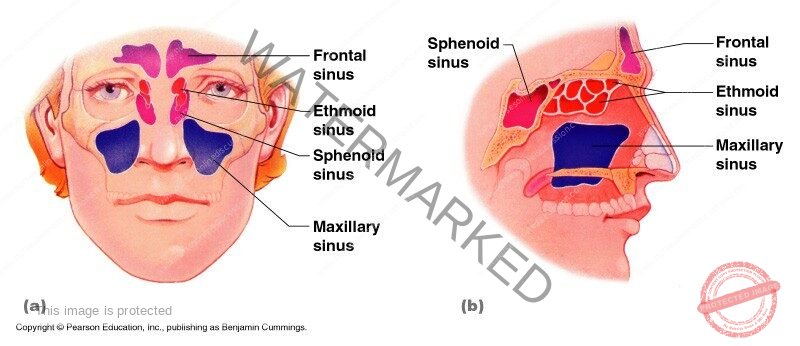
- They air filled cavities found in the sphenoid, ethmoid, maxilla and frontal bone.
- They all communicate with the nasal cavity and are aligned with ciliated mucus membrane.
- They give resonance to the voice and reduce weight of the skull.
FONTANELLES FO THE SKULL
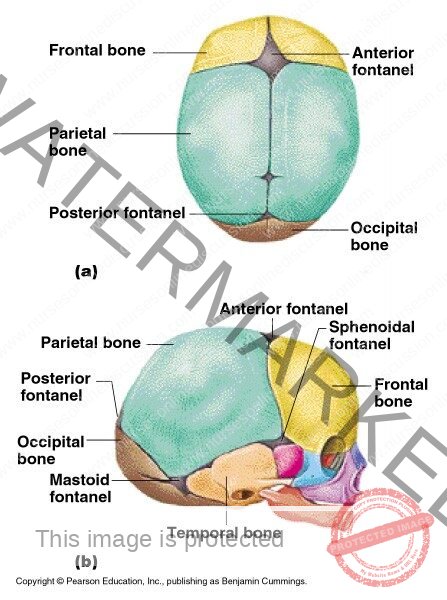
These are membraneous areas where two or three sutures meet. The two largest are the : Anterior fontanelle and Posterior fontanelle. The anterior fontanelle is not fully ossified until the child is 12-18 months old and the fontanelle usually is ossified two to three months after birth. The skull does not fuse earlier to allow for moulding of the babies head during child birth.
Functions of the skull
- The cranium protects the delicate tissues of the brain.
- The bone eye sockets provide the eye with protection against injury and give attachment to the muscles that move the
- The temporal bone protects the delicate structures of the ear.
- The sinuses in some face and skull give resonance to the body and keep the skull weight in a minimum.
- The maxilla and the mandible provide alveolar ridges in which the teeth are embedded.
- Chewing of food is performed by the mandible controlled by muscles of the lower
THE VERTEBRAL COLUMN
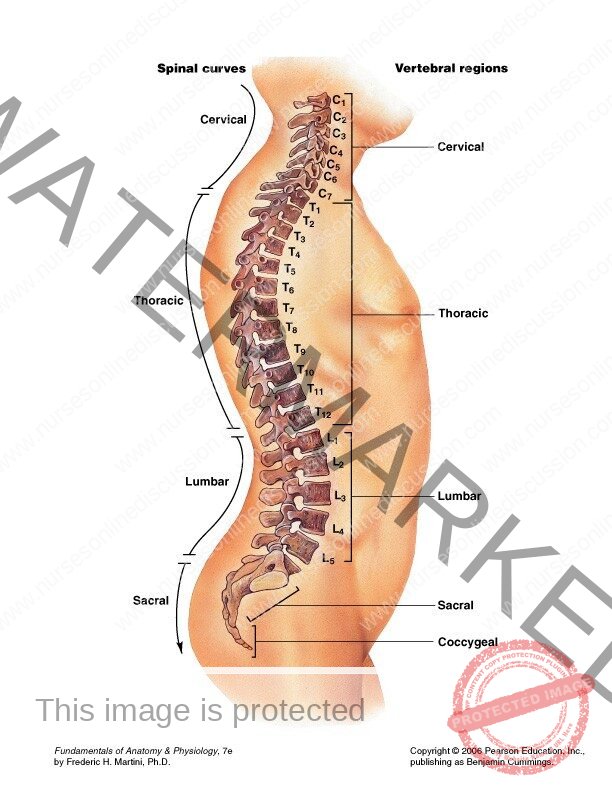
- The human vertebral column (back one) or spine of the human skeleton consisting of 24 articulating verterbra and a fusal vertebra in the sacrum and coecyx.
- The vertebia column protects the spinal cord. They are normally 33 vertebra.
- The upper 24 are articulating and separated from each other by the intervetebra discuss and the lower are fused in adults, five in the sacrum and in the coccyx. (tailbone).
Characteristics of a typical vertebra
It must have a body and neural arch.
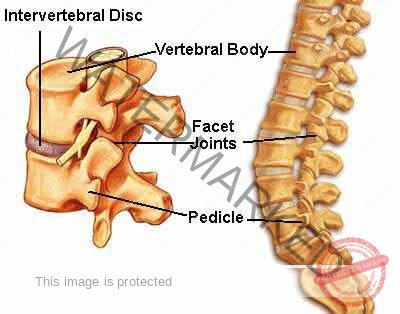
BODY
- It is broad flattened largest part of the vertebra.
- It is the flatteted surfaces of the body of each vertebra that articulates with corresponding surfaces of adjacent verterbia.
- No direct contact of the vertebra. There is a tough pad of fibrocartilage called intervertebral discs.
- Bodies of the vertebra lie to the front of the vertebral column increasing greatly in size towards the base of the spine as the lower spine has to support much weight than the upper part.
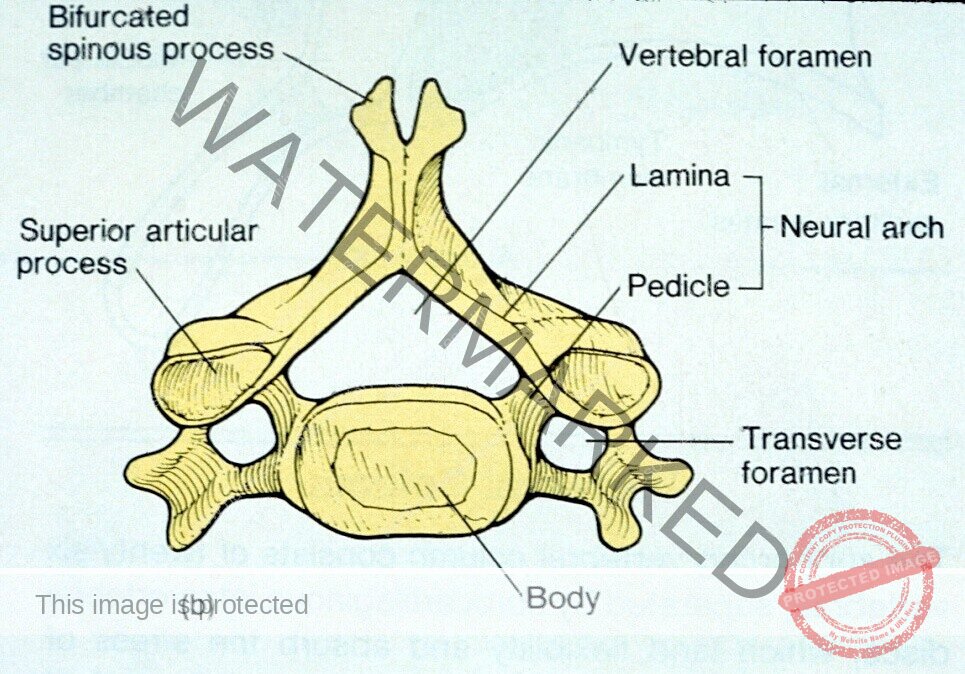
VERTEBRAL (NEURAL) ARCH
- This encloses a large vertebra foramina. It lies behind the body, forming posterior and lateral walls of lateral foramina. Lateral walls are formed from plates of bones called pedicles and the posterior walls are formed from lamina.
- Projecting from the region where the pedicles meet the lamina is the transverse processes and where the two lamina meet at the back is the process called the spinous process. These prominences can be felt through the skin along the length of the spine. The vertebral foramen form the vertebral neural canal that contains the spinal cord.
Diagram
THE CERVICAL VERTEBRA (Vertebra)
- They are the smallest vertebra. the transverse processes have a farmen through which the vertebral artery passes up to the brain. It has vertebra. The first two cervical vertebra are; Atlas & Axis.
- The first cervical vertebra is the Atlast and is the bone where the skull rests. The second cervical bone is the axis where the skull turns. The atlas has some short traverse process.
- It posses 2 flattened facets that articulate with the occipital bone to form a joint that permits nodding of the head.
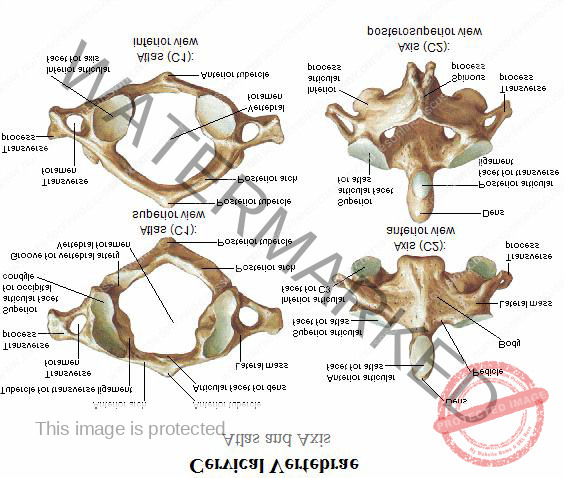
Axis : The axis sits below the atlas and has a small body with a superior projection called for odontoid process also called dens (tooth). This occupies part of the posterior foramen of the atlas and its held secretly by the transuense ligaments. The head pivots (turns side to side( on this joint. The seventh cervical vertebrae is the vertebra prominens which is easily felt at the base of the neck.
LUMBAR VERTEBRA: It’s the largest of the vertebra. This is because they have to support the weight of the upper body, They have substancial spinous processes for attachment of muscles of the lower back.
Diagram
SACRUM: It consists of 5 rudimentary fused vertebra which forms a triangular or wedge shaped bone with a concave anterior surface.
The upper part or base articulates with the fifth lumber vertebra on each side it articulates with the illium to form the sacroiliac joint. The inferior part articulates with eh coccyx.
The anterior edge of the base (promotary) protrudes into the pelvic cavity. It has vertebra foramina for the passage of blood vessels and nerves.
COCCYX: It consists of four (4) fused terminal vertebra to form a very small triangular bone. The broad base articulates with the tip of the sacrum.
FEATURES OF THE VERTEBRA COLUMN
Intervertebral discs
- Bodies of adjacent vertebral are separated by intervetebral discs consisting of fibro cartilage.
- thinnest in the cervical and progressively thicker towards the lumbar region as spinal loading increases.
- They are kept in place by the posterior longitudinal ligament.
- They act as shock absorbers.
- Fibrocartilage form cartilaginous joint which contribute to flexibility of the vertebra column as a whole.
Intervertebral foramen
When the vertebra are viewed seen from a side aforamen formed by the gap between the pedicles can be seen.
There is intervertebra foramina on each side between every pair of vertebri through which the spinal nerves, blood vessels and lymph vessels.
Ligaments of the vertebia column
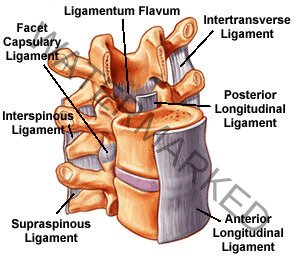
These hold the vertebia together and keep the cartilaginous joint in position.
Transverse ligaments
- The transverse keep the ondotoid process in correct position in relation to atlas.
- Anterior longitudinal ligament: The moves the whole length of the vertebral column and lies infront of the vertebra.
- Posterior longitudinal ligament: This lies inside the vertebral canal and in close contact with the posterior surface of the bodies of the vertebra.
- Supra spinous ligament : This connect the spinous process from the occinut to the sacrum.
Curves of the vertebra
When viewed from the side the vertebra column presents for curves. Two primary, and Two secondary curves; The fetus in the uterus lies curved so that the head and knees are more less toughing this shows the primary curvature. When a child can hold up his head ( after about 3 months).
The first secondary cervical curve develops. And when a child can stand up right (around 12-15 months) the second any lumber curve. The thoracic and sacral curvature is maintained hence the two primary curves. Primary curves : Thoracic , and Socral
Secondary curves: Cervical (1st), Lumbar (2nd)
Movement of the vertebral column
- Movement between bones of the vertebra is limited some movements include:-
- Flexion (bending forward)
- Extension (bending backward)
- Lateral flexion (bending aside)
- Rotation (turning round)
NB More movement is in cervical and lumbar region.
function of the vertebral column
- The vertebral canal gives strong protection for the delicate spinal cord.
- The intervertebral foramina provides passage for spinal nerves, blood vessels, lymph vessels.
- The supports the skull
- Intervertebral discs act as shock absorbers protecting the brain.
- It forms the axis of the trunk giving attachment for ribs, shoulder, girdle and limbs, pelvic girdle and lower limbs.
- The numerous individual bones with other intervebral discs allow movement of the whole column.
THORAX
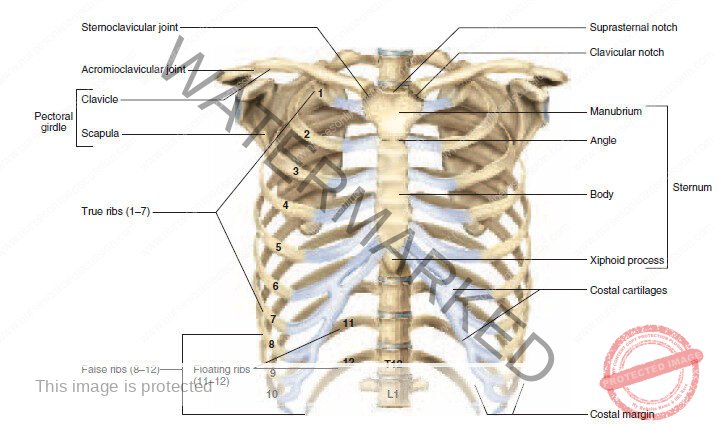
- This refers to the chest.
- It is a bony cage formed by sternum, ribs, coastal cartilage , bodies of the thoracic vertebra.
STERUM (Breast bone):
It is a flat narrow born measuring about 15cm (6 inch) located in the median line of the anterior thoracic wall. It consists of three basic portions
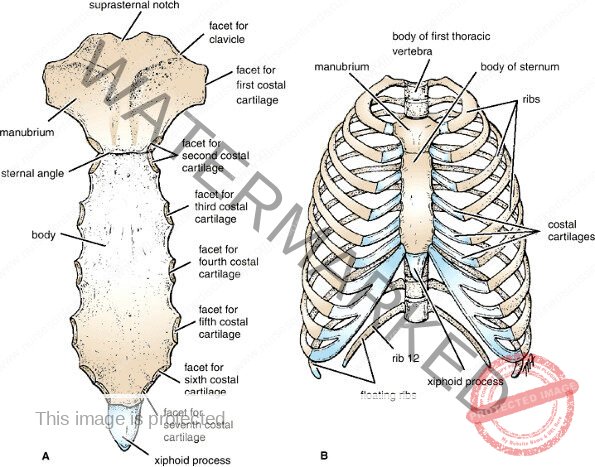
- The manubrium (superior portion)
- The body (middle and largest portion)
- Xiphoid process (inferior and smallest portion)
The junction of the manubrium and the body forms the sterna angle.The manubrium on its superior portion has a depression called Jugular (suprasternal notch). On each side of the jugular notch are clavicular notch that articulates with first and second ribs. The body of the sternum articulates directly or indirectly with the 2nd to 10th rib.
The xiphoid process consists of hyaline cartilage during infancy and childhood and do not ossify completely up-to the age of 40.
Diagram
RIBS
- Human being contain 12 pairs of ribs that make up the side of the thoracic cavity.
- Ribs increase in length from 1st to the 7th and they decrease in length to the 12th .
- Each rib posteriorly articulates with the body of its corresponding thoracic vertebra.
- Anterioly the first of ribs have direct attachment to sternum by coastal cartilage hence they are called true ribs (vertebra-sternal ribs)
- The remaining three ribs are called false ribs. The 8th, 9th, 10th ribs are the false ribs (vertebral- chondrial ribs) because their cartilage attach one another and then attach their cartilage to the 7th rib.
- The 11th and 12th ribs are disgnated as floating ribs because their anterior part doesn’t even attach tough indirectly to the sternum.
Diagram
APPENDICULAR SKELETON
It consists of the shoulder girdle and the pelvic girdle.
The shoulder girdles and upper limbs: 2 upper limbs ( extremities), 2 clavide collar bone), 2 scapulae humerous (1), Radius (1), ulna(1) wrist (caupal) (8), metacarpal s (5), phalanges (14_. Total 32 bones.
- The lower limbs consists of the femur (s), fibula (1), tibia (1) , Patella (1), Tarsal (7), metatarsal (s) phallnges (15) total 30 bones
- Two innominate bones (2)
- The total bones of the appendicular skeleton are 128 bones.
- The pelvic girdle has two innominate bones consisting of the illium, ischium, and pubis.
SHOULDER GIRDLE (Pectoral)
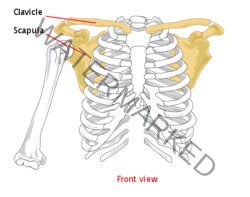
Clavicle (collar bone)
They are two in number.
- Double curved long bone with rounded medial end and flattened lateral bone. It isS-shaped.
It is held in place by ligaments - It holds shoulder joints and arm away from the thorax so that the upper limb can swing freely.
- It articulates with the manubrium of the sternum at the sternol- clavicular joint and also articulates with the acromion process of the scapula to farm the acromic- clavicular joint.
- It allows the upper arm to move freely.
- It is the only attachment/bony link of the appendicular skeleton to the axial skeleton.
Scapula/shoulder blade
They are two in number
- It is a flat triangular bone with a horizontal spine separating fossa. It is a site for attachment of the muscles of the arm.
- At the lateral angel is a shallow articular surface the glenoid cavity which articulates with the head of the humerous to form the shoulder joint.
- The prominence which can be felt through the skin is called the acromion process which articulates with the claucle to form acromio clavicular joint. (Synoval joint).
- A slight movable joint that contributes to the mobility of the shoulder girdle. It has also the coracoid rocess for attachment of muscles of the shoulder.
Diagram
Humerous
They are two in number.
- It is the longest bone of the upper limb.
- It forms ball and socket joint with the glenoid fossea of the scapula.
- It is a site of attachment of muscles of the shoulder and arm permitting the arm to flex, extend.
- At the distal and of the head are two roughened projections of the bone that is , greater and lesser tubercles and in between them is a deep groove Bicipital glove. (intertubercular sulcus). This is occupied by the tendon of the biceps muscle. At the distal end of the bone presents two round/smooth surfaces which articulate with the Radius and Ulna to form the elbow joint.
Diagram
Fore arm (Ulna & Radius)
Shoulder girdle
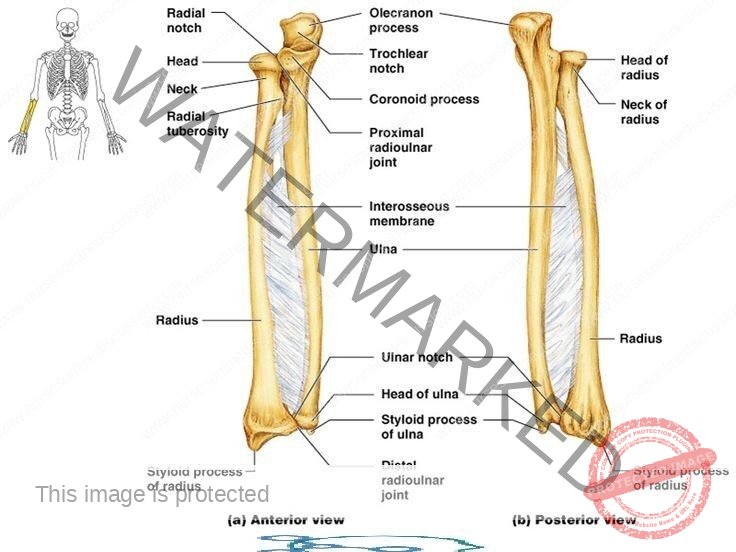
- It is composed of two bones i.e. Radius and Ulna. Radius is larger of the two bones. But ulna is longer . Ulna has olacranon process which is the prominence of elbow. The two bone articulates with the humerous at the elbow to form elbow joint.
- Wrist joint: The two bones articulate with each other at the proximal end to form. Radio ulna joint.
Wrist (carpel bones)
They are firmly held together by ligaments that allow little or slight movement between them. The bones of the proximal low form part of the wrist joint while those of the distal row articulate with the metacarpal bones forming distal carpal metacarpular joint.
Palm (Metacarpel) bones
- They are five bones in each side.
- They are numbered from the thumb side in wards.
- The proximal end articulates with the carpel bone forming carpal metarcapular joint.
- Carpal metarcapular joint.
Function
The joint aid in cupping of the hand.
Phalanges
They are 14 in number and they articulate with each other at the interphalangeal joint and this allows fingers to participate in stable grips.
Diagram
PELVIC GIRDLE
It is formed by two innominate hip bones. Pelvis is the term given to the basin shaped structure formed by the two innominate bone , sacrum and coccyx.
Innominate bones
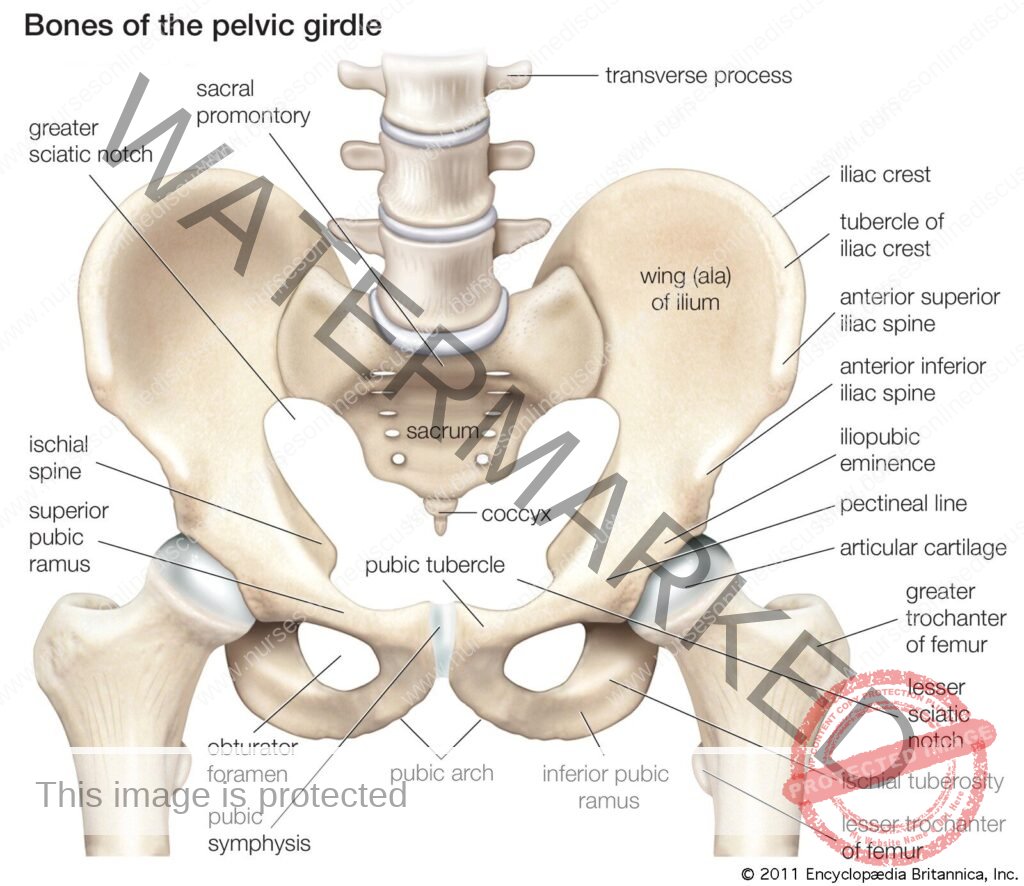
- These are formed by three fused bones that is:- Illium, ischium, publis
- On it is lateral surface, it has a depression which is the acetabulum which articulates with head of the femur to form Hip joint.
Ilium: articulates with the sacrum
Upper flattened part of the bone which presents the iliac crest. It forms the synovial joint with the sacrum (sacro-iliac joint ). A strong joint capable of absorbing stressed of body weight.
- It tends to become fibrosed in latter life.
Pubis
- It is the anterior part of the bone.
- It articulates with each other at a cartilaginous joint, the symphysis pubis.
Ischium
- This forms the inferior and posterior part of the bone. It presents with rough inferior projections, the ischial tuberosities which bear the weight of the body when seated.
PELVIS
- It is divided into upper and lower parts . (Brim of the pelvis). It consists of : prometary of the sacrum.
- Ileopectineal line.
- The greater or false pelvis is above the brim and lesser or true pelvis is below the brim.
Difference between male and female pelvis
Male Female
- Bones are heavier Bones are lighter
- Pelvis is smaller Pelvis is wider
- Triangular shaped Rectangular shaped
- Less shallower More shallow
- Triangular shaped Rounded
- Not roomier Roomier generally
The shape of the female pelvis allows for the passage of the baby during child birth.
Thigh/FEMUR BONE
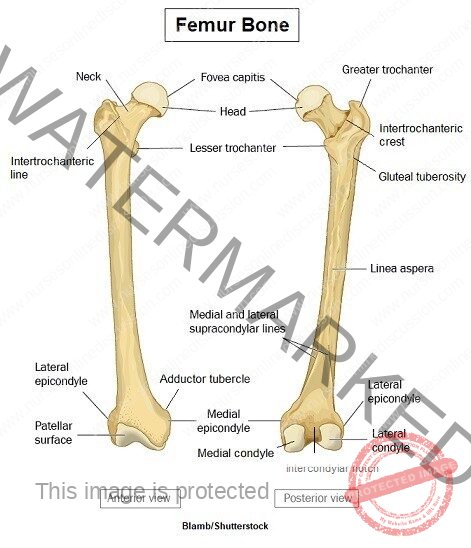
- This is a typical long bone
- It is the longest, strongest, heaviest bone.
- It has a spherical head that articulates with the acetabulum of the hip bone to form the hip joint which is a Ball & Socket Joint. It has greater and lesser trochanter for attachment of muscles.
- At the lower extremities it has two condyles that is Medial and lateral condlles which with tibia and patella form the knee joint
- Function: To support the body.
Leg/TIBIA & FIBULA
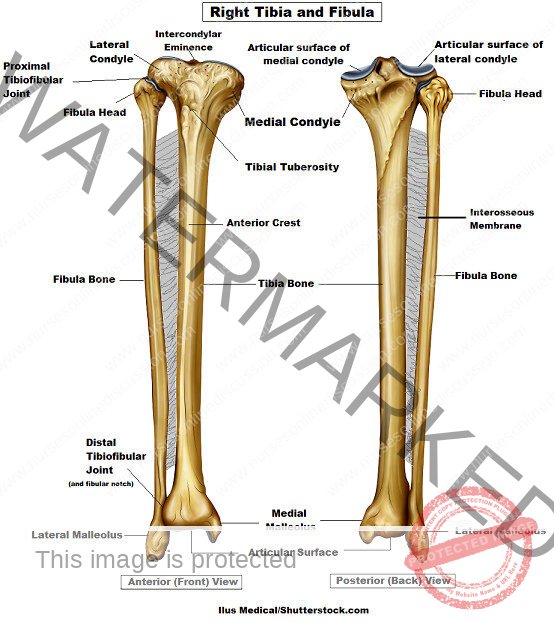
- Tibia which participates in forming both the knee and ankle joints.
- At the proximal end presents two condyles for articulation with the femur to form the knee joint.
- The head of the tibula articulates with the inferior aspect of the lateral condyle of the Tibia bone farming proximal tibiofibula joint.
- At the distal and the Tibia forms the ankle joint with the falus and fibula.
Fibula:
- It is a long slender lateral bone of the leg.
- Its head articulates with the lateral condyle of the tibia to form the proximal tibiofibula joint and the lower extremely articulates with the tibia and projects beyond it to form the lateral malleolus.
- This helps to stabilize the ankle joint.
Diagram
Arches of the foot
- Medial longitudinal arch
- Trasverse arch
- Lateral longitudinal arch
- The foot is supported by three arches that distribute body weight to the heel and ball of the foot.
- Avoid damage of blood vessels and nerves
- Increase on stability.
Patella (knee cap)
- It is a roughly triangular shaped sesmoid bone associated with the knee joint.
- Its posterior surface articulates with the patellar surface of the knee joint and its anterior surface is in the patella, tendon, i.e. the tendon of the quardriceps famoris muscle.
Tarsal (ankle) bones
- The seven tarsal bones forming the posterior part of the foot ( ankle) and three cuneiform bones. The talus articulates with the tibia and fibula at the ankle joint. The calcaneus forms the heel of the foot. The other bones articulate with each other and with the metatarsal bones.
Metatarsal (bones of the foot)
- They are five bones, numbered from inside out, which form the greater part of the dorsum (sole) of the foot. At their proximal ends they articulate with the tarsal bones and at the distal end with the phalanges. The enlarged distal head of the 1st metatarsal bone forms the ball of the foot.
Phalanges (toe bones)
- They are 14 phalanges arranged in a similar manner to those in the fingers ie
- Two in the great toe ( the hallux)
- Three in each of the other toes.
Arches of the foot
- The arrangement of bones in the foot, supported by associated ligaments and action of associated muscles, gives the sole of the foot an arched or curved shape. The curve running from head to toe is called the longitudinal arch and the curve cross the foot is called the transverse arch.
Questions
1)Identify the bones forming the appendicular skeleton.
- State the characteristics of bones forming the appendicular skeleton.
- Outline the differences in structures between the male and female pelvis
2) State the functions of bones
- List five types of bones and give an example of each.
- Outline the general structure of along bone.
- Describe the structure of compact and spongy bone tissue
- Describe the development of bone.
- Explain the process of bone healing and the factors that complicate it.
- Outline the factors that determine bone growth.
3) Identify the bones of the skull ( face and cranium)
- List the functions of the sinuses and fontanelles of the skull.
- Outline the characteristics of a typical vertebra.
- Describe the structure of the vertebral column.
- Explain the movements and functions of the vertebral column.
- Identify the bones forming the thoraric cage.
JOINTS
Draw all necessary diagrams
Classification of joints
- FIBROUS JOINTS: These are made of fibrous connective tissue which unites articulating bones. There is no joint cavity, Mostly are immovable and some are slightly movable.
- Examples; Cranial sutures, Inferior tibio fibula joint, Interosseus ligament , Roots of teeth in Alveolar processes of mandible and maxilla.
CARTILAGENOUS JOINTS
- The articulating bones are united by a plate of hyaline cartilage or fibrocartilage nous disc mostly slightly movable but some immovable.
- Examples; Symphysis pubis , Intervertebral disc
SYNOVIAL JOINTS
- Articulating bones move freely along smooth lubricated articular cartilage which is enclosed within a flex capsule.
Diagram
CHARACTERISTIC OF SYNOVIAL JOINTS
Articular/hyaline cartilage
- This provides smooth articular surface forces and bear the weight of the body.
- Its about 7mm thick in young people and becomes thinner and less compressible with age and thus increase stress on the other structures of the bone.
- Cartilage has no blood supply. It only receives its nourishment from synovial fluid.
Capsular ligament
- It is a sleeve of fibrous tissue which holds bones together. Its loose to allow freedom of moment but strong enough to protect it from any injury.
Synovial membrane
- It has epithelial layer which lines the capsule and it secrets synovial fluid.
Synovial fluid
It is a thick sticky fluid of egg white consistence that fill the synovial cavity.
Functions of synovial fluid
- Maintains bone structure.
- Nourishes structures within the cavity.
- It contains phagocytes which remove microbes and cellular debris.
- Acts as a lubricant
- Maintains joint stability
- Prevents ends of bones from being separated does a little water btn the glasses.
- Some little sacs of synoval fluid (bursae) are present in some joints eg the knee joint and they act as cushions to prevent friction between abone and aligament or tendon or skin where the bone is near the surface.
- Extra capsular structures: Examples:- tendons , Ligaments , Muscles , Nerve and blood supply
- The blood and nerve supply is usually to the capsule and to muscles that move it.
Movement possible at synovial joint.
- Flexion (bending usually forward
- Extension (straightening or bending backwards)
- Abduction (movement away from the midline of the body)
- Adduction (movement towards the midline)
- Circumduction (movement of the limb or digit so that it describes the shape of a cone.
- Rotation (Movement along the axis of above)
- Pronation (turning the palm of the hand upwards)
- Supination (Turning the side of the foot inwards)
- Inversion ( turning the sole of the foot inwards)
- Eversion (Turning the sole of the foot outwards)
TYPES OF SYNOVIAL JOINTS
1)Ball and socket joint
- The head of one bone is ball shaped and articulates with a cup shaped socket of another.
- It allows for a wide range of movement like extension, flexion, abduction, abduction
- Examples include; Shoulder joint , Hip joint
2) Hinge Joint
Articulating ends of the bones form an arrangement like a hinge on a door and movement is restricted to extension and flexion eg Elbow joint. Interphalangaeal joint, Knee joint
3) Gliding joints : Articular surfaces are that or very slightly curved and glind over one another but movement is restricted. Its the only least movable joint of the synovial joint.
Examples ; Joints between the carpal bones in the wrist, Tarsal bones in the foot.
4)Pivot joint: Allow a bone or limb to rotate.
Example; The head rotates on the pivot joint formed by the dens of the axis held within the ring of the atlas by transverse ligament and the ondotoid process of the axis.
- Candyloid joints: A condyle is a smooth rounded projection on a bone and in a condyloid It sits within a cupshaped depression on the other bone. Eg – A joint btn the condyle process of the mandible and the temporal bone, Btn metacarpal and phalanges , Metatarsal and phalonges of the foot.
5) Saddle joint: The articulating bones fit together like a man sitting on a saddle.
Example- Base of the thumb between the trapezium to the wrist bones and the first metacarpal bones.
- Ability to touch each of the finger tips on the same hand is due to the nature of the thumb joint.
SHOULDER JOINT
- It is a ball and socket joint.
- It is the most movable/mobile in the body and least stable and therefore easily to dislocation especially in children
- It is formed by glenoid cavity of the scapula and the head of the humerous and is well padded with a protective bursae.
- Glenoid cavity is deepened by a rim of fibro cartilage and is called Glenoidal labrum which provides additional stability without limiting movement.
- The joint is stabilized by a number of ligaments ie Gleno humeral transverse. Also muscles with their tendons
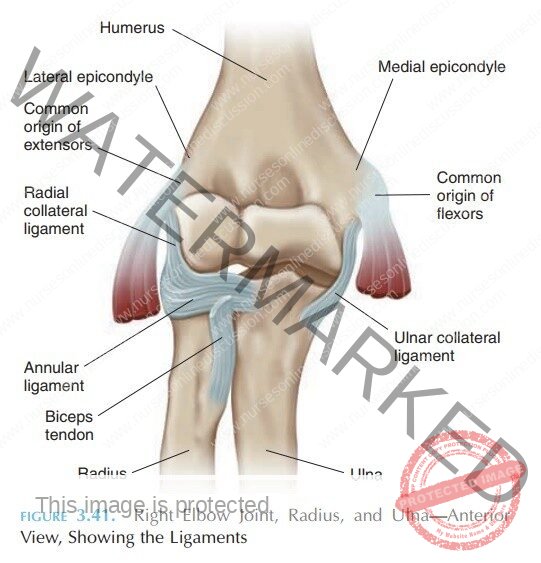
This is formed by Trochlea and capitulum of the humerous then trochlear notch of the ulna and head of the radius. Its extremely a stable joint because the humeral and ulna surfaces interalock and the capsule is strong. It has anterior, posterior, medial and lateral strengthening ligaments for stability.
Diagrams
Proximal and distal radioulnar joints
- It is a pivot joint (proximal radioulnar joint) and distal.
- It is formed by the rim of the head of the radius rotating in the radial notch of the ulna.
- It forms the same- capsule as the elbow joint.
- The annular ligament is a strong extra capsular ligament that encircles the head of the radius and keeps it in contact with the radial notch of the ulna.
- The interasseous membrane (fibrous membrane) links the bones along their shafts and prevents separation of the bones when force is applied at either end ie at the wrist or elbow.
Muscles and movements
- The fore arm may be pronated (turned palm down) or supinated (turned palm up)
- Pronation is caused by the action of the pronator teres , supination is by action of supinator and biceps muscles.
Wrist joint
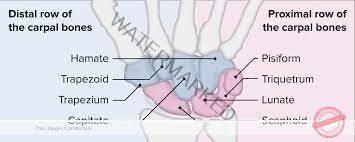
- It is a condyloid joint formed between the distal end of the radius and the proximal end of the proximal carpals, ie the scaphoid, lunate and friquetrum.
- A disc of white fibrocartilage separates the ulna from the joint cavity and articulates with the carpal bones. It also seperates the inferior radiolnar joint from the wrist joint.
- Extracapsular structures consist of medial and lateral ligaments and anterior and posterior radiocorpal ligaments.
- It can be flexed, extended, abducted, adducted.
Diagram
Joints of the hands and fingers
- There are synovial joints between the carpal bones, between the carpal and metacarpal bones, between the metacarpal bones and proximal phalanges and between the phalanges.
- Movement of the joints of the hand and fingers is controlled by muscles in the fore arm and smaller muscles within the hand. There are no muscles in the fingers, finger movements are produced by tendons extending from muscles in the fore arm and the hand.
- The joint of the base of athumb is a saddle joint unlike the corresponding joints of the other fingers, which are condyloid. This means that the thumb is more mobile than the fingers and the thumb can be flexed, extended circumducted, adbucted and adducted. In addition the palm can be moved across the palm to touch the tips of each of the fingers on the same hand (opposition), giving great manual dexterity and allowing eg the holding of a pen and the fine manipulation of objects held in the hand.
- The joints between the metacarpals and finger bones allow movement of the fingers. The fingers may be flexed, extended adducted, abducted and circumducted with the first finger more flexible joints (interphallangeal joints) are hinge joint and allow flexion and extension.
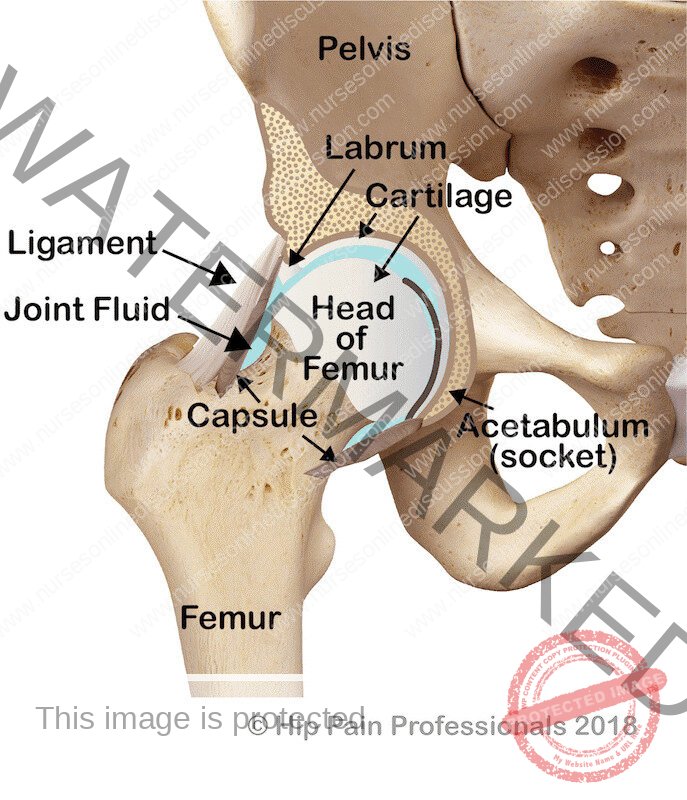
HIP JOINTS
- It is a ball and socket joint
- It is formed by the cup- shaped acetabulum of the innominate (hip) bone and the almost spherical head of the femur.
- The capsular ligament encloses the head and most of the neck of the femur.
- The cavity is deepened by the acetabulum labrum, a ring of fibro-cartilage attached to the rim of the acetabulum which stabilizes the joint without limiting its range of movement.
- It is a steady and powerful joint, since it bears all body weight when standing. It is stabilized by its muscuclature, but its ligaments are also important.
- The three main external ligaments are; Iliofemoral, Pubofemoral, Ischiofemoral
KNEE JOINT
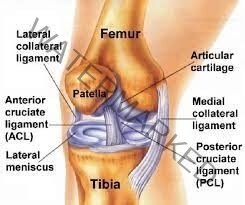
- This is the body’s largest and most complex joint .
- It is a hinge joint formed y the candyles of the femur, the tibia condyles and the posterior surface of the patella.
- The anterior part of the capsule is formed by the tendon of the quadriceps femoris muscle which also supports the patella.
- Intracapsular structures include ; Two cruciate ligaments , Semilunar cartilages (menisci)
- Two cruciate ligaments that cross each other, extending from the intercondylar notch of the femur to the intercondlar eminence of the tibia. They help to stabilize the joint.
- Semilunar cartilages or Menisci are incomplete discs of fibrocartilage lying on top of the articular condyles of the tibia. They are wedge shaped, being thicker at their outer edges and provide stability. They prevent lateral displacement of bones and cushion the moving joint by shifting within the joint space according to the relative positions of the articulating bones. Bursae and pads of fat are numerous. They prevent friction between a bone and aligament or tendon between the skin and the patella.
- Synovial membrane covers the cruciate ligaments and the pads of fat. The menisci are not covered with synovial membrane because they are weight bearing.
- External ligaments provide further support, making it a hard joint to dislocate.
- Movements at this joint are:- flexion extension and a rotary movement that ‘locks” the joint when fully extended.
- When the joint is locked it is possible to stand upright for long period of time without tiring the knee extensions.
- Muscles extending the knee:-Quadriceps femoris, Principal flexors; Gastocnemius, Hamstrings
ANKLE JOINT
- It is a hinge joint.
- It is formed by the distal end of the tibia and its Mallelus (Medial Malleolus), the distal end at the fibula lateral malleolus and the tallus.
- Four important ligaments strengthen this joint.
- Deltoid and the anterior, Posterior, Medial ,Lateral
- Movements of inversion and eversion occur between the tarsal bones and not the ankle joint movements.
Diagram

JOINTS OF THE FEET AND TOES
There are a number of synovial joints between the tarsal bones.
- Between the tarsal bones and metatarsal bones.
- Btn the metatarsals and proximal phalanges.
- Between the phalanges.
Movements are produced by muscles in the leg with long tendons that cross the ankle joint and by muscles of the foot. The tendons crossing the ankle joint are wrapped in synovial sheaths and held close to the bones by strong transverse ligaments.
They move smoothly within their sheaths as the joints move. In addition to moving the joints of the first, these muscles support the arches of the foot and help to maintain balance.
Join Our WhatsApp Groups!
Are you a nursing or midwifery student looking for a space to connect, ask questions, share notes, and learn from peers?
Join our WhatsApp discussion groups today!
Join NowWe are a supportive platform dedicated to empowering student nurses and midwives through quality educational resources, career guidance, and a vibrant community. Join us to connect, learn, and grow in your healthcare journey
Quick Links
Our Courses
Legal / Policies
Get in Touch
(+256) 790 036 252
(+256) 748 324 644
Info@nursesonlinediscussion.com
Kampala ,Uganda
© 2025 Nurses online discussion. All Rights Reserved | Design & Developed by Opensigma

